USMLE/COMLEX 1 - Ischemic Heart Disease Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Ischemic Heart Disease tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards.
 2. Plaque Erosion:
2. Plaque Erosion:
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
Cardiac Ischemia: Basics
1. Definition: Occurs when coronary blood flow is insufficient for metabolic needs.
2. Result: Impaired mechanical and/or electrical cardiac function.
3. Acute Coronary Syndrome (ACS): Umbrella term for sudden cardiac ischemia events.
4. Leading cause of death in both men and women worldwide.
5. Important risk factors: Family history, age, smoking, hypertension, diabetes, hyperlipidemia, obesity, low physical activity.
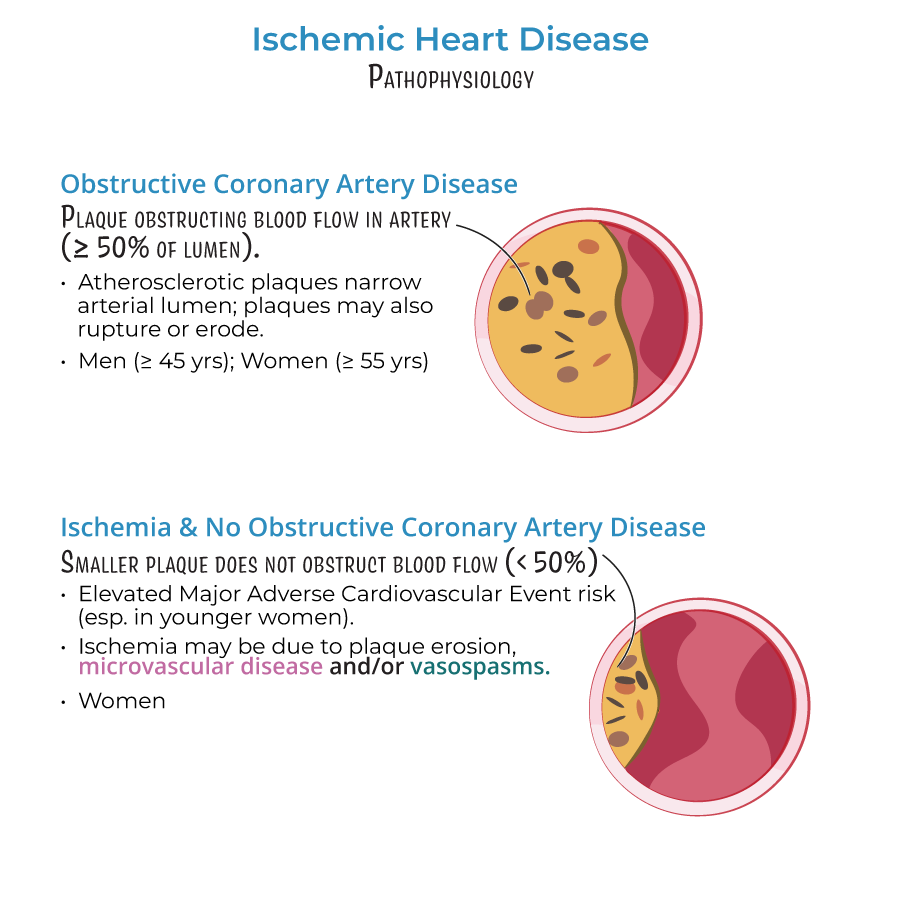
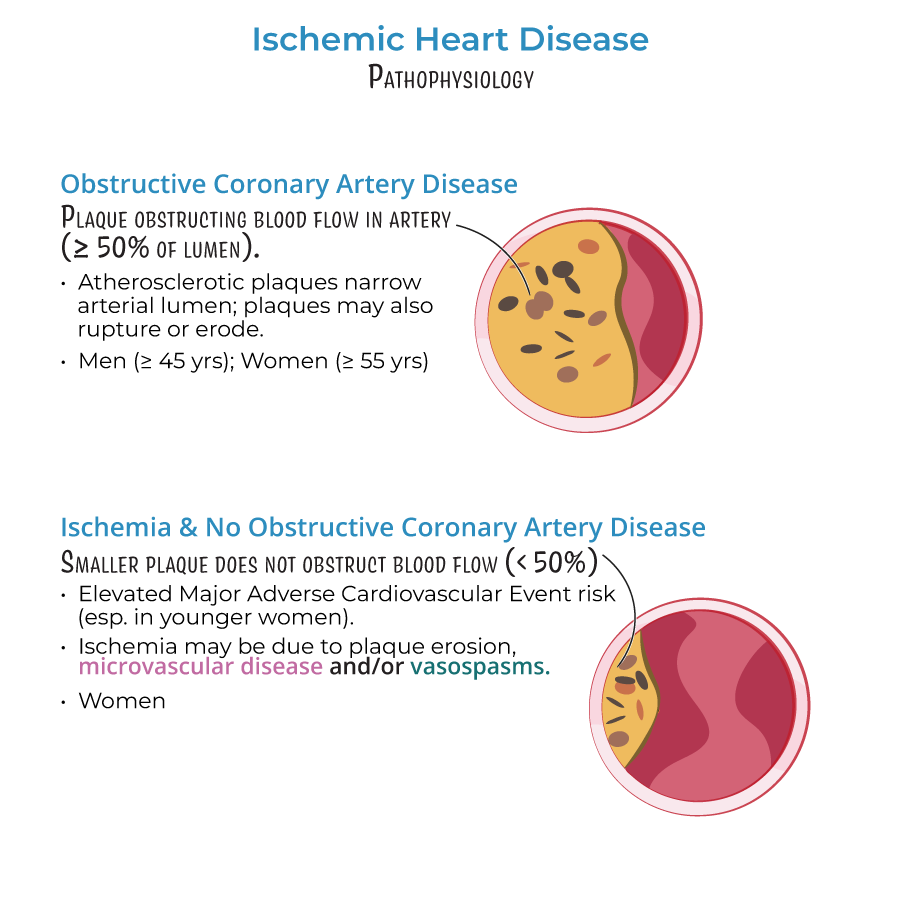
Obstructive Coronary Artery Disease (CAD)
1. Definition: Atherosclerotic plaques obstructing ≥50% of epicardial artery lumen.
2. Demographics: Primarily men >45 years; women >55 years.
3. Complications: Plaque rupture or erosion can produce thrombi leading to acute coronary events.
4. Key fact: Up to 50% of patients with suspected ischemia have no significant coronary obstruction on angiogram.
INOCA (Ischemia with No Obstructive Coronary Artery Disease)
1. Definition: Smaller plaques (<50% obstruction) with non-obstructive flow limitation.
