USMLE/COMLEX 1 - Myocardial Infarction Symptoms, Diagnosis, & Treatment
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Myocardial Infarctions: Diagnosis & Treatment tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
Definition & Pathophysiology
1. Myocardial infarction is defined as myocardial injury with ischemia.
2. Results from coronary artery blockage leading to myocardial cell death.
3. Time-dependent process where longer ischemia leads to greater necrosis.
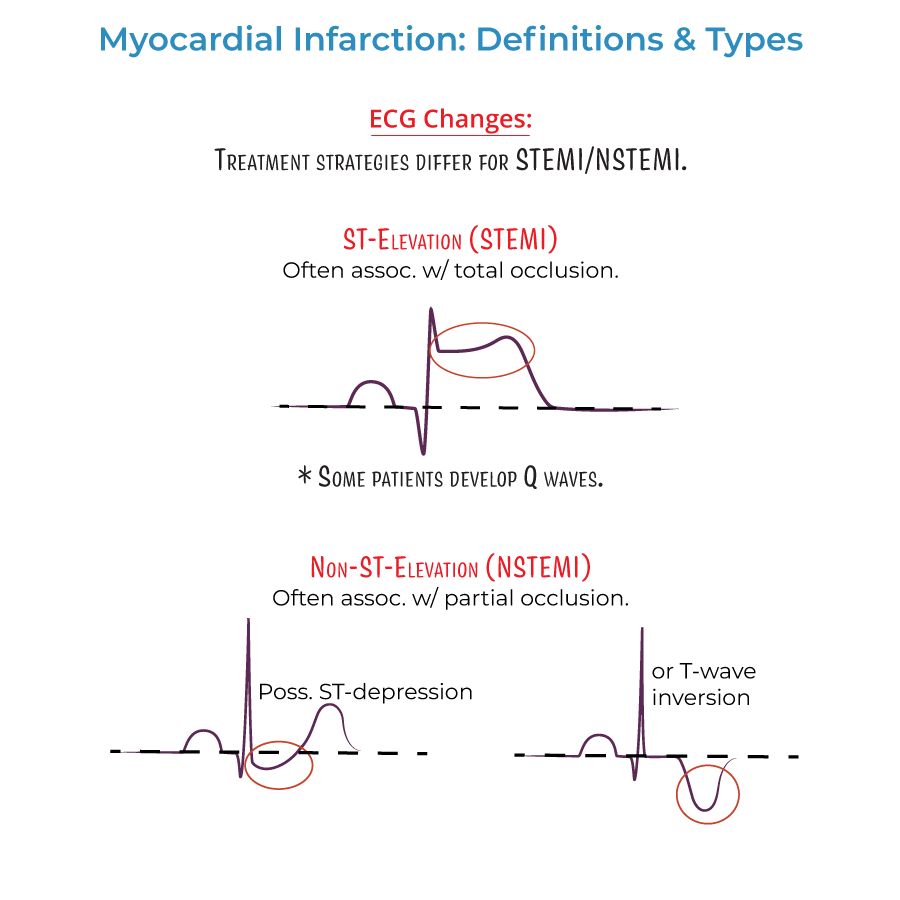
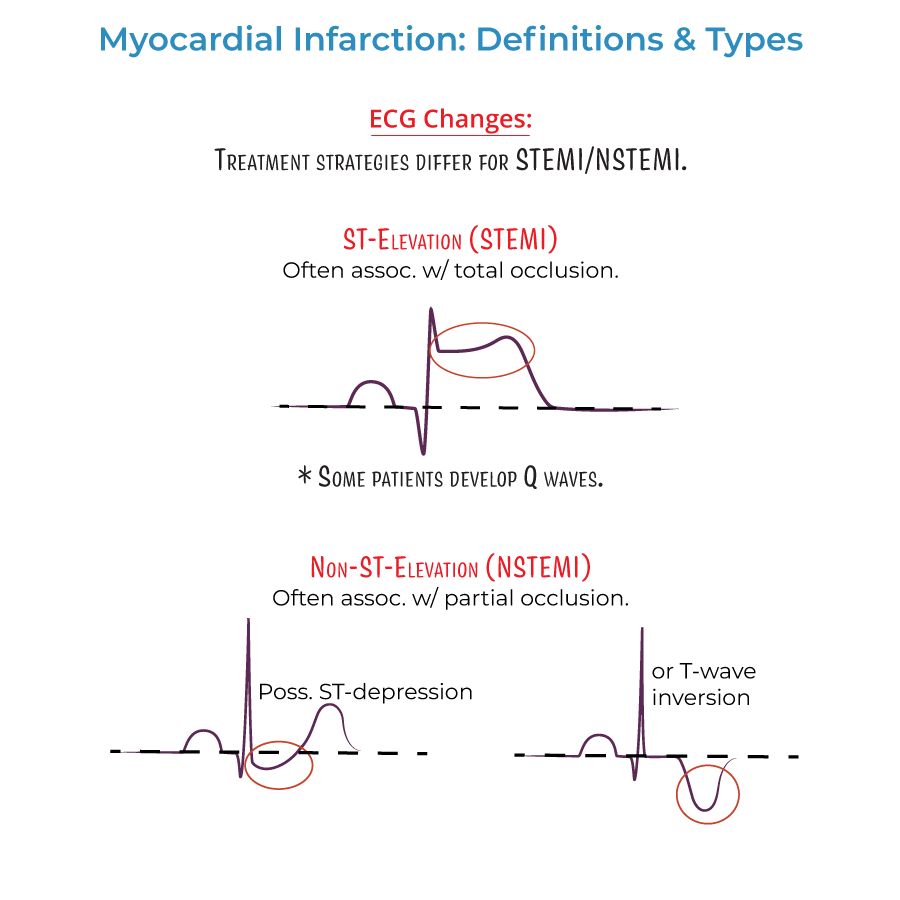
4. STEMI: ST-Elevation Myocardial Infarction - complete coronary occlusion.
5. NSTEMI: Non-ST-Elevation Myocardial Infarction - partial coronary occlusion.
Epidemiology & Risk Factors
1. Geographic distribution: Declining in high-income countries but rising in middle/low-income countries.
2. Demographic patterns: Incidence after age 35, from highest to lowest: Black males > Black females > White males > White females.
3. Age & gender: First MI occurs approximately 10 years earlier in men than women, possibly related to risk factors.
4. Mortality trends: Higher in women, especially young and/or minority women, despite overall declining rates.
