USMLE/COMLEX 1 - Large Vessel Vasculitis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Large Vessel Vasculitis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 1
General Features of Large Vessel Vasculitis
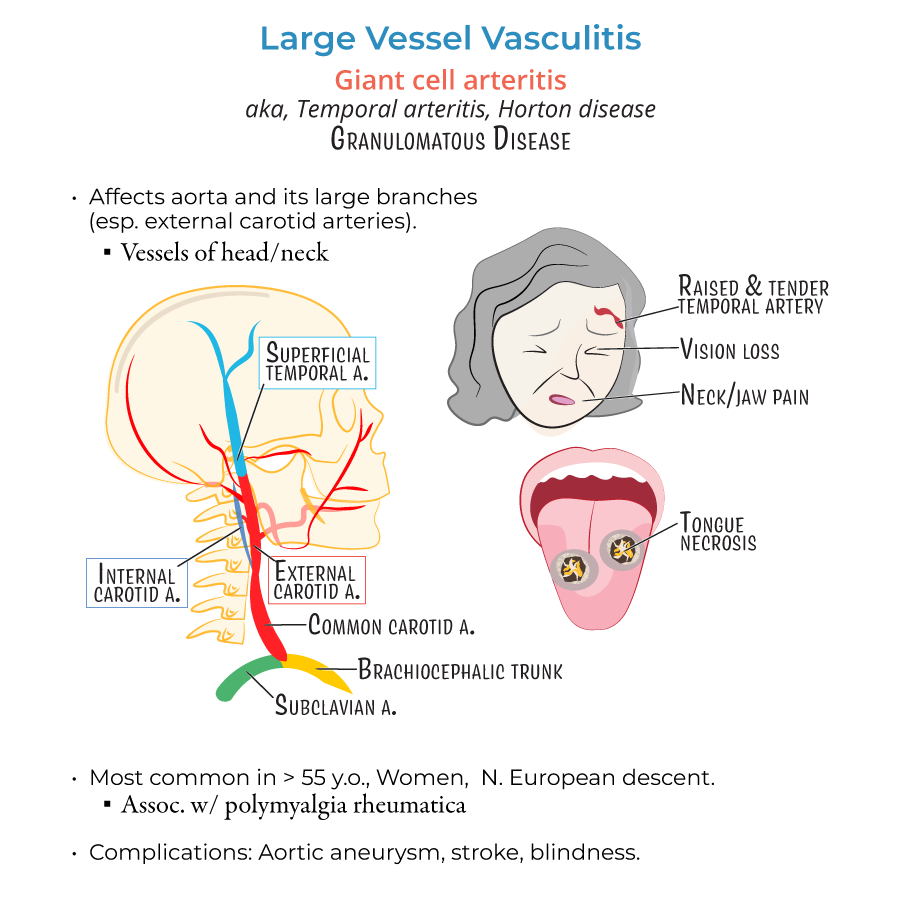
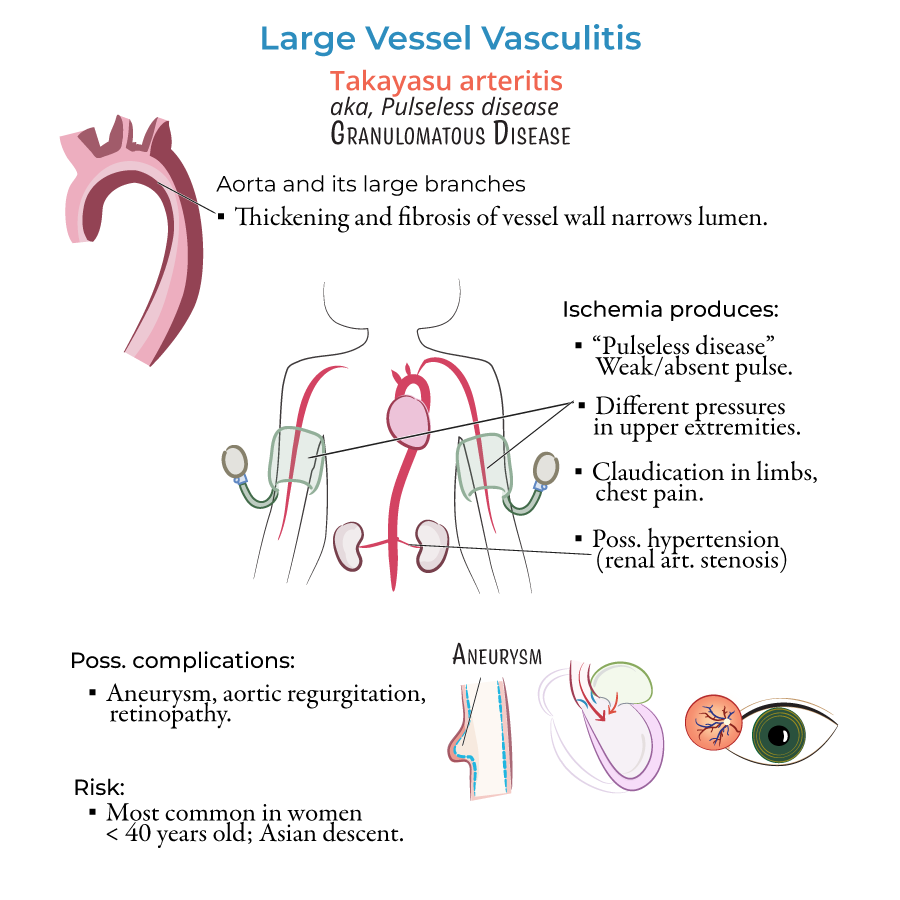
1. Large vessel vasculitis affects the aorta and its major branches