2. Demographics: Common in women (~30% of men also affected).
3. Significance: Associated with elevated risk of Major Adverse Cardiovascular Events (MACE).
4. Mechanisms: Plaque erosion, microvascular disease, and/or vasospasm.
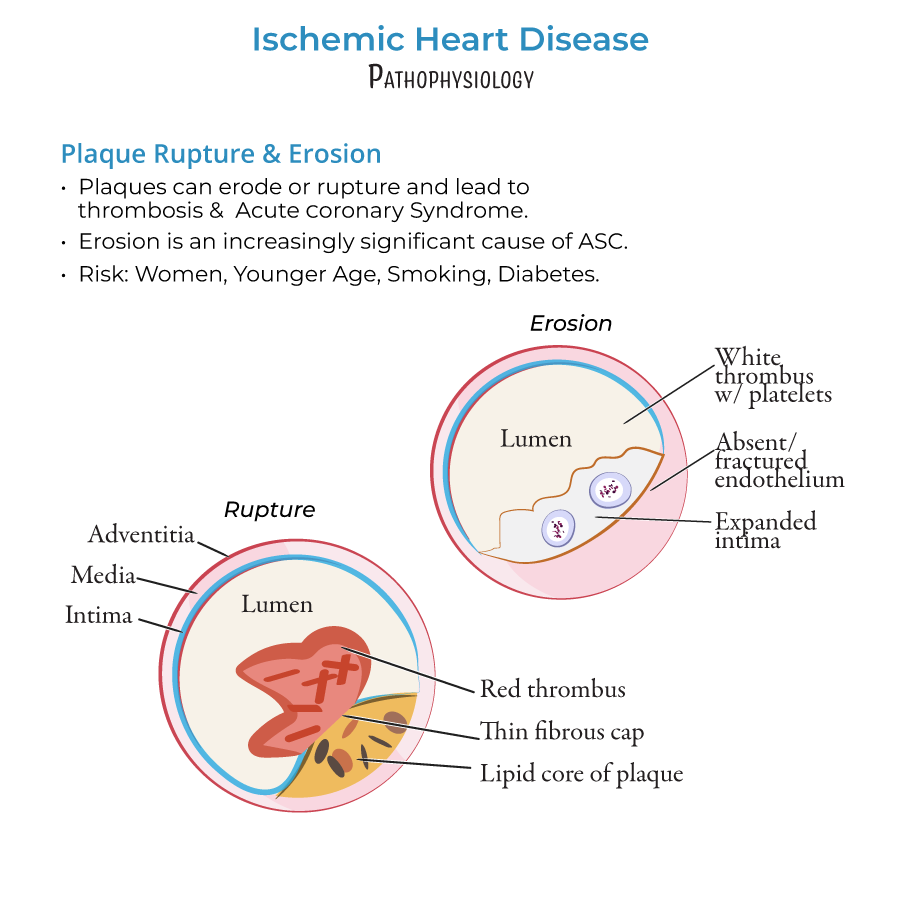
Plaque Rupture vs. Erosion
1. Plaque Rupture:
- Tears in fibrous caps releasing thrombogenic contents
- Characterized by lipid cores and thin caps
- Forms fibrin-rich "red thrombi"
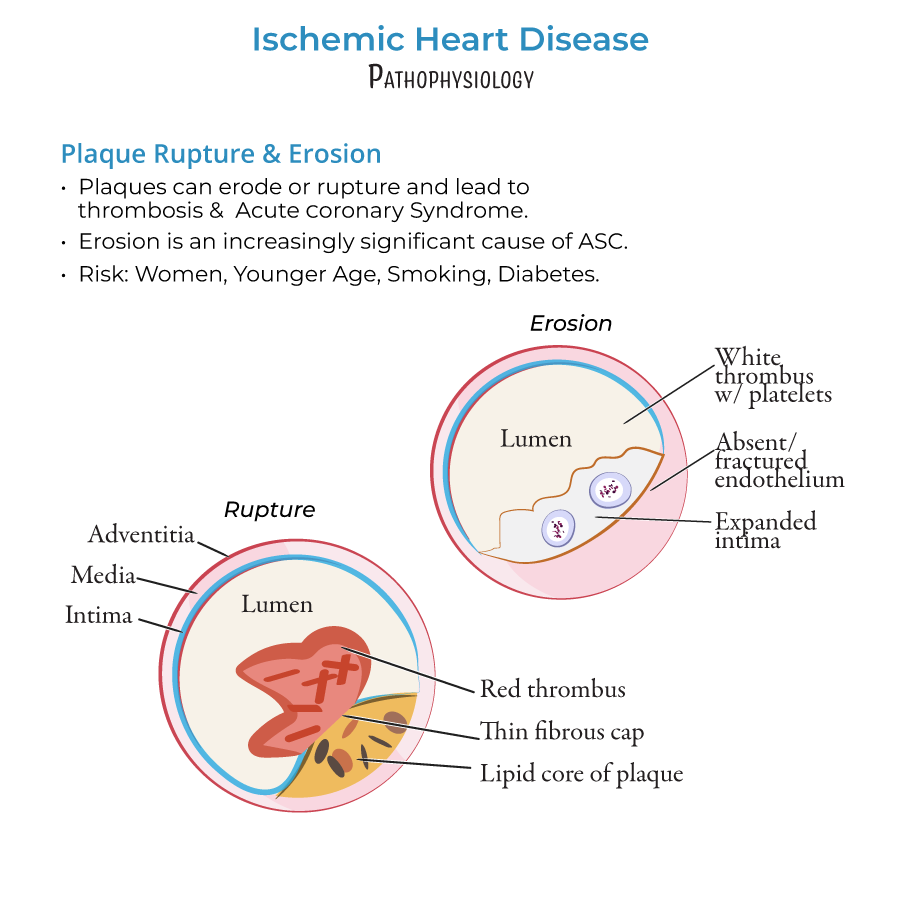 2. Plaque Erosion:
2. Plaque Erosion:
- Increasingly significant cause of ACS
- More common in women, young individuals, smokers, and diabetics
- Thick cap plaques producing platelet-rich "white thrombi"