5. Major modifiable risk factors: Dyslipidemia, diabetes mellitus, hypertension, smoking (including e-cigarettes), obesity, psychosocial stress, alcohol consumption, poor diet (low in fruits and vegetables).
ECG Findings & Localization
1. ECG timing: Should be performed ASAP when MI is suspected, with serial ECGs to observe infarct evolution.
2. Classification: Distinguishes STEMI from NSTEMI, influencing treatment strategy.
3. Q-waves: May indicate size/location of current MI or evidence of prior MI.
4. Infarct localization by ECG leads:
- Lateral: Leads I and aVL - left circumflex artery
- Apical: Leads V5 and V6 - left circumflex or right coronary arteries
- Anterior: Leads V3 and V4 - left anterior descending artery
- Anteroseptal: Leads V1 and V2 - proximal left anterior descending artery
- Inferior: Leads II, aVF, and III - right coronary artery (90%) or left circumflex (10%)
- Right ventricular: Additional leads V3R-V6R required
- Posterolateral: Additional leads V7-V9 required - right coronary or left circumflex artery
Biomarkers
1. Cardiac troponin: Key diagnostic biomarker, highly specific for myocardial injury.
2. CK-MB: Supports diagnosis, peaks within 24 hours of infarction.
3. Temporal pattern: Both troponin and CK-MB rise after infarction, peak within 24 hours, then gradually decline.
