USMLE/COMLEX 1 - Heart Murmurs
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX 1 from the Hypertension Overview tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE Step 1 & COMLEX 1
Murmur Basics & General Principles
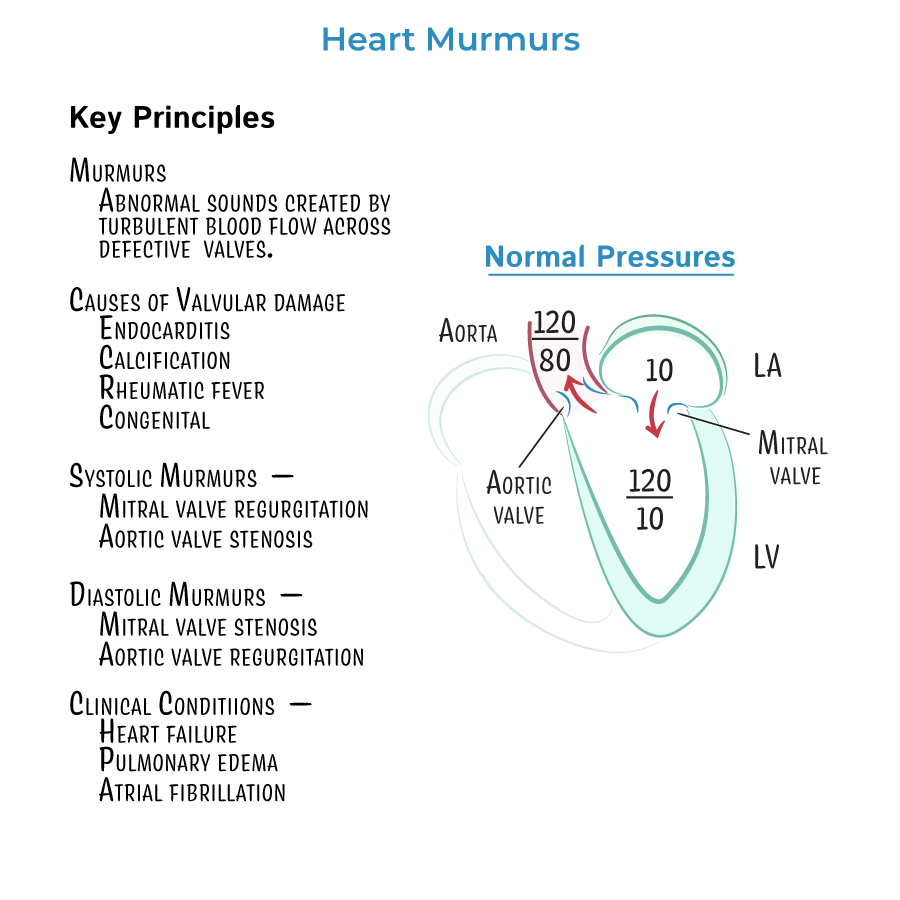
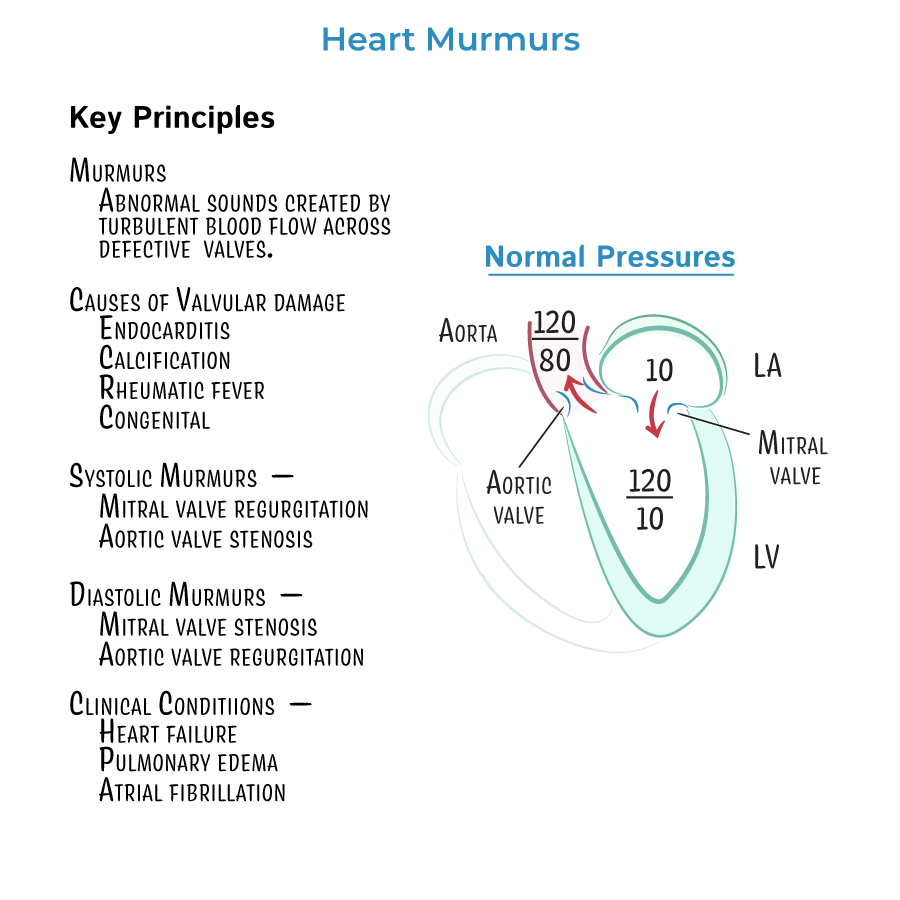
1. Murmurs are due to turbulent blood flow across abnormal valves (stenosis or regurgitation).
2. Systolic murmurs include:
- Aortic stenosis
- Mitral regurgitation
- Mitral valve prolapse
- Aortic regurgitation
- Mitral stenosis
Mitral Regurgitation (MR)
4. Holosystolic murmur heard best at the apex, radiates to axilla.
5. Pathophysiology:
- Regurgitant flow from LV to LA during systole
- Increased LA pressure → pulmonary congestion
- Elevated v-wave on LA pressure tracing
Aortic Regurgitation (AR)
7. Early diastolic, decrescendo murmur best heard at left sternal border.
8. Pathophysiology:
- Blood flows back from aorta to LV during diastole
- Widened pulse pressure
- High systolic, low diastolic aortic pressures
- Corrigan's sign: bounding pulse or “water-hammer pulse”
Aortic Stenosis (AS)
10. Systolic crescendo-decrescendo murmur at right 2nd intercostal space, radiates to carotids.
11. Pathophysiology:
- Fixed obstruction of LV outflow → pressure overload
- LV concentric hypertrophy
- Reduced systolic aortic pressure
Mitral Stenosis (MS)
14. Opening snap followed by low-pitched diastolic murmur heard best at apex, in left lateral decubitus.
15. Pathophysiology:
- Obstructed LA to LV flow during diastole
- Elevated LA pressure, LA hypertrophy → atrial fibrillation
