USMLE/COMLEX 1 - Gastritis & Peptic Ulcer Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Gastritis & Peptic Ulcer Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
Gastritis
1. Inflammation of the gastric mucosa; can be diffuse or multi-focal.
2. Most common causes: H. pylori infection and NSAID use.
3. Signs and symptoms: Epigastric pain, GI bleeding, nausea, vomiting; many patients are asymptomatic.
4. Diagnosis: Upper endoscopy with biopsies, urea breath test, and stool antigen test for H. pylori.
5. Treatment: Proton pump inhibitors, NSAID discontinuation, and H. pylori eradication with antibiotics.
Peptic Ulcer Disease (PUD)
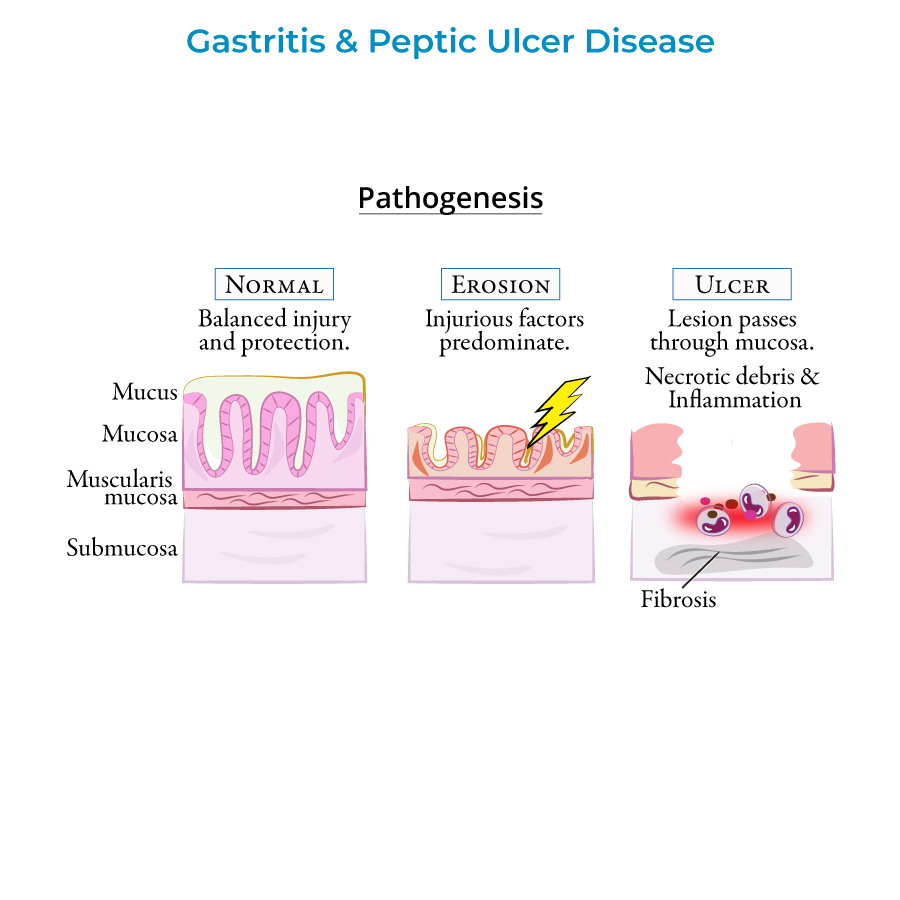
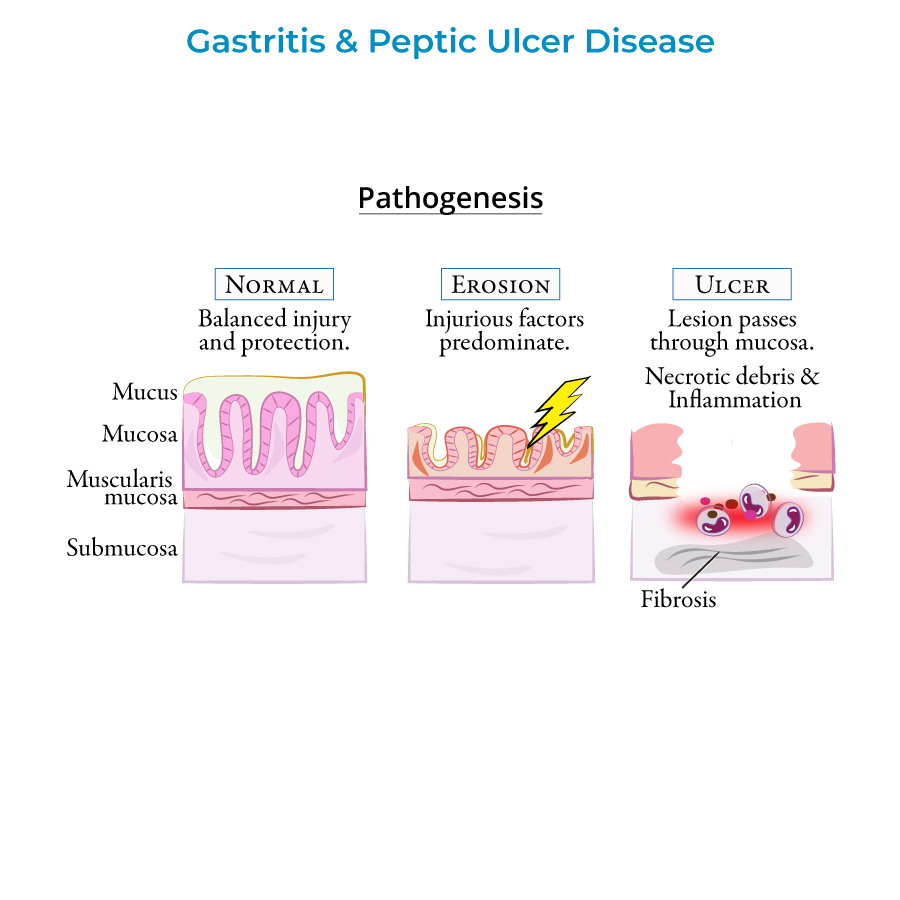
1. Ulcers in stomach/duodenum that penetrate mucosa to reach deeper layers of GI tract.
2. Types: Gastric ulcers (reduced mucosal protection) vs. duodenal ulcers (increased acid production).
3. H. pylori present in 70% of gastric ulcers and 90% of duodenal ulcers.
4. Top complications: Hemorrhage (most common), perforation (emergency), and gastric outlet obstruction.
5. Risk factors: H. pylori, NSAIDs, and cigarette smoking (not stress or spicy foods).
- --
HIGH YIELD
Gastritis Types
1. Acute gastritis: Sudden insult to gastric mucosa, commonly from NSAIDs, aspirin, and alcohol.
2. Stress ulcers: Curling ulcers (systemic burns, hypovolemia) vs. Cushing ulcers (brain injury, increased vagal stimulation).
3. Chronic gastritis: Often due to H. pylori, can lead to atrophy (loss of gastric glands and folds).
4. H. pylori: Gram-negative spirochete bacterium, raises stomach pH via urease, classified as class I carcinogen.
5. Autoimmune gastritis: T-cell mediated destruction of parietal cells, can lead to pernicious anemia.
