USMLE/COMLEX 1 - Hypertension Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Blood Pressure Regulation and Hypertension tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 2. Aldosterone:
2. Aldosterone:
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
Blood Pressure Fundamentals
1. Mean arterial pressure is determined by cardiac output and total peripheral resistance.
2. Cardiac output is the product of heart rate and stroke volume.
3. Stroke volume is determined by preload and contractility.
4. Total peripheral resistance is primarily determined by the degree of vasoconstriction in small arteries and arterioles.
5. Hypertension results from increased cardiac output and/or increased total peripheral resistance.
Key Mediators of Blood Pressure
1. Angiotensin II:
- Potent vasoconstrictor
- Increases sodium and water retention
- Stimulates release of norepinephrine, ADH, and aldosterone
- Target of multiple antihypertensive drug classes
 2. Aldosterone:
2. Aldosterone:
- Secreted by adrenal cortex
- Increases sodium and water retention, leading to increased blood volume and cardiac output
- Secreted by posterior pituitary
- Vasoconstrictor
- Increases water reabsorption in collecting ducts
- Vasoconstrictor
- Increases heart rate and contractility
- Chronic hypertension leads to thickening of vessel walls
- Increases endothelin (vasoconstrictor)
- Decreases nitric oxide (vasodilator)
Hypertensive Crisis
1. Definition: Blood pressure exceeding 180/120 mmHg
2. Hypertensive urgency: No end-organ damage
3. Hypertensive emergency: End-organ damage present
4. Symptoms: Severe headache, confusion, visual impairment, chest pain, dyspnea, nausea/vomiting, anxiety, seizures
- --
HIGH YIELD
Blood Pressure Regulation Mechanisms
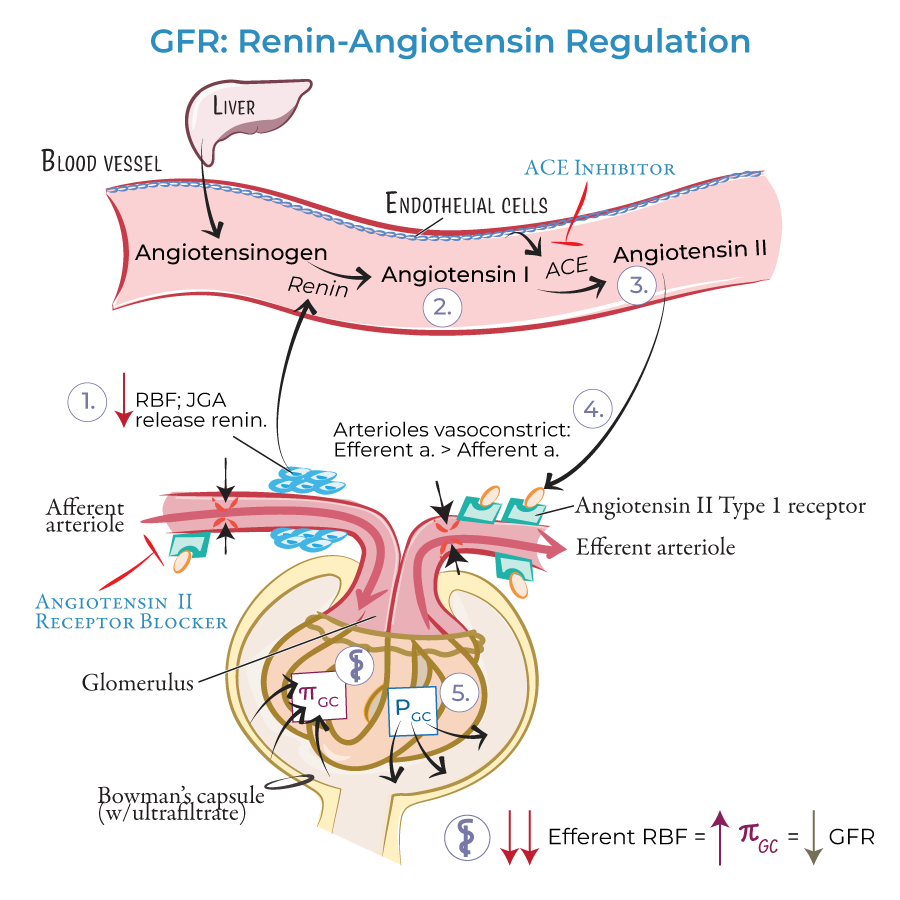
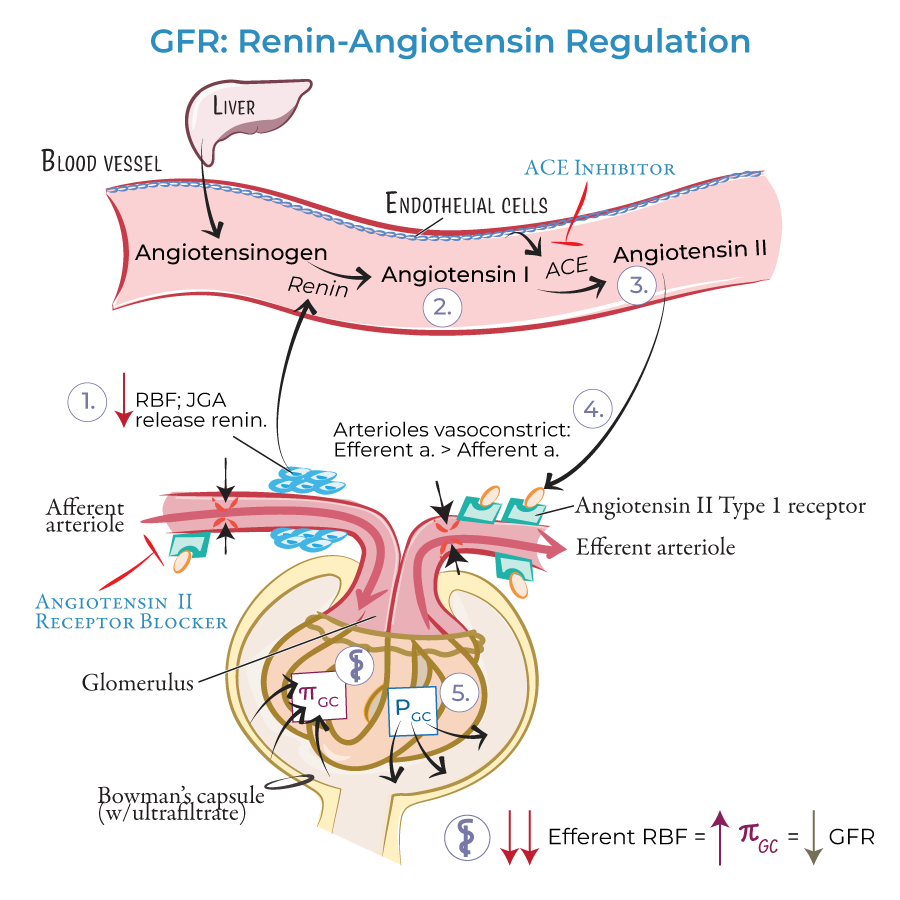
1. Renin-Angiotensin-Aldosterone System (RAAS):
- Key pathway for BP regulation
- Angiotensin-converting enzyme (ACE) converts Angiotensin I to Angiotensin II
- Angiotensin II breaks down bradykinin (a vasodilator)
- ACE inhibitors work by reducing Angiotensin II and increasing bradykinin
- Regulates blood volume through sodium and water retention
- Salt-sensitive individuals develop hypertension with high sodium intake
- Decreased renal perfusion activates RAAS
- Vasodilators: nitric oxide, prostaglandins, histamine, bradykinin