and causes chronic vessel wall inflammation, leading to ischemia and organ damage.
2. General symptoms include fever, fatigue, weight loss, arthralgias, and myalgias due to systemic inflammation.
3. Treatment for both giant cell arteritis and Takayasu arteritis includes corticosteroids as first-line therapy.
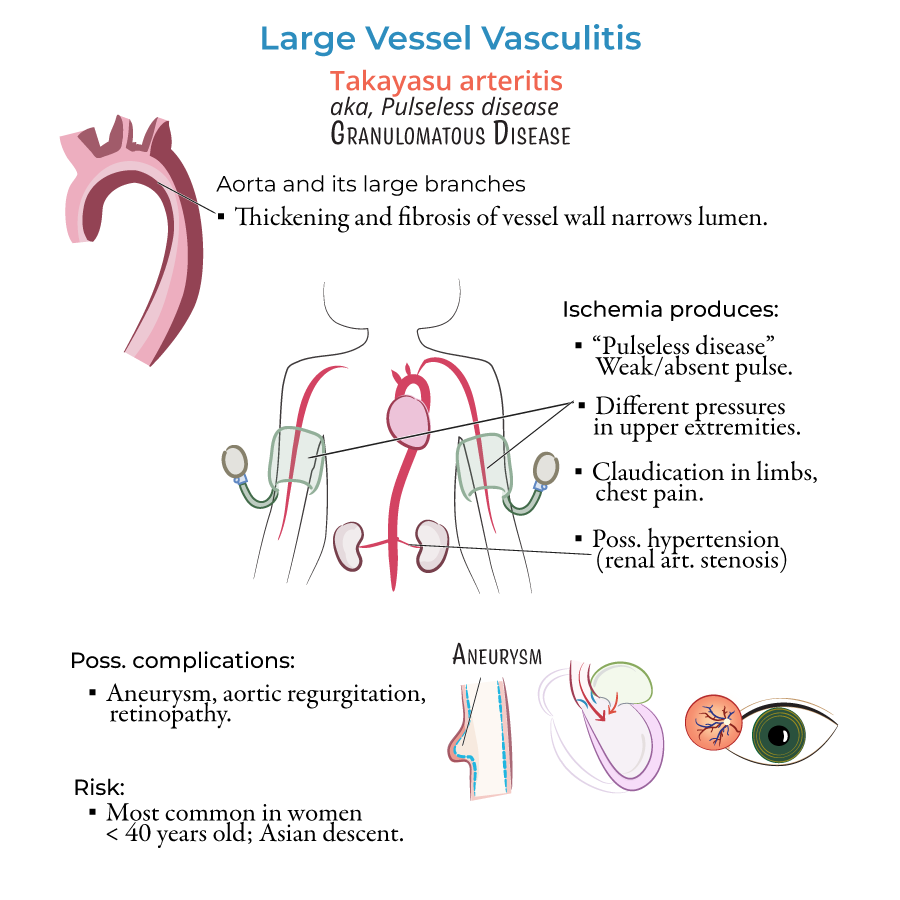
