USMLE/COMLEX 1 - Jaundice
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Jaundice tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 1. Jaundice is a sign of underlying disorder requiring investigation.
2. Key diagnostic tests:
1. Jaundice is a sign of underlying disorder requiring investigation.
2. Key diagnostic tests:
- --
VITAL FOR USMLE/COMLEX 1
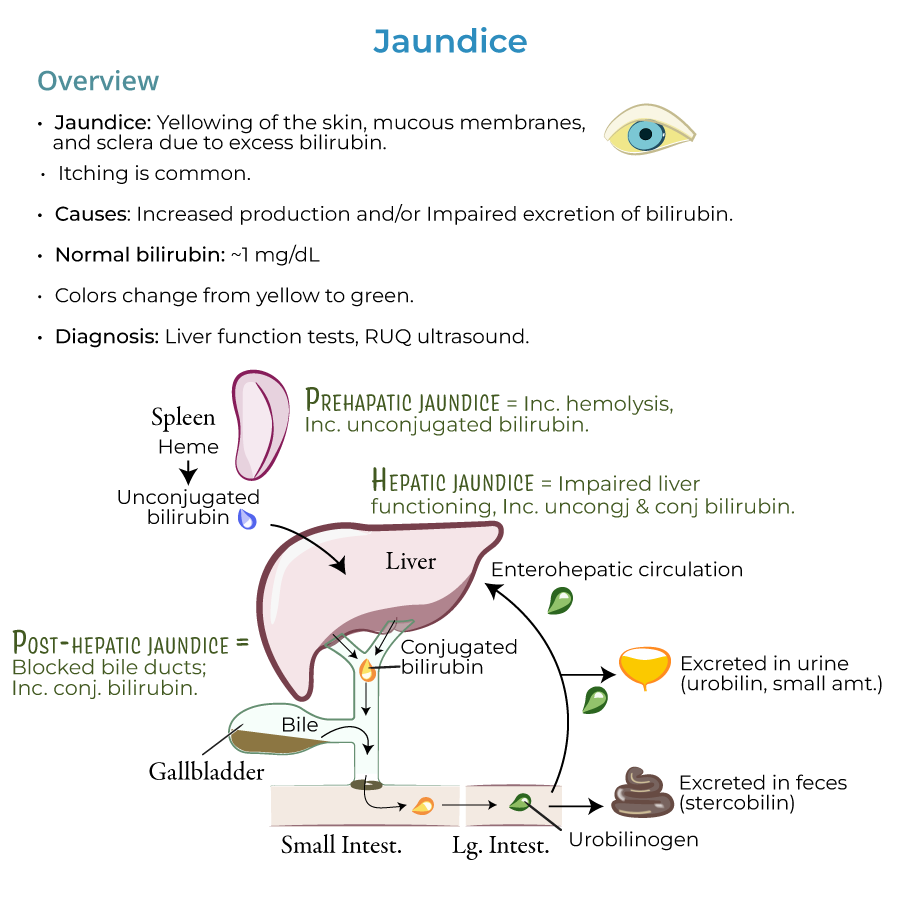
Definition & Appearance
1. Jaundice: Yellowing of the skin, mucous membranes, and sclera due to excess bilirubin; itching is also common.
2. Bilirubin: A pigment in the bile; it is a by-product of heme degradation.
3. Visible jaundice usually present when bilirubin levels reach 2.5 mg/dL or higher (normal is approximately 1 mg/dL).
4. Jaundice can progress from a yellowish to greenish color as bilirubin accumulates.
5. Differential diagnosis: Excess carotene can cause yellow/orange skin color, but the sclera is spared.
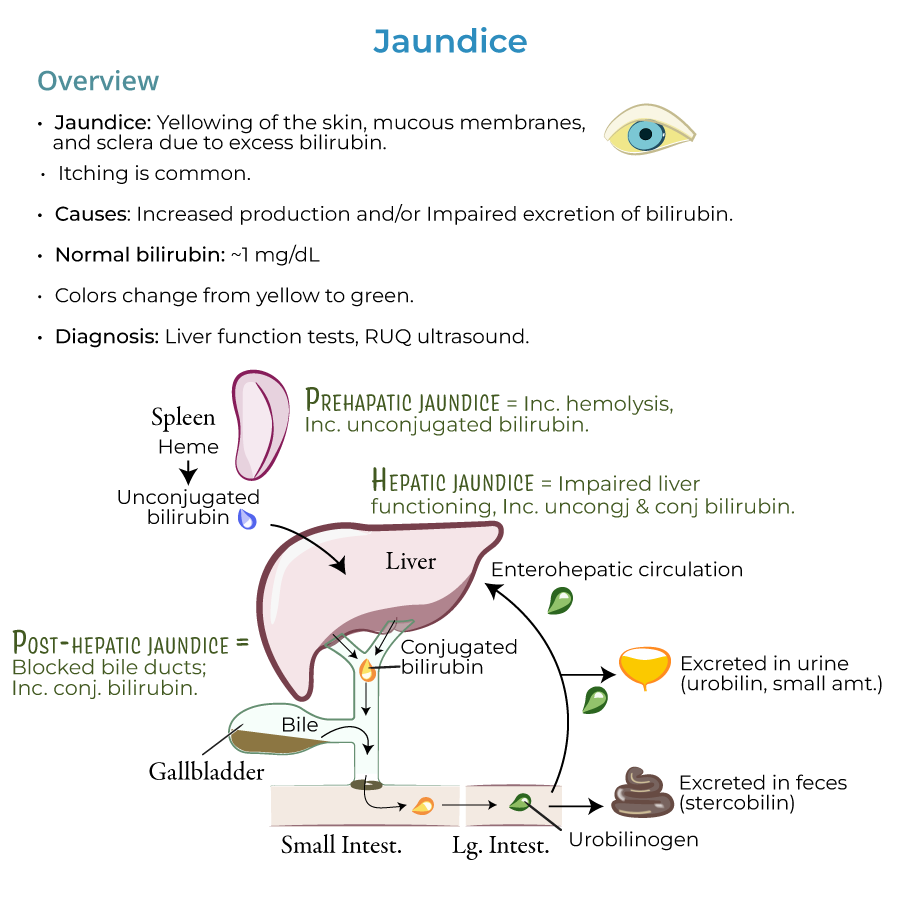
Pathophysiology Framework
1. Pre-hepatic phase: Heme converted to unconjugated bilirubin in reticuloendothelial cells, primarily in the spleen.
2. Hepatic phase: Unconjugated bilirubin travels to liver, where it's taken up by hepatocytes and conjugated.
