USMLE/COMLEX 1 - H. pylori Infection
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Helicobacter pylori tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX-USA Level 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX-USA Level 1.
- --
VITAL FOR USMLE/COMLEX 1
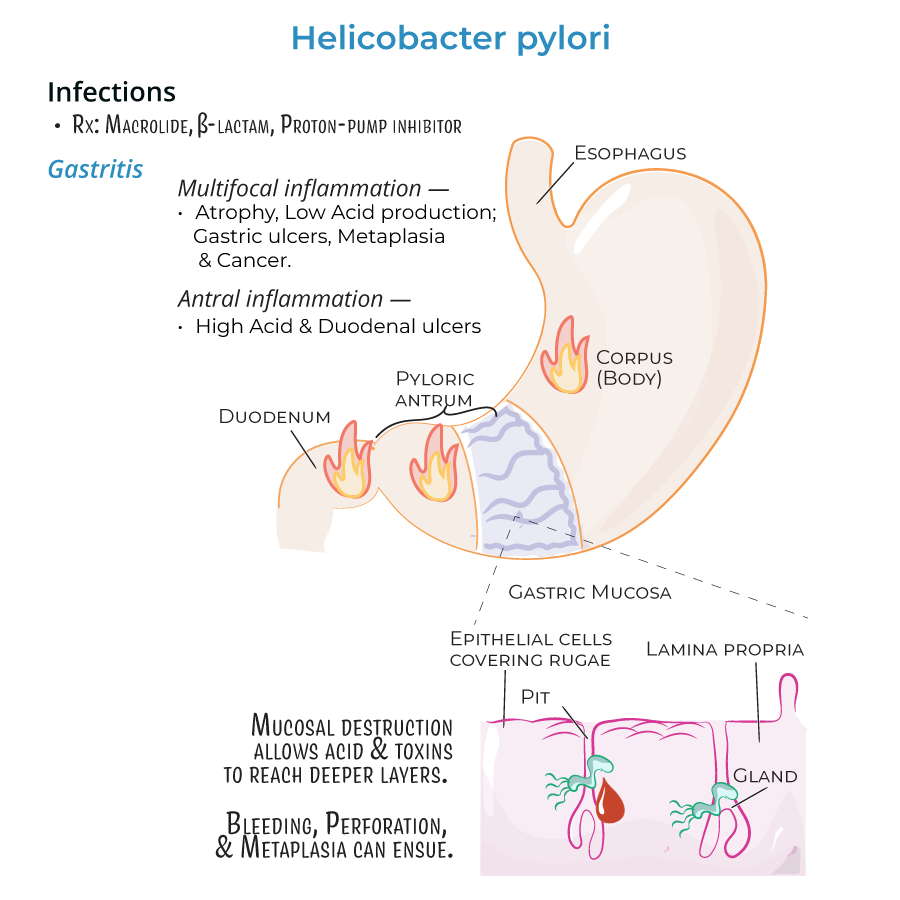
Helicobacter pylori - Basic Characteristics
1. Spiral, Gram-negative rods that can appear as coccoid in older cultures.
2. Catalase, oxidase, and urease positive.
3. Microaerobic: Grows in conditions of reduced oxygen and increased carbon dioxide.
4. Human-to-human transmission; typically acquired in childhood with symptoms in adulthood.
5. Causes life-long colonization of the stomach.
Virulence Factors
1. Urease converts urea to ammonia and bicarbonate to neutralize gastric acids.
2. Multiple flagella provide corkscrew motility to penetrate gastric mucus.
3. Mucinase production allows bacteria to migrate through viscous stomach mucus.
4. Vacuolating cytotoxin A (VacA) promotes pore formation and induces host cell death.
5. Cytotoxin-associated gene A (cagA) promotes tissue changes and T-cell apoptosis.
6. Type IV secretion system injects cagA effector protein into host cells.
Clinical Manifestations
1. Gastritis: Inflammation of stomach lining with neutrophil infiltration.
2. Peptic ulcers: Develop in 10-20% of patients with gastritis.
3. Gastric adenocarcinoma: Occurs in 1-2% of chronic infections.
4. MALT lymphoma: Monoclonal B-cell proliferation in gastric lymphoid tissue.
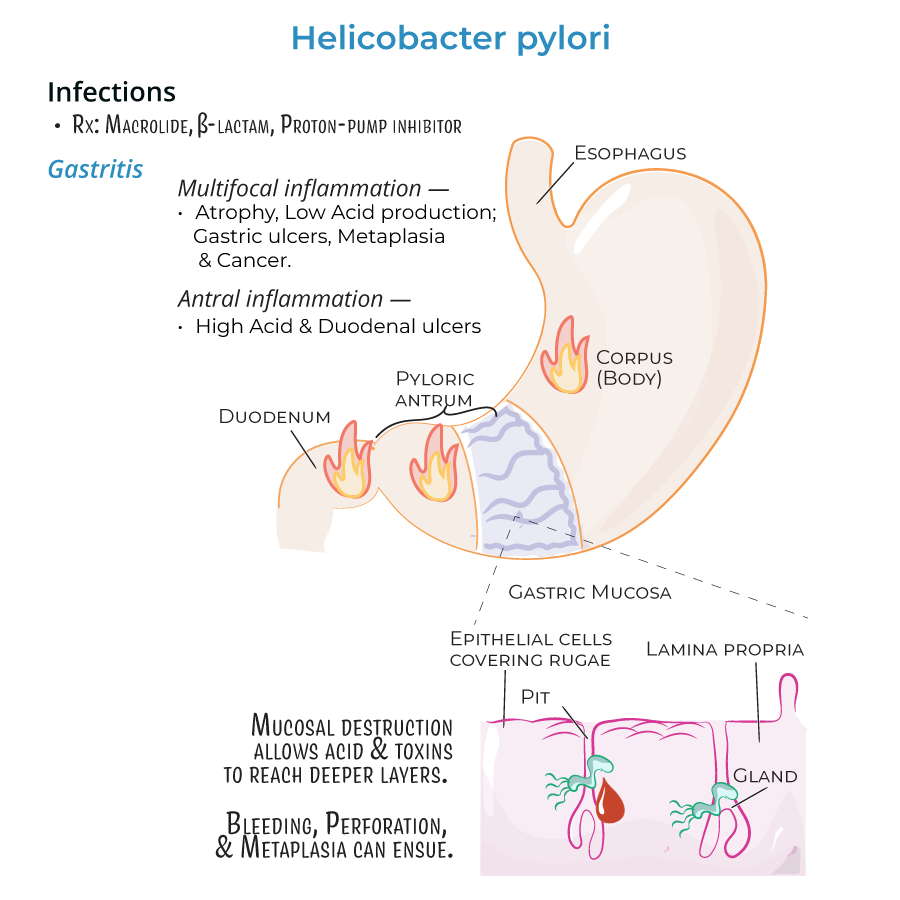
Treatment
1. Standard therapy includes macrolides, beta-lactams, and proton-pump inhibitors.
- --
HIGH YIELD
Pathophysiology of Infection
1. Infection triggers host production of IL-8, a pro-inflammatory cytokine that recruits neutrophils.
2. Bacteria protect themselves by producing superoxide dismutase and catalase to detoxify reactive oxygen species.
3. Lipopolysaccharide endotoxin has lower toxicity compared to other Gram-negative bacteria.
4. Inflammation can be localized (usually to pyloric antrum) or widespread.
