USMLE/COMLEX 1 - Inflammatory Bowel Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Inflammatory Bowel Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 1
Inflammatory Bowel Disease (IBD)
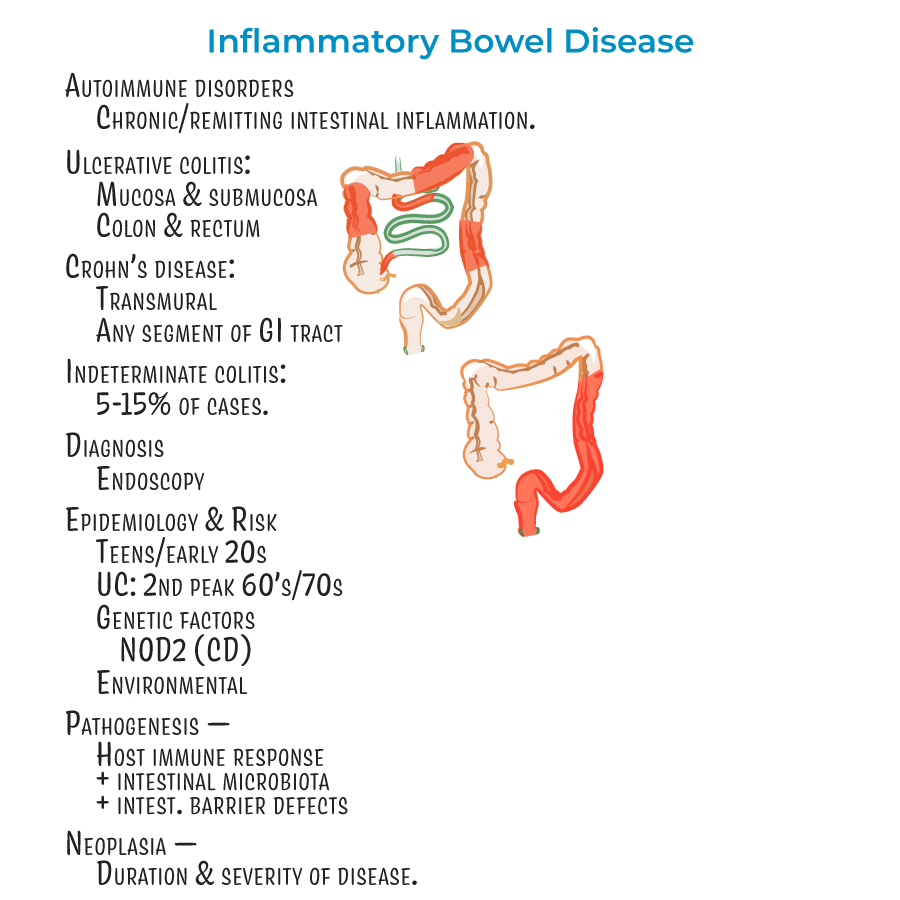
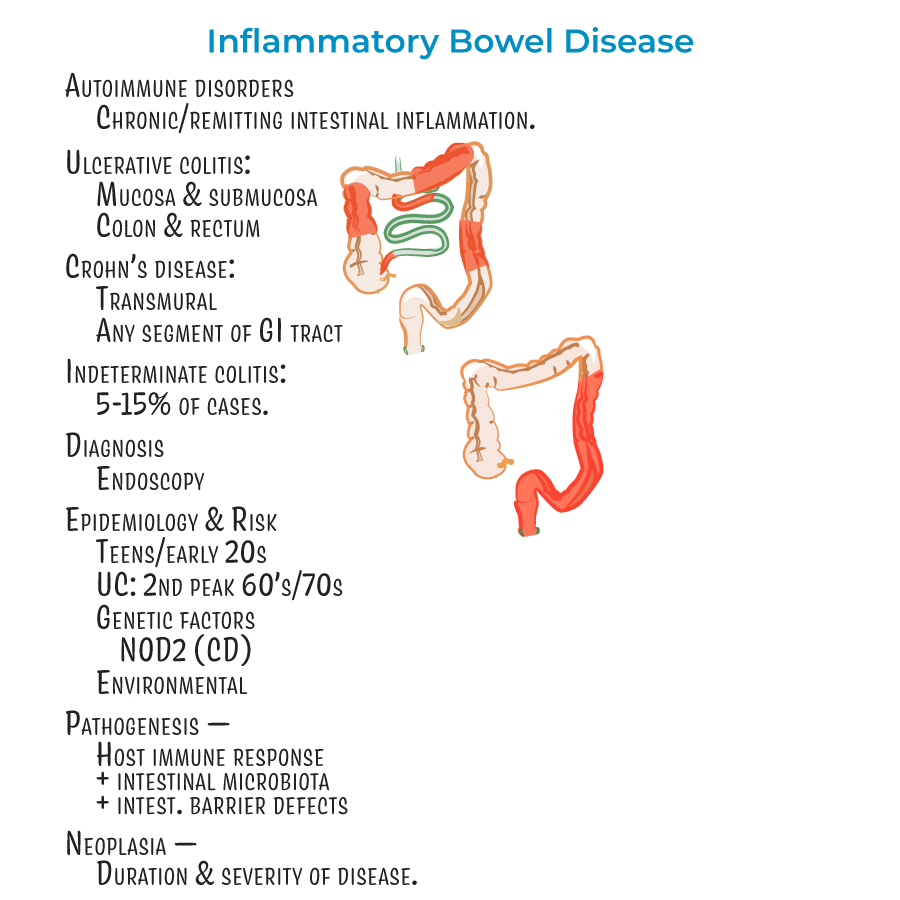
1. Autoimmune disorders characterized by chronic or remitting intestinal inflammation.
2. Diagnosis relies on endoscopy.
3. Most patients diagnosed in teens/early 20s; ulcerative colitis has a second "peak" in patients in their 60's or 70's.
4. Genetic factors play a role (e.g., mutations in NOD2 associated with Crohn's disease).
5. Result of detrimental interactions between host immune response, intestinal microbiota, and intestinal barrier defects.