- Associated with endothelial dysfunction or absence
- --
HIGH YIELD
Coronary Blood Supply
1. Epicardial coronary arteries: Run along heart surface (left and right coronary arteries and branches).
2. Microvasculature: Prearterioles, arterioles, and capillaries in deeper cardiac tissues.
3. Function: Prearterioles and arterioles provide resistance and regulation of blood flow.
Coronary Microvascular Dysfunction (CMD)
1. Significance: Major cause of INOCA, can coexist with obstructive CAD.
2. Demographics: Affects both sexes in near-equal proportions.
3. Mechanisms:
- Structural: Arteriole remodeling with thicker walls and reduced wall:lumen ratio
- Functional: Impaired vasodilation due to endothelial dysfunction
- Diffuse pattern: Produces patchy areas of ischemia (vs. localized epicardial lesions)
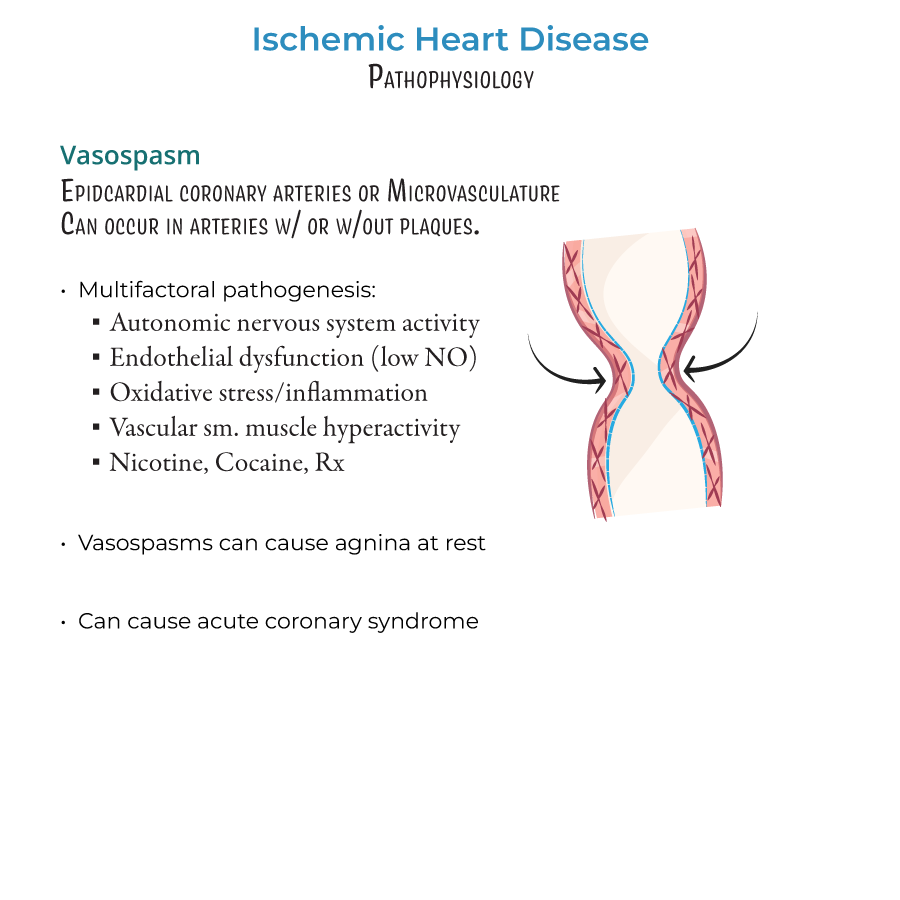
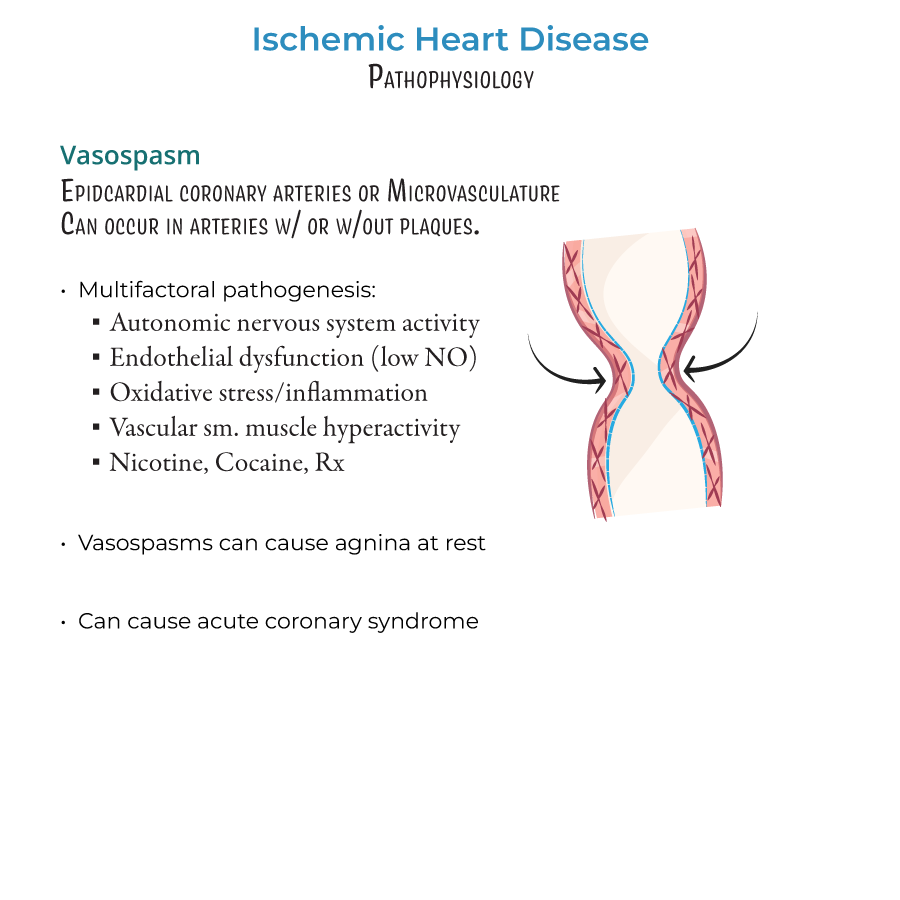
Vasospasm
1. Location: Can occur in epicardial arteries and microvasculature.
2. Context: Can happen with or without stenosis.
3. Triggers:
- Enhanced autonomic nervous system activity
- Endothelial dysfunction (especially reduced nitric oxide)
- Oxidative stress and inflammation
- Vascular smooth muscle hyperactivity
- Substances: nicotine, cocaine, vasoconstricting medications
Cross-Type Concepts
1. Sex differences:
- INOCA and plaque erosion more common in women