4. Diagnostic utility: Biomarkers help distinguish NSTEMI from unstable angina - only NSTEMI shows rising/falling troponin.
5. Serial measurements: More valuable than single determinations.
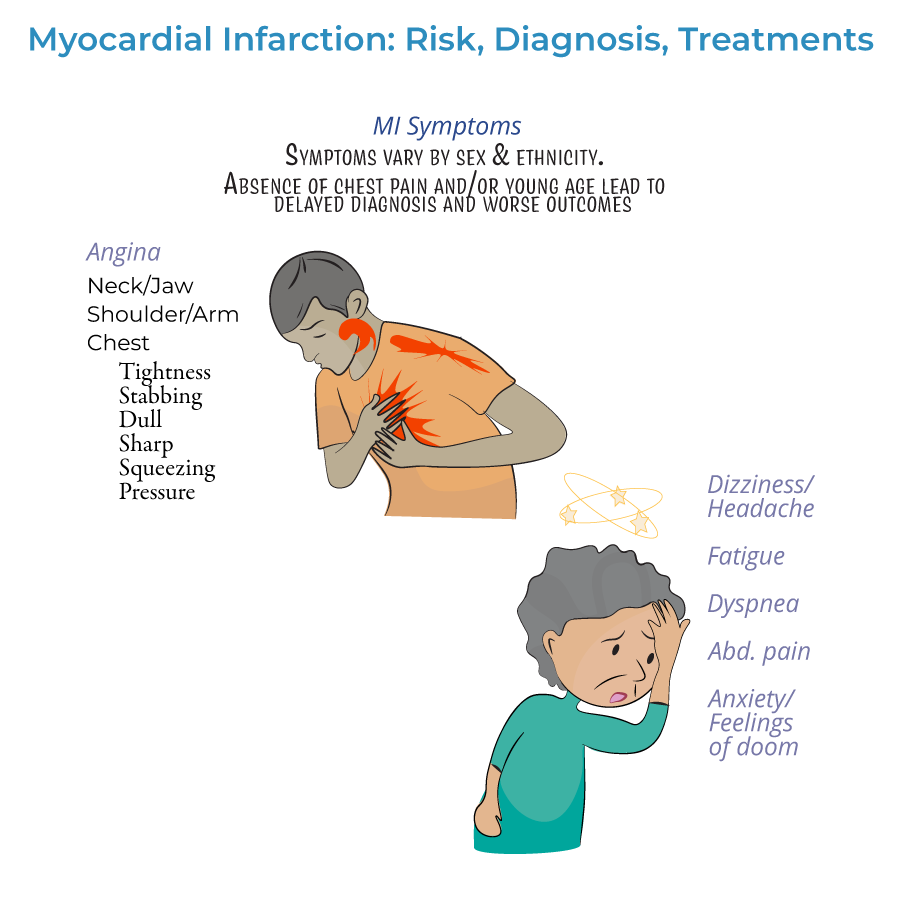
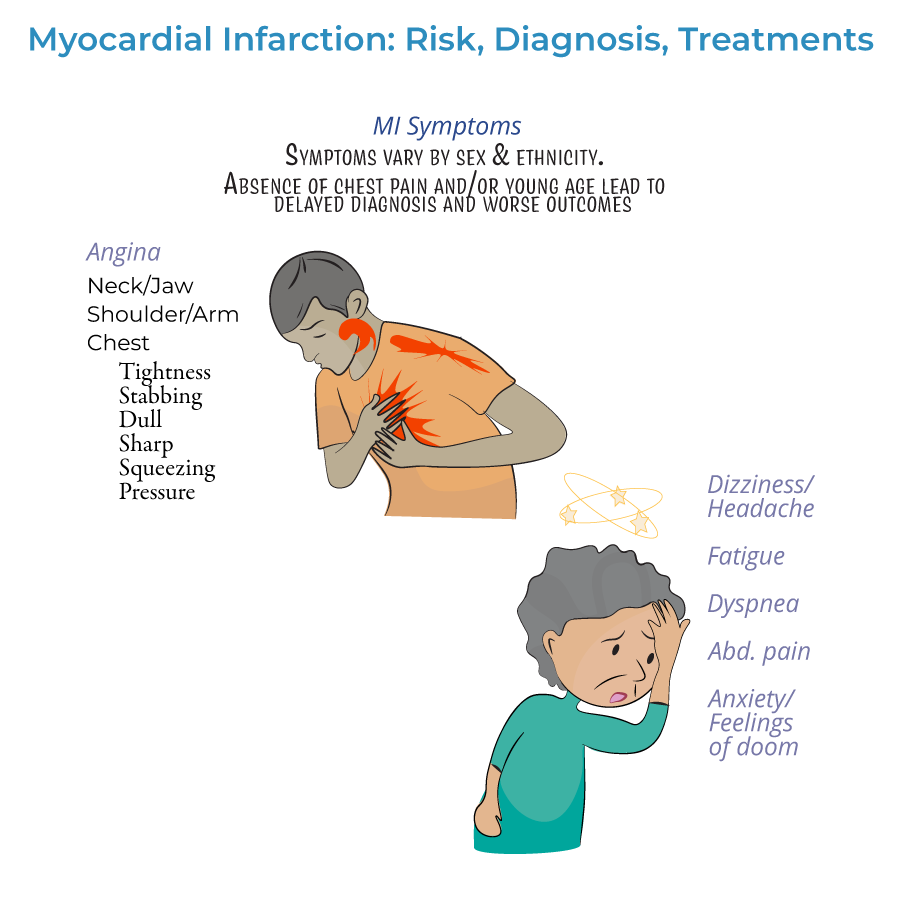
Clinical Presentation
1. Presentation timeline:
- Prodromal: Symptoms days/weeks/months before the acute event
- Acute: Symptoms during the actual infarction
- Silent: No noticeable symptoms (common in diabetics)
- --
HIGH YIELD
ECG Interpretation Pearls
1. ST elevation: Indicates transmural injury with complete coronary occlusion (STEMI).
2. ST depression/T-wave inversion: May indicate subendocardial ischemia (NSTEMI/unstable angina).
3. Q-wave progression: Develops over hours to days after infarction.
4. Reciprocal changes: ST depression in leads opposite to the infarct site.
5. Additional leads: Right ventricular (V3R-V6R) and posterior infarctions (V7-V9) require special lead placement.
Coronary Artery Distribution
1. Left anterior descending (LAD): Supplies anterior wall and anterior septum - abnormalities in V1-V4.
2. Left circumflex (LCx): Supplies lateral wall - abnormalities in I, aVL, V5-V6.
3. Right coronary artery (RCA): Supplies inferior wall and (in 90% of people) right ventricle - abnormalities in II, III, aVF.
