USMLE/COMLEX 1 - Liver Disease Overview
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Liver Pathophysiology Overview tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
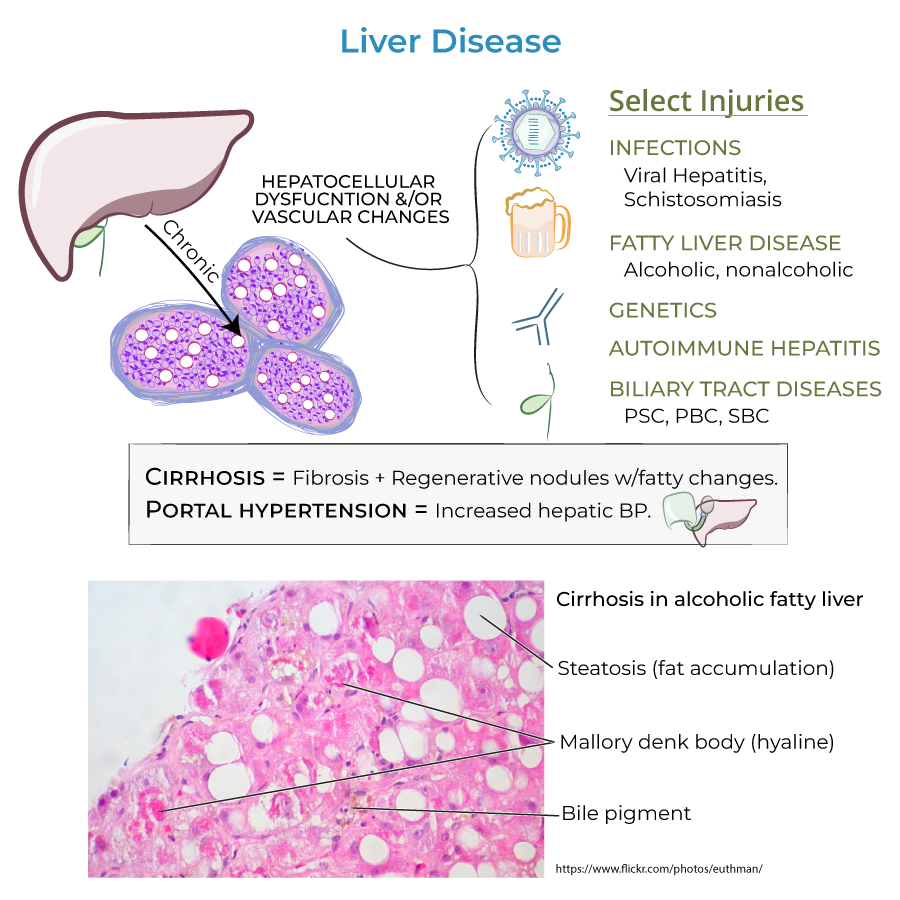
Stages of Liver Disease
1. Four progressive stages: inflammation, fibrosis, cirrhosis, and liver failure.
2. Stage 1 (Inflammation): Hepatic tissues are inflamed from fighting infection or healing injuries.
3. Stage 2 (Fibrosis): Scar tissue replaces normal hepatic tissue.
4. Stage 3 (Cirrhosis): Extensive scarring impairs liver function; signs and symptoms may appear (decompensation).
5. Stage 4 (Liver Failure): Requires urgent medical attention.
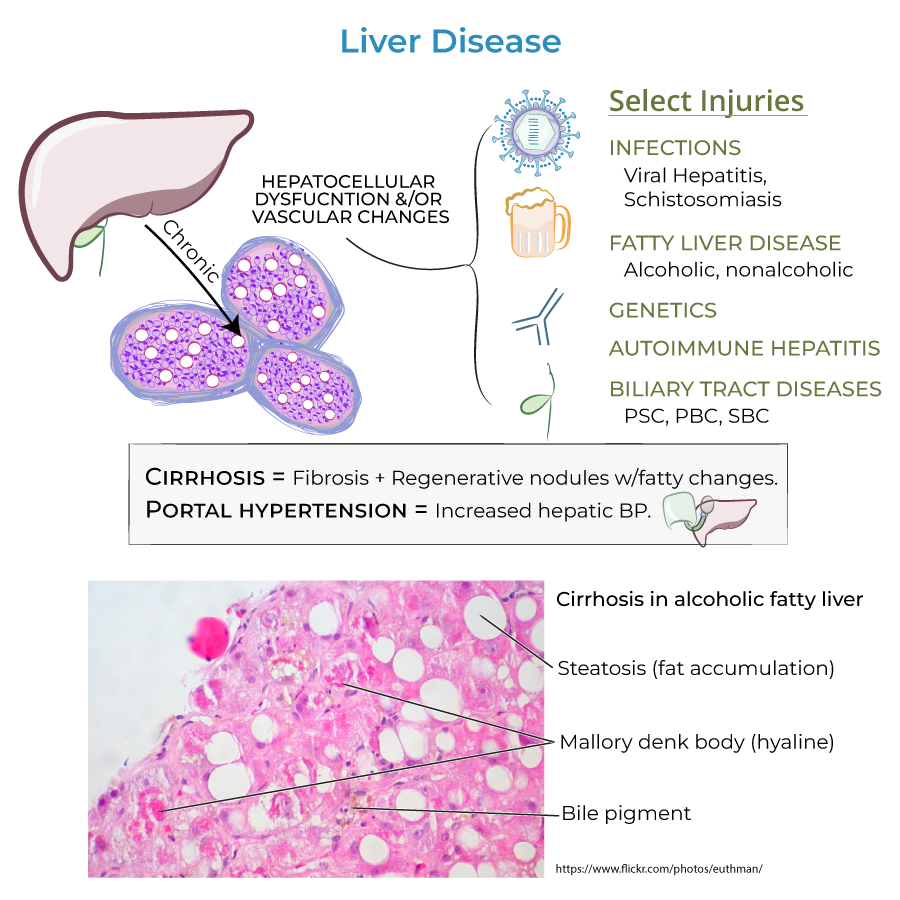
Cirrhosis & Portal Hypertension
1. Cirrhosis: Characterized by fibrosis and regenerative nodules with fatty changes.
2. Portal hypertension: Increased hepatic blood pressure (above 6 mmHg).
3. Reversibility: Newer research indicates that cirrhosis (stage 3) is also reversible, not just stages 1 and 2.
Liver Functions
1. Energy metabolism: Key roles in carbohydrate and lipid metabolism.
2. Plasma protein synthesis: Albumin, clotting factors, angiotensinogen, IGF-1.
3. Storage: Glucose, vitamins B12, D, and K, copper, and iron.
4. Degradation, detoxification, clearance: Ammonia (to form urea), bilirubin, drugs, and toxins.
Sources of Liver Injury
1. Infections: Viral hepatitis and Schistosomiasis.
2. Fatty liver disease: Alcoholic and nonalcoholic forms.
3. Genetic disorders: Hereditary hemochromatosis.
4. Autoimmune hepatitis.
5. Biliary tract diseases: Primary sclerosing cholangitis, primary biliary cholangitis, and secondary biliary cholangitis.
- --
HIGH YIELD
Complications: Impaired Synthesis and Storage
1. Coagulopathy: Results from decreased storage of vitamin K and synthesis of clotting factors.
Complications: Impaired Degradation and Clearance
1. Hepatic encephalopathy: Result of toxin build-up in the blood; ammonia is a key culprit.
2. Asterixis: "Flapping hand tremor" or "liver flap" indicates metabolic encephalopathy.
Complications: Drug Reactions and Hormone Imbalances
1. Elevated estrogen levels: Can cause spider angiomas, palmar erythema, and gynecomastia.