3. Post-hepatic phase: Transfer of conjugated bilirubin in bile through the biliary system to intestines.
4. Bacterial enzymes in intestine reduce conjugated bilirubin to produce urobilinogens.
5. Most urobilinogen excreted in feces as stercobilin (gives feces brown color); small portion excreted in urine as urobilin.
Major Etiologies (HOT Liver mnemonic)
1. H: Hemolysis (pre-hepatic, unconjugated hyperbilirubinemia)
2. O: Obstruction (post-hepatic, conjugated hyperbilirubinemia)
3. T: Tumors (can cause obstruction or liver damage)
4. Liver diseases: Hepatocellular damage (mixed hyperbilirubinemia)
- --
HIGH YIELD
Indirect (Unconjugated) Hyperbilirubinemia
1. Key feature: Unconjugated bilirubin does not appear in urine (not water soluble).
2. Pre-hepatic causes (excess production):
- Increased hemolysis: Sickle cell anemia, G6PD deficiency
- Inefficient erythropoiesis: Thalassemia, pernicious anemia
- Increased bilirubin production: Massive blood transfusions, hematoma resorption
- Medications: Protease inhibitors, Rifampin
- Gilbert syndrome: Mild, intermittent symptoms (UDP-glucuronosyltransferase deficiency)
- Crigler-Najjar syndrome: Can be mild or severe; Type 1 has total lack of UDP-glucuronosyltransferase, risking kernicterus