- Vasoconstrictors: angiotensin II, norepinephrine, endothelin, ADH
- Balance determines vascular tone
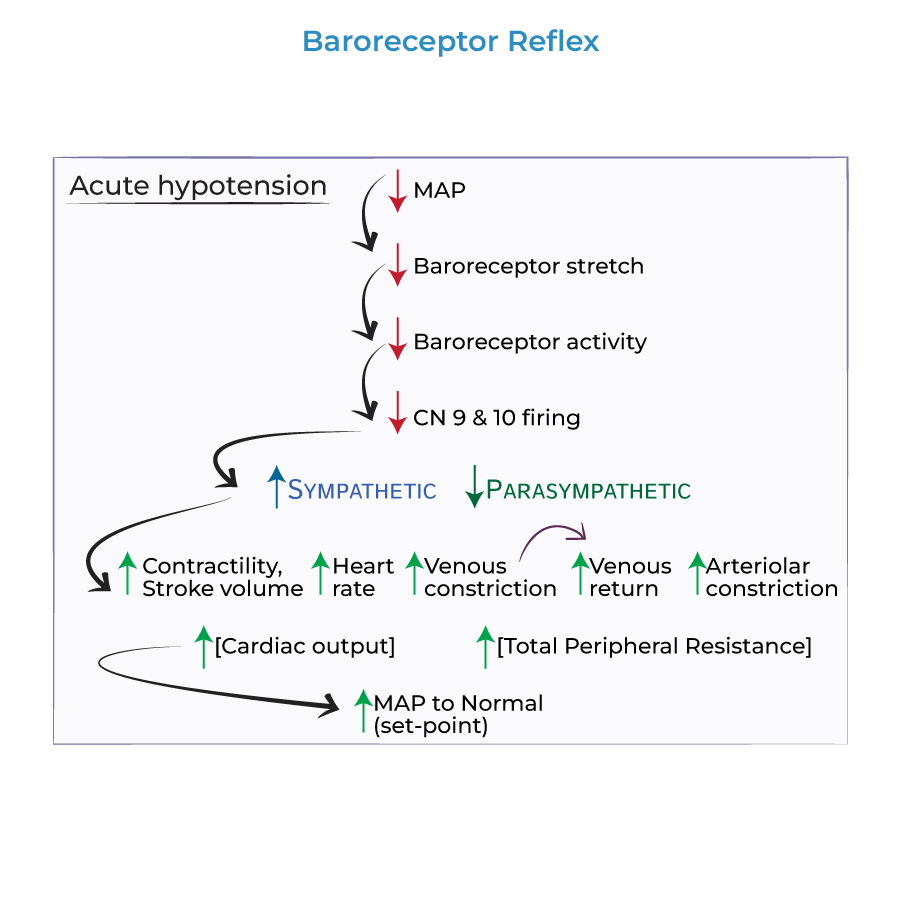
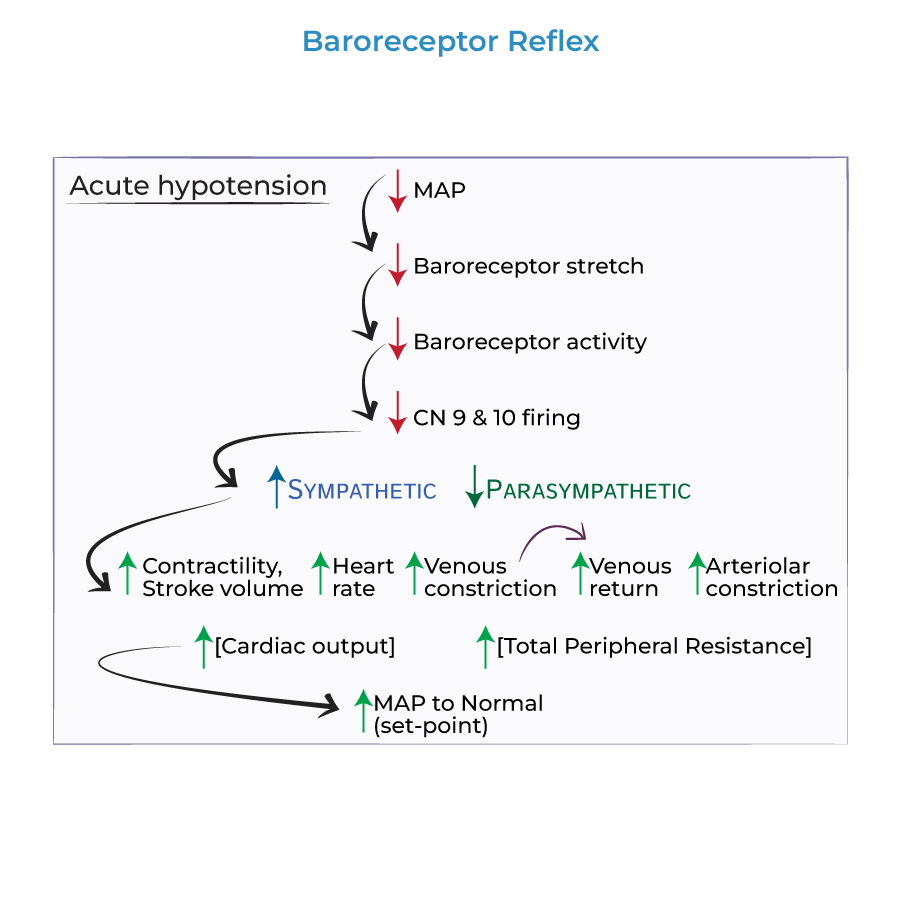
- Short-term regulation of blood pressure
- Located in carotid sinus and aortic arch
- Decreases sympathetic tone when BP increases
Pathophysiology of Hypertension
1. Primary (Essential) Hypertension:
- 90-95% of cases
- Multifactorial: genetic, environmental, dietary factors
- Characterized by increased peripheral resistance
- 5-10% of cases
- Identifiable causes (renal, endocrine, vascular, drug-induced)
- Examples: renal artery stenosis, pheochromocytoma, Cushing's syndrome, primary hyperaldosteronism (Conn's syndrome)
- Obesity increases cardiac output and activates RAAS
- Insulin resistance associated with salt retention
- Sleep apnea increases sympathetic activity
- Alcohol consumption increases blood pressure
- --
Beyond the Tutorial
Pharmacology of Antihypertensives
1. First-line agents:
- Thiazide diuretics
- ACE inhibitors
- Angiotensin receptor blockers (ARBs)
- Calcium channel blockers (CCBs)
- Thiazides: inhibit Na⁺/Cl⁻ cotransporter in distal convoluted tubule, decreasing blood volume