6. Associated with neoplasia, influenced by duration and severity of disease.
Crohn's Disease
1. Characterized by transmural inflammation (can reach all layers of GI tract).
2. Can affect any segment of GI tract, but most commonly involves ileum and colon.
3. "Skip lesions" - discontinuous pattern with normal areas between affected segments.
4. Rectum usually spared (unlike ulcerative colitis).
5. Histology: crypt distortion, fissures, and noncaseating granulomas (in up to 60% of cases).
6. Inflammation is Th1/Th17 cell-mediated.
Ulcerative Colitis
1. Inflammation of mucosal and submucosal layers only.
2. Restricted to the colon and rectum.
3. Characterized by continuous lesions (unlike Crohn's disease).
4. Sunken, red/bloody ulcers with remaining mucosa creating "pseudopolyps".
5. Histology: crypt distortion with crypt abscesses containing neutrophils.
6. Inflammation is Th2 cell-mediated.
- --
HIGH YIELD
Inflammatory Bowel Disease
1. Environmental factors are important (diet, cigarette smoking, medications).
2. About 5-15% of cases are considered "indeterminant" colitis when distinction between UC and CD is difficult.
3. Extraintestinal manifestations: Most common are skin lesions (in up to 40% of patients), uveitis, and arthritis.
4. Less common but potentially deadly complications: involvement of liver/gallbladder, lung, pancreas, and kidneys.
Crohn's Disease
1. Many studies suggest a female predominance.
2. Transmural inflammation with wall thickening and "creeping fat" that wraps around the GI tract.
3. Lesion types and progression:
- Aphthous erosions (early shallow whitish sores)
- Longitudinal "bear claw" ulcers (look like rake dragged down GI lining)
- Cobblestone appearance (as tissue becomes crowded with ulcers)
- Fissures form and progress to fistulas that open to abdominal/pelvic cavity or connect with other organs
Ulcerative Colitis
1. Inflammation destroys submucosal vascular network.
2. Mucosa is bloody during active inflammation with friable appearance.
3. Signs/symptoms: bloody diarrhea with rectal bleeding, abdominal pain, fever, and weight loss.
4. Complications: toxic ulceritis, toxic megacolon, intestinal perforation, dysplasia and adenocarcinoma (more likely with pancolitis).
5. Treatment: anti-inflammatories, immune suppressors, colectomy.
6. Patients who smoke cigarettes more likely to experience bouts upon quitting.
Differential Diagnosis
1. Key differences:
- CD = transmural inflammation, skip lesions, any GI segment, rectum usually spared
- UC = mucosal/submucosal inflammation, continuous lesions, colon/rectum only
- --
Beyond the Tutorial
Pathophysiology
1. Barrier dysfunction: Defective intestinal epithelial tight junctions contribute to increased permeability.
2. Pattern recognition receptors: NOD2 mutations (chromosome 16) in Crohn's disease impair bacterial sensing.
3. Dysbiosis: Altered microbiota composition with reduced diversity and increased pathobionts.
4. Autophagy defects: ATG16L1 and IRGM gene polymorphisms impair bacterial clearance in Crohn's disease.
Histopathology
1. Lamina propria: Increased plasma cells, lymphocytes, and eosinophils in both diseases.
2. Paneth cell metaplasia: Often seen in ulcerative colitis distal to the hepatic flexure.
3. Neural hyperplasia and hypertrophy: Characteristic of Crohn's disease but not ulcerative colitis.
4. Basal plasmacytosis: Early histologic feature of IBD preceding architectural distortion.
Immunology
1. ASCA (Anti-Saccharomyces cerevisiae antibodies): Associated with Crohn's disease.
2. p-ANCA (perinuclear anti-neutrophil cytoplasmic antibodies): Associated with ulcerative colitis.
3. IL-23/IL-17 axis: Critical pathway in Crohn's disease inflammatory cascade.
4. Regulatory T cells: Dysfunctional Tregs contribute to loss of tolerance to commensal bacteria.
Genetics
1. Concordance rates: Higher in monozygotic than dizygotic twins (especially for Crohn's disease).
2. IL23R polymorphisms: Confer protection against IBD.
3. HLA associations: HLA-DRB1*0103 associated with extensive UC and colonic Crohn's.
4. Genetic risk score: Combination of risk alleles better predicts disease than individual variants.
Laboratory Findings
1. Stool studies: Fecal calprotectin and lactoferrin as non-invasive inflammatory markers.
2. Anemia profile: Microcytic (iron deficiency) vs. macrocytic (B12/folate deficiency) patterns.
3. Liver function tests: Elevated alkaline phosphatase may indicate primary sclerosing cholangitis.
4. Malabsorption markers: Hypoalbuminemia, fat-soluble vitamin deficiencies (A, D, E, K).
Basic Pharmacology
1. 5-ASA compounds: Mechanism involves PPARγ activation and NFκB inhibition.
2. Azathioprine/6-MP: Converted to 6-thioguanine nucleotides that inhibit purine synthesis.
3. Methotrexate: Inhibits dihydrofolate reductase and promotes adenosine release.
4. Anti-TNF mechanism: Neutralizes soluble TNF and induces apoptosis of TNF-expressing cells.