Complications: Impaired Bile Flow
1. Multiple effects: Can lead to hyperlipidemia, jaundice, and malabsorption of GI contents.
Complications: Glucose Metabolism
1. Blood glucose abnormalities: Patients can be hyper- or hypoglycemic.
Complications of Portal Hypertension
1. Varices: Collateral blood vessels that pose significant risk for hemorrhage and GI bleeding.
2. Ascites: Accumulation of fluid in the peritoneum; a main complication of cirrhosis.
3. Spontaneous Bacterial Peritonitis (SBP): Acute infection from bacteria and endotoxins leaking from the GI tract.
4. Renal insufficiency/failure: Result of local vasoconstriction and inflammatory processes.
5. Hepatopulmonary syndrome: Pulmonary vasodilation leads to ventilation/perfusion mismatch and hypoxemia.
6. Liver cancer: Increased risk in advanced disease.
- --
Beyond the Tutorial
Diagnostic Approaches
1. Non-invasive assessments: FibroScan (transient elastography), serum biomarkers (FibroTest, APRI, FIB-4).
2. Liver biopsy: Still the gold standard for assessing liver fibrosis and inflammation.
3. Imaging studies: Ultrasound, CT, and MRI can help diagnose cirrhosis and complications.
Clinical Pearls: Portal Hypertension
1. Portosystemic anastomoses: Key locations include gastroesophageal junction (esophageal varices), rectum (hemorrhoids), umbilicus (caput medusae), and retroperitoneum.
2. TIPS procedure: Transjugular intrahepatic portosystemic shunt for managing refractory ascites and variceal bleeding.
3. Hepatorenal syndrome: Type 1 (rapidly progressive) vs. Type 2 (moderate renal dysfunction).
Drug Metabolism in Liver Disease
1. Phase I (cytochrome P450) and Phase II (conjugation) metabolism alterations.
2. Child-Pugh score: Used to adjust medication dosing based on severity of liver dysfunction.
3. Medications to avoid: Acetaminophen, NSAIDs, certain antibiotics, and sedatives may worsen liver function.
Nutritional Considerations
1. Protein requirements: Contrary to older beliefs, most patients with liver disease need normal-to-increased protein intake.
2. Sodium restriction: Important for ascites management (typically 2000 mg/day).
3. Branched-chain amino acids: May benefit patients with hepatic encephalopathy.