- ACE inhibitors: prevent conversion of angiotensin I to II, reduce aldosterone
- ARBs: block angiotensin II receptor (AT₁), similar effects to ACE inhibitors but without bradykinin increase
- CCBs: inhibit Ca²⁺ influx, causing vasodilation and decreased cardiac contractility
Special Populations
1. Pregnancy:
- Preeclampsia: hypertension with proteinuria after 20 weeks gestation
- First-line treatment: methyldopa, labetalol, or nifedipine
- Contraindicated: ACE inhibitors, ARBs (teratogenic)
- More likely to have isolated systolic hypertension
- Increased sensitivity to volume depletion
- Start with lower doses to avoid orthostatic hypotension
Hypertension Complications
1. Cardiac:
- Left ventricular hypertrophy
- Heart failure
- Coronary artery disease
- Stroke
- Hypertensive encephalopathy
- Chronic kidney disease
- Hypertensive nephrosclerosis
- Aortic dissection
- Aortic aneurysm
- Peripheral arterial disease
Diagnostic Workup
1. Secondary HTN Screening:
- Young patients (<30 years)
- Sudden onset of severe hypertension
- Resistant hypertension (requiring ≥3 medications)
- Lab tests: electrolytes, BUN, creatinine, urinalysis
- Imaging: renal ultrasound, CT angiography when indicated
