USMLE/COMLEX 1 - Malabsorption Syndromes
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Malabsorption Syndromes tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
General Malabsorption Concepts
1. Malabsorption is the failure to assimilate one or more nutrient types due to defects in digestion, absorption, or transport.
2. Failure is due to: deficient digestive agents (i.e., pancreatic enzymes), abnormal gastrointestinal epithelium, impaired transport, short bowel, or inadequate mixing in the stomach.
3. Signs and symptoms: Diarrhea, steatorrhea, weight loss, weakness, anemia, and vitamin and mineral deficiencies.
4. Malnutrition can lead to musculoskeletal, neurologic, and cardiac complications.
Exocrine Pancreatic Insufficiency (EPI)
1. Causes malabsorption of fats and fat-soluble vitamins (A, D, E, K, and B12) when more than 90% of the pancreatic enzyme function is lost.
2. Top causes: Pancreatitis (often due to excess alcohol consumption in adults), cystic fibrosis (the most common cause in children), and tumors.
3. Signs and symptoms: Loose, bulky, oily, and pale feces that often float because of the oil content.
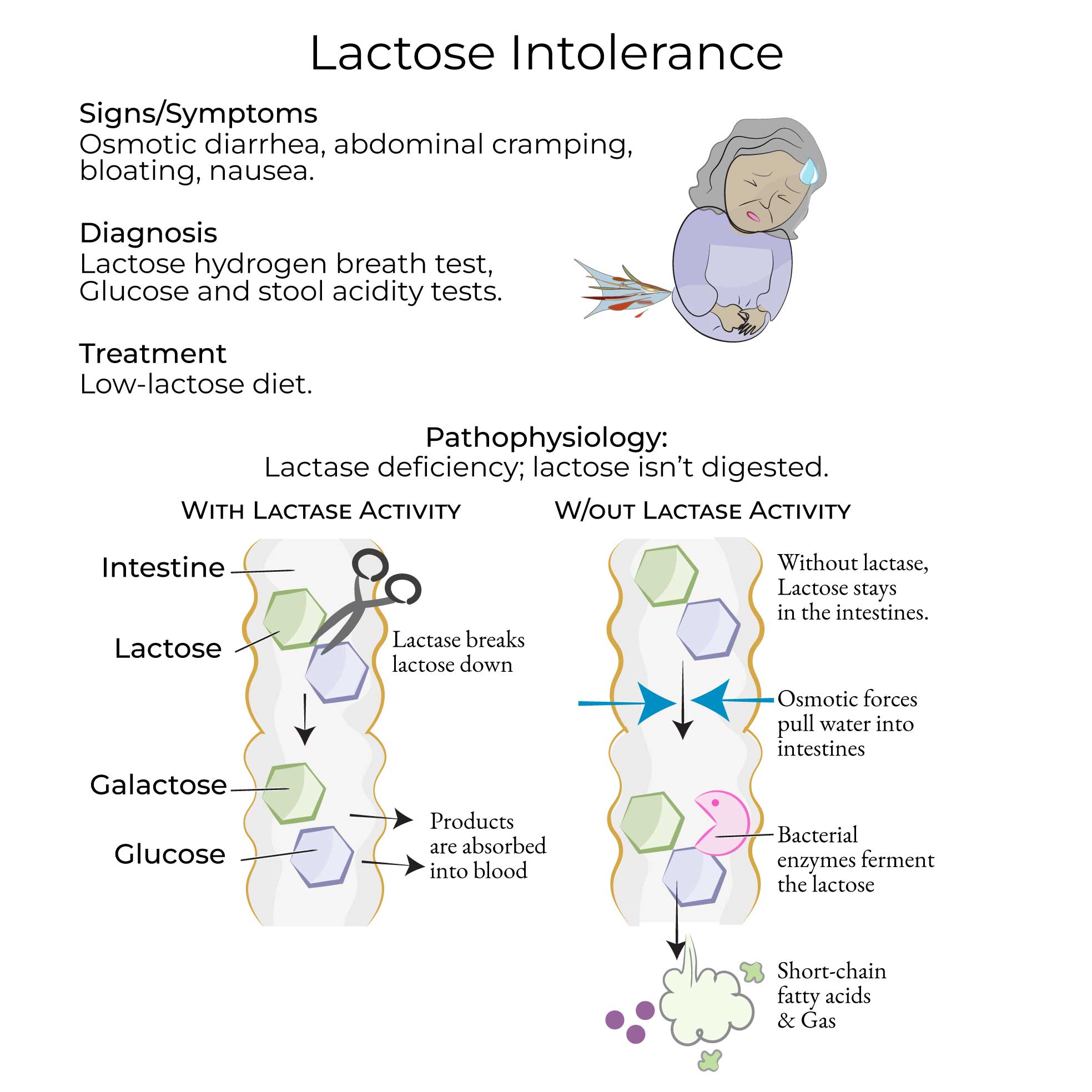
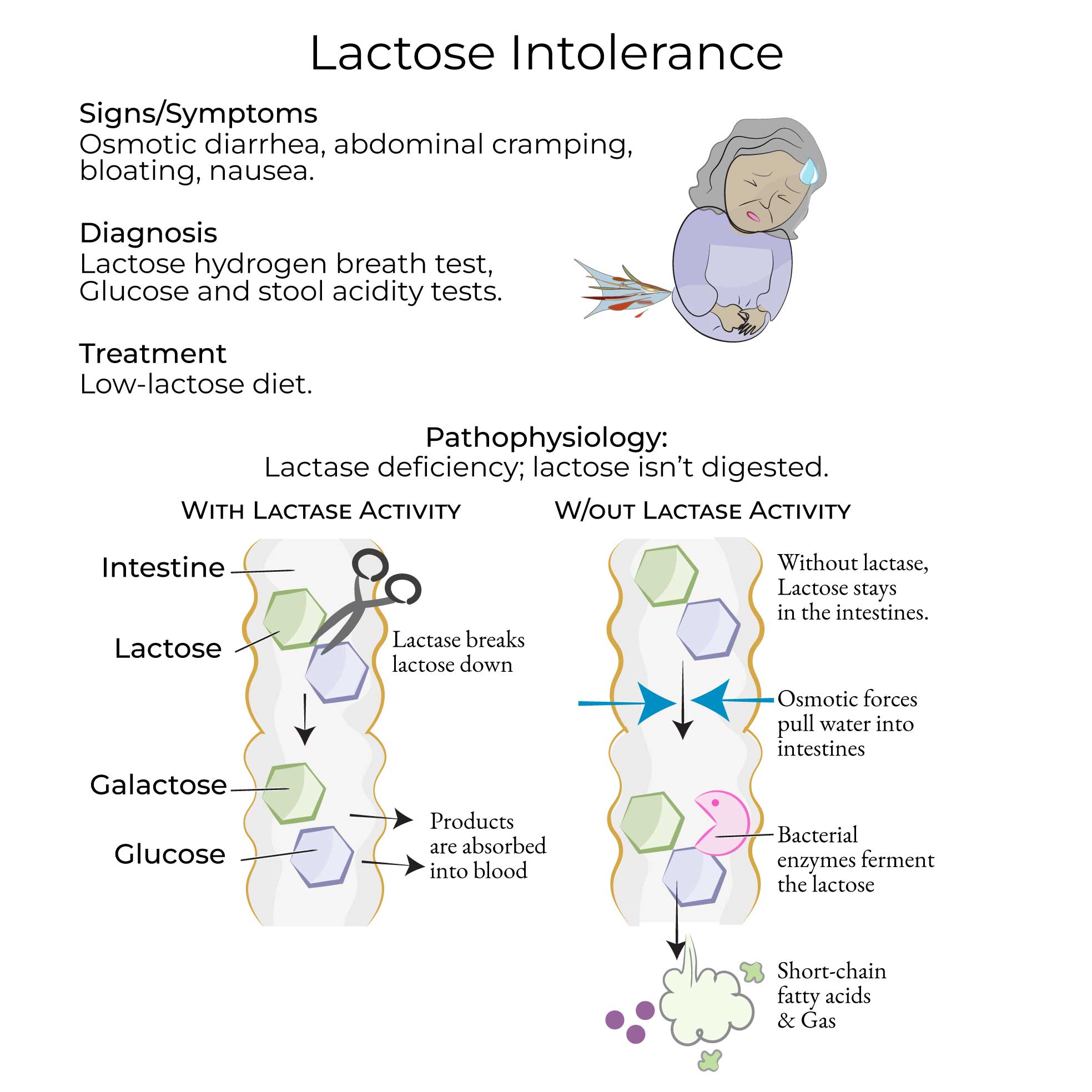
Lactose Intolerance
1. Caused by deficient activity of lactase, which breaks down lactose (a carbohydrate found in dairy products).
2. Types: Congenital lactase deficiency (rare autosomal recessive), primary lactose intolerance (adult-type, common), and secondary lactase deficiency (transient due to intestinal damage).
3. Prevalence varies widely by population: ~30% in Europe, ~50% in United States, ~70% in Asian countries, and nearly 100% in Africa.
Celiac Disease (CD)
1. Autoimmune-mediated inflammatory disorder of the small bowel triggered by gliadin (a gluten protein found in wheat, barley, and rye).