- Obstructive CAD more common in men
- Risk factors may have stronger effects in women
- Plaque rupture decreasing due to statin use
- Plaque erosion increasing in clinical significance
- --
Beyond the Tutorial
Clinical Manifestations
1. Stable angina: Predictable chest pain with exertion, relieved by rest or nitroglycerin.
2. Unstable angina: Chest pain at rest or with minimal exertion, increasing in frequency/severity.
3. Prinzmetal (variant) angina: Caused by coronary vasospasm, occurs at rest, often in early morning.
4. Microvascular angina: Chest pain with normal coronary angiogram, due to microvascular dysfunction.
Diagnostic Approaches
1. ECG changes:
- ST depression: Subendocardial ischemia
- ST elevation: Transmural ischemia
- T wave inversion: Ischemia
- Q waves: Completed infarction
Treatment Principles
1. Antiplatelet therapy: Aspirin, P2Y12 inhibitors (clopidogrel, ticagrelor, prasugrel).
2. Anticoagulation: Heparin, low-molecular-weight heparin, fondaparinux.
3. Beta-blockers: Reduce myocardial oxygen demand.
4. Nitrates: Vasodilate coronary arteries, reduce preload.
5. Calcium channel blockers: Especially for vasospastic angina.
6. Statins: Stabilize plaques, reduce inflammation.
7. Revascularization: PCI (percutaneous coronary intervention) or CABG (coronary artery bypass grafting).