Peptic Ulcer Disease Characteristics
1. Gastric ulcers: Reduced mucosal protection, higher risk of malignancy (5-10%).
2. Duodenal ulcers: Typically benign, caused by increased acid production.
3. Clinical pattern: Gastric ulcer pain increases with eating (weight loss); duodenal ulcer pain relieved by eating (possible weight gain).
4. Perforation signs: Sudden abdominal pain, tachycardia, abdominal rigidity, pneumoperitoneum (free air under diaphragm).
5. Diagnostic approach:
- Age <60 without alarming symptoms: Non-invasive H. pylori testing, PPI trial
- Age >60 or with alarming symptoms (weight loss, anemia, bloody stools, dysphagia): Upper endoscopy
- --
Beyond the Tutorial
Gastritis
1. Histopathology of acute gastritis: Interstitial hemorrhage, capillary dilation, necrotic debris with fibrin and neutrophils.
2. Zollinger-Ellison syndrome: Rare cause of peptic ulcer disease due to gastrin-secreting tumors (gastrinomas).
3. Helicobacter pylori virulence factors: CagA, VacA, and adhesins contribute to pathogenicity.
4. Reactive gastropathy: Chemical-induced injury without significant inflammation, often from bile reflux or NSAIDs.
5. Ménétrier disease: Rare hyperplastic gastropathy with protein loss and increased risk of gastric cancer.
Peptic Ulcer Disease
1. NSAID-induced ulcers: Mechanism involves inhibition of both COX-1 (protective) and COX-2 (inflammatory).
2. Triple therapy for H. pylori: PPI + clarithromycin + amoxicillin/metronidazole.
3. Quadruple therapy: PPI + bismuth + tetracycline + metronidazole (for resistant H. pylori).
4. Dieulafoy lesion: Vascular malformation that can mimic peptic ulcer bleeding.
5. Cameron lesions: Linear erosions at hiatal hernia, can cause occult bleeding and anemia.