Peptic Ulcers
1. Ulcers can occur in the stomach or duodenum (first portion of small intestine).
2. Result from inflammation eroding stomach tissues.
Gastric Adenocarcinoma
1. Develops when chronic inflammation leads to metaplasia.
2. Over time, gastric mucosa is replaced by fibrotic tissue that can become neoplastic.
3. Reduced gastric acid secretion is associated with higher risk of adenocarcinoma.
MALT Lymphoma
1. Lymphoid tissues infiltrate the stomach in response to H. pylori infection.
2. In some cases, monoclonal B cells proliferate and form MALT lymphomas.
Infection Patterns and Consequences
1. Antral gastritis is associated with increased acid production and duodenal ulcers.
2. Pangastritis (multifocal inflammation) is associated with atrophy, reduced acid production, and risk of gastric cancer.
3. H. pylori destroys mucosa, allowing acids and toxins access to deeper tissues.
4. Severe ulceration can lead to bleeding, perforation, and metaplasia.
- --
Beyond the Tutorial
Diagnostic Testing
1. Urea breath test: Detects urease activity; patient ingests labeled urea.
2. Stool antigen test: Non-invasive detection of H. pylori antigens.
3. Serologic tests: Detect antibodies, but cannot distinguish active from past infection.
4. Rapid urease test: Performed on gastric biopsy specimens.
5. Histology with special stains: Silver stains can visualize the organism.
Risk Factors for Infection
1. Low socioeconomic status.
2. Crowded living conditions.
3. Inadequate sanitation and unsafe water.
4. Family history of infection.
Complications of Treatment
1. Antibiotic resistance is increasing globally.
2. Triple and quadruple therapy regimens may be necessary.
3. Bismuth-containing regimens for resistant strains.
Special Populations
1. Higher prevalence in developing countries (>80%) compared to developed nations (~30%).
2. Association with iron deficiency anemia, especially in children.
3. Possible protective effect against esophageal diseases (GERD, Barrett's esophagus).