Direct (Conjugated) Hyperbilirubinemia
1. Key feature: Excess conjugated bilirubin is water soluble and appears in urine (dark urine).
2. Genetic disorders:
- Dubin-Johnson syndrome: Often asymptomatic, defects in bilirubin secretion
- Rotor syndrome: Generally benign and self-limiting, defects in bile storage
- Post-hepatic causes:
- Gallstone obstruction (cholelithiasis, choledocholithiasis)
- Biliary system inflammation, atresia, or strictures
- Ductal compression from tumors or pancreatitis
- Intrahepatic causes:
- Cholestatic liver disease (primary biliary cholangitis, primary sclerosing cholangitis)
- Infiltrative liver diseases (amyloidosis, lymphoma, sarcoidosis, tuberculosis)
- Sepsis, pregnancy, total parenteral nutrition, malaria
Mixed Hyperbilirubinemia
1. Key feature: Increased levels of both unconjugated and conjugated bilirubin with abnormal liver function tests.
2. Major causes (hepatocellular injury):
- Hepatitis: Viral, alcoholic, autoimmune, nonalcoholic steatohepatitis
- Other viral infections: Yellow fever, EBV, CMV, HSV
- Other disorders: Cirrhosis, Wilson's disease
- Drugs and toxins: Estrogen, acetaminophen, arsenic
Newborn Hyperbilirubinemia
1. Newborn jaundice: Common and generally benign due to immature hepatic conjugation; resolves in weeks.
2. Breast milk jaundice: Benign form lasting 3-12 weeks, resolves on its own.
3. Breastfeeding jaundice: Occurs when infant takes in too little breastmilk for sufficient stool production.
4. Caution: Newborns are particularly susceptible to kernicterus (brain damage from bilirubin deposits).
- --
DIAGNOSIS
- Liver function tests
- Right upper quadrant ultrasound (when biliary obstruction suspected)
- --
Beyond the Tutorial
Bilirubin Metabolism
1. Heme catabolism: Heme → biliverdin → bilirubin via heme oxygenase and biliverdin reductase.
2. Plasma transport: Unconjugated bilirubin bound to albumin in plasma (important for understanding drug displacement effects).
3. Conjugation enzyme: UDP-glucuronosyltransferase (UGT1A1) adds glucuronic acid to make bilirubin water-soluble.
4. Enterohepatic circulation: 10-15% of urobilinogen is reabsorbed and recycled to the liver or excreted by kidneys.
Laboratory Findings
1. Van den Bergh reaction: Differentiates direct (conjugated) from indirect (unconjugated) bilirubin.
2. Urobilinogen: Increased in urine with hemolysis; decreased/absent with complete biliary obstruction.
3. AST/ALT ratio: Typically >2:1 in alcoholic hepatitis; <1:1 in viral hepatitis (important differentiating feature).
4. Alkaline phosphatase: Significantly elevated in cholestatic and infiltrative disorders.
5. Gamma-glutamyl transferase (GGT): Helps distinguish bone-origin vs. liver-origin alkaline phosphatase elevation.
Neonatal Jaundice Specifics
1. Physiologic jaundice peaks at 3-5 days in term infants, 5-7 days in preterm infants.
2. Pathologic jaundice red flags: onset <24 hours after birth, bilirubin rising >5 mg/dL/day, or persistent >2 weeks.
3. Phototherapy: Converts bilirubin to water-soluble photoisomers that can be excreted without conjugation.
4. Kernicterus risk factors: Prematurity, acidosis, hypoalbuminemia, drugs that displace bilirubin from albumin.
5. ABO/Rh incompatibility: Leading cause of hemolytic disease of the newborn causing jaundice.
Special Considerations
1. Drug metabolism: Jaundice can result from Phase I/II drug metabolism impairment (not just bilirubin metabolism).
2. Gilbert's syndrome is exacerbated by fasting, stress, and illness; affects 3-10% of population (most common inherited cause).
3. Delta bilirubin: Conjugated bilirubin that covalently binds to albumin; remains elevated longer in resolving jaundice.
4. Vanishing bile duct syndrome: Progressive destruction of intrahepatic bile ducts in various conditions.
5. Reye's syndrome: Encephalopathy and fatty liver associated with aspirin use in children with viral illnesses; presents with jaundice.