2. Also referred to as gluten-induced enteropathy, non-tropical sprue, and celiac sprue.
3. Affects 1% of US adults.
4. Genetic markers include haplotypes HLA-DQ2 and HLA-DQ8.
Tropical Sprue
1. Rare disorder of uncertain origins (likely infectious or environmental) that occurs in some tropical regions.
2. Characterized by malabsorption of folic acid and Vitamin B12, leading to megaloblastic anemia.
Whipple Disease
1. Rare bacterial disease caused by Tropheryma whipplei (gram-positive, PAS-positive bacilli).
2. Most common in older males of European descent with immune defects.
3. Multisystemic symptoms including arthralgias, neurologic symptoms, endocarditis, and GI effects.
- --
HIGH YIELD
Exocrine Pancreatic Insufficiency (EPI)
1. Carbohydrate and protein digestion and absorption are typically maintained by amylase and protease secreted by other organs (salivary glands, stomach, small intestine).
2. Patients with pancreatitis have pain that starts in the left epigastric area and radiates to the back.
3. Diagnosis: Reduced duodenal pH and fecal elastase-1 (FE-1), an enzyme marker of pancreatic secretion.
4. Treatment: Lifestyle modifications (alcohol cessation), vitamin supplements, and exogenous pancreatic enzyme administration.
Lactose Intolerance
1. Pathophysiology: In the absence of lactase, undigested lactose pulls water into the intestines causing osmotic diarrhea, and bacterial enzymes ferment lactose producing short-chain fatty acids and gas.
2. Diagnosis: Hydrogen breath test (increase >20 ppm above baseline indicates lactase deficiency), blood glucose tests, DNA tests, and stool acidity tests.
3. Secondary lactase deficiency shows damaged intestinal villi, whereas primary lactose intolerance has normal-appearing villi.
4. Lactose intolerance differs from "milk allergy," which is an immune-mediated reaction to cow's milk proteins.
Celiac Disease (CD)
1. Diagnosis requires serological markers (tTG-IgA, tTG-IgG, deamidated gliadin peptide antibodies, EMA-IgA) followed by endoscopy with small bowel biopsy.
2. Histopathology: Increased lymphocytes, mucosal inflammation, villous atrophy, and crypt hyperplasia upon exposure to gluten.
3. On gross inspection: "Scalloping" of the duodenal folds and increased vascularity.
4. Common associations: Dermatitis herpetiformis (~10% of CD patients), reduced bone density, increased risk of malignancy.
5. Treatment: Gluten-free diet.
Tropical Sprue
1. Histopathology: Villous atrophy, increased crypt depth, epithelial cell enlargement, and increased lymphocytic and inflammatory cells.
2. Differentiation from celiac disease through serologic tests.
3. Treatment: Folic acid and Vitamin B12 supplementation, plus antibiotics (tetracycline, ampicillin, etc.).
Whipple Disease
1. Clinical presentation: Starts with arthralgias, followed by neurologic symptoms and later GI effects.
2. Diagnosis: PAS-positive staining after small bowel biopsy showing PAS-positive foamy macrophages in the lamina propria and villous atrophy.
3. PCR tests for T. whipplei DNA in the CSF are important due to potential neurologic complications.
4. Treatment: Antibiotics (ceftriaxone or penicillin, then trimethoprim/sulfamethoxazole); fatal without treatment.
5. Relapses are common.
- --
Beyond the Tutorial
Pathophysiologic Mechanisms
1. Fat-soluble vitamin deficiencies: Specific clinical manifestations of vitamins A, D, E, and K deficiency in malabsorption states.
2. Small intestinal bacterial overgrowth (SIBO): Role in secondary malabsorption, diagnostic approaches, and treatment.
3. Bile acid malabsorption: Impact on fat digestion and development of diarrhea.
4. Transport protein defects: Genetic disorders affecting intestinal absorption.
5. Post-surgical malabsorption: Consequences of intestinal resection, bypass procedures, and altered anatomy.
Laboratory Diagnosis
1. D-xylose absorption test: Principles, procedure, and interpretation.
2. Fecal fat determination: Quantitative versus qualitative methods.
3. Specific antibody tests: Sensitivity and specificity for celiac and other autoimmune enteropathies.
4. Genetic testing: When to consider testing for hereditary malabsorption disorders.
5. Imaging studies: Role of CT, MRI and nuclear medicine studies in evaluation of malabsorption.
Clinical Pearls
1. Extra-intestinal manifestations: Recognition of dermatologic, hematologic, and neurologic findings as clues to underlying malabsorption.
2. Pharmacokinetic implications: Impact of malabsorption on medication dosing and effectiveness.
3. Age-related considerations: Differences in presentation and management across the lifespan.
4. Nutritional rehabilitation: Strategies for safe refeeding and monitoring.
5. Emerging therapies: Novel approaches to management of refractory malabsorption syndromes.