4. Dominant circulation: In approximately 10% of the population, left circumflex is dominant rather than RCA.
5. Proximal LAD occlusion: Particularly dangerous, causes anteroseptal MI (leads V1-V2).
Treatment Principles
1. Time sensitivity: "Time is myocardium" - earlier reperfusion leads to better outcomes.
2. Pre-hospital care: Oxygen (if saturation <90%), aspirin, nitrates (morphine if nitrates ineffective).
3. Reperfusion strategies:
- STEMI: Emergency PCI is preferred; if unavailable, immediate fibrinolytics
- NSTEMI: Timing based on risk stratification (immediate for unstable patients)
- Fibrinolytics: Not recommended for NSTEMI (risks outweigh benefits)
- Antiplatelets: Aspirin, clopidogrel, or other P2Y12 inhibitors
- Anticoagulants: Unfractionated or low molecular weight heparin
- Anti-ischemic agents: Beta-blockers or calcium channel blockers
- Plaque stabilization: Statins, ACE inhibitors
Clinical Presentation Variations
1. Gender differences: Women often present with atypical symptoms and have higher mortality rates.
2. Age considerations: Young patients with MI are frequently misdiagnosed due to low clinical suspicion.
3. Prodromal symptoms: May be present for days to months before acute infarction.
4. Silent MI: No noticeable symptoms, often diagnosed incidentally on ECG or imaging.
5. Awareness gap: Many patients, especially women, are unaware of risk factors and symptoms - a significant obstacle to prevention and treatment.
Complications
1. Heart failure: MI is an important cause of heart failure, which is itself a significant cause of death.
2. Mechanical complications: Free wall rupture, ventricular septal rupture, papillary muscle rupture.
3. Electrical complications: Arrhythmias, conduction disturbances.
4. Ischemic complications: Post-infarction angina, reinfarction, infarct extension.
5. Others: Pericarditis, ventricular aneurysm, mural thrombus formation, systemic embolism.
- --
Beyond the Tutorial
Pathophysiology Details
1. Atherosclerotic plaque rupture: Primary mechanism initiating coronary thrombosis and most MIs.
2. Platelet activation cascade: Following plaque rupture, triggers thrombus formation.
3. Ischemic cascade: Progressive cellular changes from reversible (stunning) to irreversible (necrosis).
4. Wavefront phenomenon: Subendocardial-to-epicardial progression of ischemic cell death.
5. Hibernating myocardium: Chronically underperfused but viable myocardium that may recover with revascularization.
Electrophysiologic Changes
1. Action potential alterations: Intracellular K+ loss and Na+/Ca2+ gain during ischemia.
2. Conduction abnormalities: Bundle branch blocks, fascicular blocks, AV blocks.
3. Reperfusion arrhythmias: Accelerated idioventricular rhythm, ventricular tachycardia.
4. Cardiac memory: T-wave changes that persist after resolution of infarct-induced conduction abnormalities.
5. Electrical remodeling: Changes in ion channel expression and distribution following MI.
Complications Pathophysiology
1. Cardiac rupture: Usually occurs 3-5 days post-MI when necrotic tissue is most fragile.
2. Right ventricular infarction: Occurs in 30-50% of inferior MIs, presents with triad of hypotension, clear lungs, elevated JVP.
3. Post-MI pericarditis: Early (2-4 days, fibrinous) vs. late (weeks to months, Dressler syndrome, immune-mediated).
4. Ventricular aneurysm: Outward bulging of thinned, scarred myocardium with paradoxical movement.
5. Papillary muscle dysfunction/rupture: More common in posterolateral MI affecting posteromedial papillary muscle.
Histopathological Timeline
1. 0-6 hours: Minimal visible changes (waviness of fibers at borders), negative TTC staining.
2. 6-12 hours: Coagulation necrosis begins, early neutrophil infiltration.
3. 12-24 hours: Pyknotic nuclei, contraction band necrosis, extensive neutrophil infiltration.
4. 1-3 days: Continued coagulation necrosis, beginning of macrophage infiltration.
5. 7-10 days: Granulation tissue formation with neovascularization and fibroblast proliferation.
6. 2-8 weeks: Collagen deposition, scar formation with reduced cellularity.
Advanced Diagnostic Methods
1. Cardiac MRI: Gold standard for viability assessment, detects edema and microinfarctions.
2. Nuclear imaging: SPECT or PET for perfusion and viability assessment.
3. Echocardiography: Wall motion abnormalities, complications, stress echo for ischemia.
4. Coronary CT angiography: Noninvasive assessment of coronary anatomy.
5. High-sensitivity troponin assays: Enhanced sensitivity for earlier detection of myocardial injury.