Giant Cell Arteritis (Temporal Arteritis)
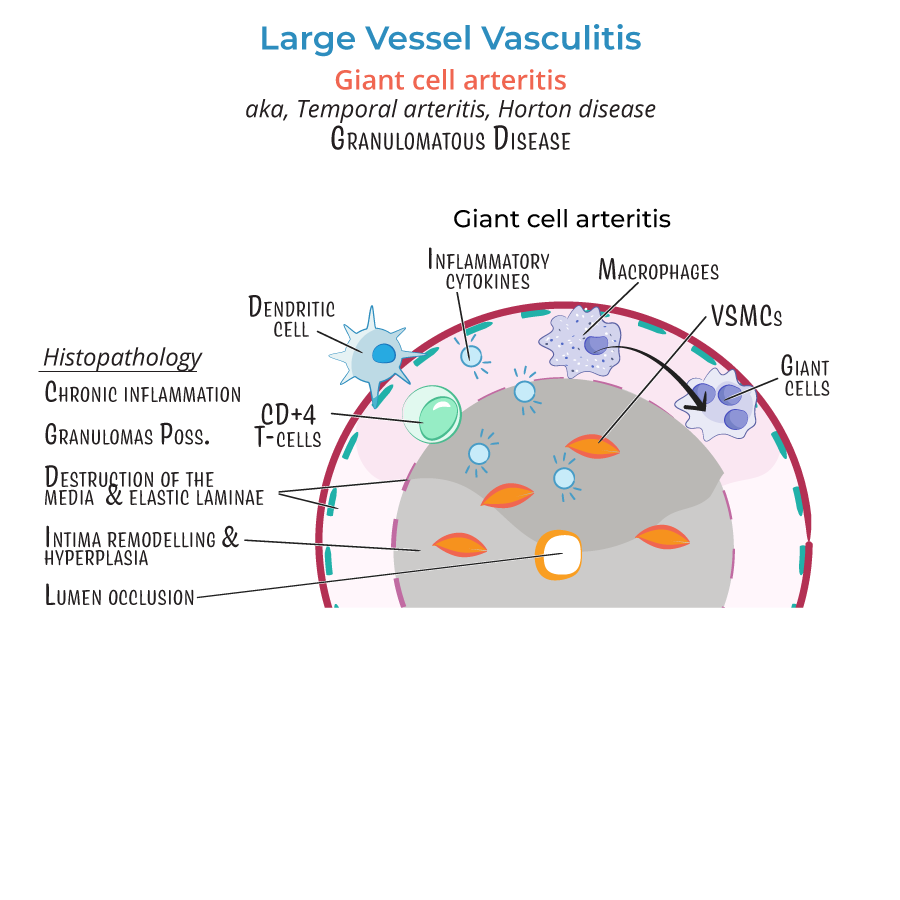
4. It is a granulomatous large vessel vasculitis most commonly affecting the branches of the carotid artery, especially the temporal artery.
5. Classic findings include:
- Temporal headache with tender or palpable temporal artery
- Jaw claudication
- Vision loss (due to ophthalmic artery involvement)