- Decreased LV filling → reduced CO
- --
HIGH YIELD
Clinical Physiology & Graphical Understanding
16. MR:
- Elevated preload, reduced afterload
- Volume overload → eccentric hypertrophy
- Increased stroke volume, increased preload
- Elevated systolic, low diastolic → increased pulse pressure
- High LA pressure → pulmonary edema
- Decreased aortic pressure and stroke volume
- High LV pressure, normal/low aortic pressure → pressure gradient across valve
- Atrial pressure may also rise due to increased afterload
Valve Timing
20. MR and AS → systolic murmurs (between S1 and S2).
21. MS and AR → diastolic murmurs (after S2).
22. VSD and tricuspid regurgitation also cause holosystolic murmurs like MR.
Murmur Characteristics
23. MVP: Mid-systolic click + systolic murmur that increases with Valsalva or standing (decreased preload).
24. AS murmur increases with squatting (increased preload).
25. AR has a “blowing” early diastolic quality, especially with patient leaning forward.
- --
Beyond the Tutorial
26. Murmur Maneuvers:
- Increased preload (squatting, leg raise) intensifies most murmurs except MVP and HOCM.
- Decreased preload (Valsalva, standing) softens most murmurs but intensifies MVP and HOCM.
27. Murmurs and Heart Failure:
- Chronic MR and AR lead to eccentric hypertrophy and eventual left-sided heart failure.
- MS can cause atrial fibrillation and stroke risk due to LA enlargement and stasis.
28. Common Associations:
- Rheumatic fever → MS, MR
- Aging and calcification → AS
- Connective tissue disorders (e.g., Marfan) → MVP, AR