- Scalp tenderness
Takayasu Arteritis
10. Granulomatous vasculitis affecting the aortic arch and proximal great vessels.
11. Commonly affects young women under 40, especially those of Asian descent.
12. Classic features include:
- Diminished or absent pulses
- Asymmetric blood pressures
- Bruits over large arteries
- Limb claudication
- --
HIGH YIELD
Histopathologic and Immunologic Mechanisms
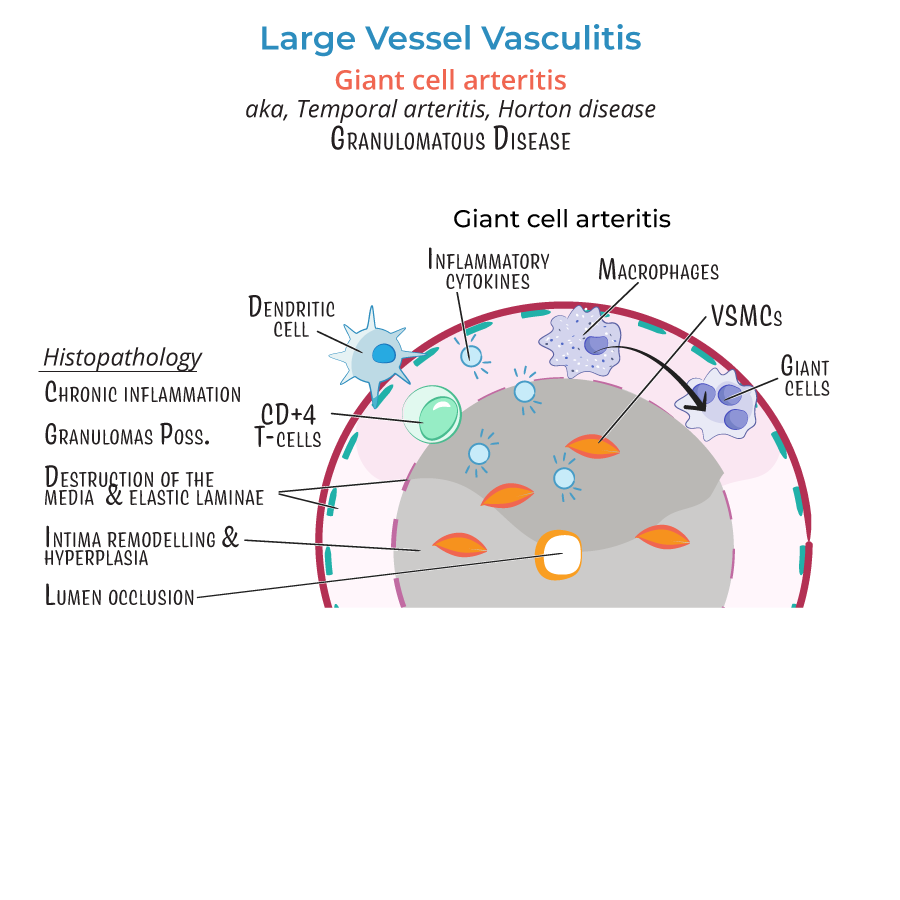
1. In giant cell arteritis, dendritic cells in the adventitia may be activated by infectious triggers.
2. These dendritic cells activate CD4+ T cells, which release cytokines to recruit macrophages.
3. Activated macrophages form giant cells, secrete reactive oxygen species (ROS), nitric oxide, and matrix metalloproteinases (MMPs), leading to media destruction and elastic lamina breakdown.
4. Smooth muscle proliferation in the intima contributes to fibrous cap formation and luminal narrowing.
5. Histological findings also include fragmentation of the internal elastic lamina and mononuclear cell infiltrates.
Clinical Clues and Associations
6. Giant cell arteritis should be suspected in any patient over 50 with new-onset headache, jaw claudication, or visual symptoms.
7. Temporal artery biopsy is the gold standard diagnostic test for GCA but should not delay steroid initiation.
8. Takayasu arteritis may be suspected in young women with absent pulses, BP discrepancies, or limb ischemia.
9. Bruits over the subclavian or carotid arteries are key physical findings.
10. Hypertension in Takayasu is often secondary to renal artery stenosis.
- --
Beyond the Tutorial
Diagnostic and Clinical Pearls
1. For GCA, ESR and CRP are typically elevated; temporal artery biopsy may show segmental lesions, so a negative biopsy does not rule it out.
2. GCA and PMR often respond to low-dose prednisone for PMR or high-dose prednisone for GCA with ocular involvement.
3. MRA or CT angiography can demonstrate large vessel narrowing or wall thickening in Takayasu arteritis.
4. Takayasu arteritis may mimic coarctation of the aorta or other large vessel occlusive diseases.
5. Other large vessel vasculitides to differentiate:
- Syphilitic aortitis (affects vasa vasorum of thoracic aorta)
- IgG4-related aortitis (rare, with systemic fibrosis and elevated serum IgG4)
