USMLE/COMLEX 1 - Diabetes Mellitus Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Diabetes Mellitus - Pathophysiology tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 1. The "3 P's": Polyuria, polydipsia, and polyphagia.
2. Pathophysiologic sequence:
1. The "3 P's": Polyuria, polydipsia, and polyphagia.
2. Pathophysiologic sequence:
- --
VITAL FOR USMLE/COMLEX 1
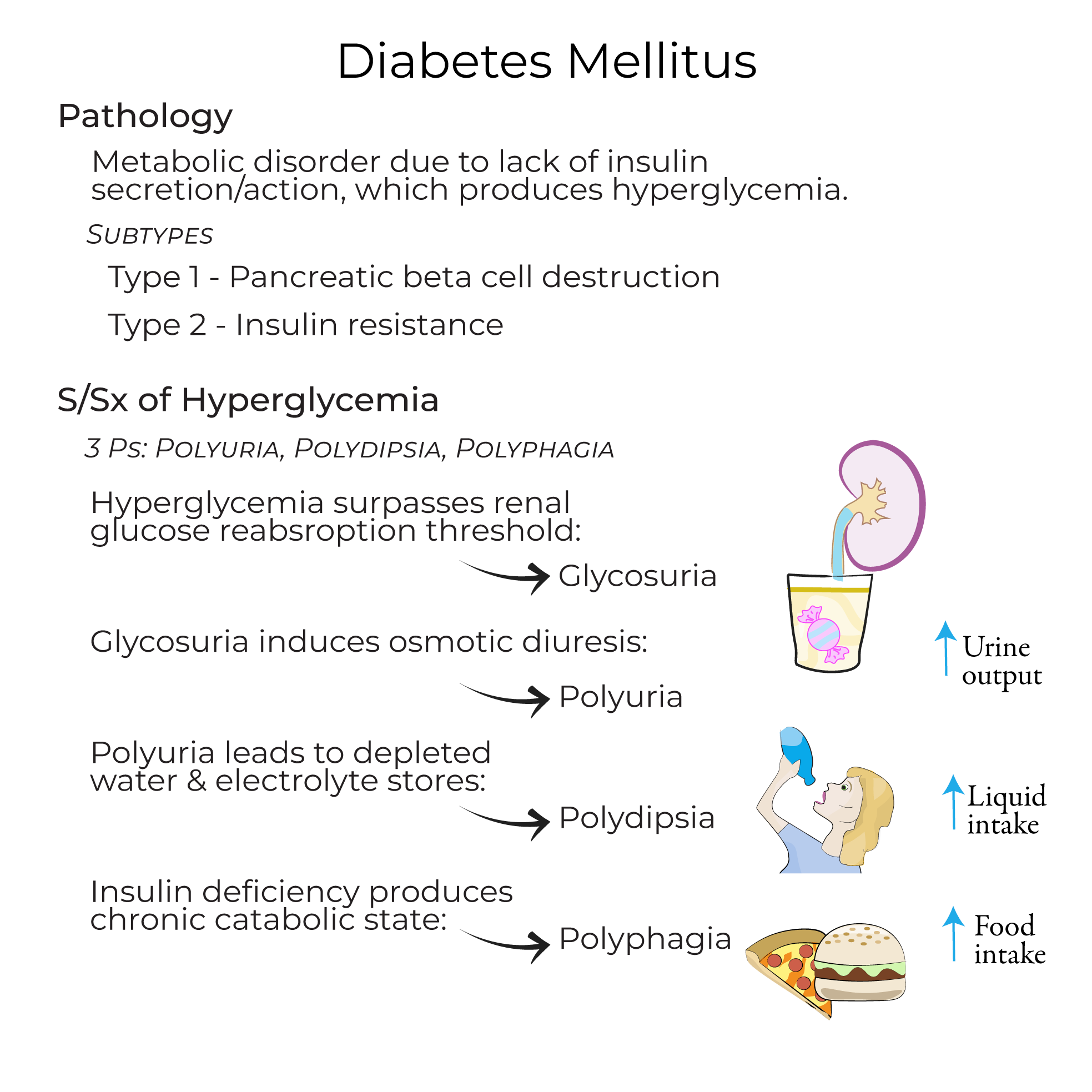
Diabetes Mellitus - Overview
1. Definition: A collection of metabolic disorders in which a lack of insulin secretion and/or insulin action leads to hyperglycemia.
2. Chronic hyperglycemia consequences: Produces dysfunction and damage of multiple organs, including the heart, kidneys, eyes, and peripheral nervous system.
3. Diagnosis: Random plasma glucose level of 200+ mg/dL or a fasting plasma glucose level of 126+ mg/dL.
4. Subtypes: Type 1, Type 2, Monogenic diabetes (including MODY), Secondary diabetes, and Gestational diabetes.
Type 1 Diabetes
1. Prevalence: Accounts for 5-10% of all diabetes mellitus cases.
2. Pathophysiology: Caused by autoimmune destruction of pancreatic beta cells; insulitis is often visible in pancreatic tissue samples.
3. Autoimmune markers: Islet autoantibodies including those targeting insulin, GAD65, ZnT8, and IA2.
4. Genetic factors: Associated with variations in HLA alleles, particularly class II DR and DQ cell-surface proteins.
5. Treatment: Requires exogenous insulin administration due to absolute insulin deficiency.
Type 2 Diabetes
1. Prevalence: Represents 90-95% of all diabetes cases.
2. Pathophysiology: Characterized by peripheral tissue insulin resistance and relative insulin deficiency due to mild beta cell destruction.
3. Histopathology: Amyloid deposits (originally called "hyaline") visible in pancreatic tissue.
4. Insulin resistance mechanism: Loss of Glut-4 receptors in peripheral tissues.
5. Risk factors: Associated with obesity, central fat distribution, sedentarism, stress, and inflammation.
Classic Symptoms of Hyperglycemia
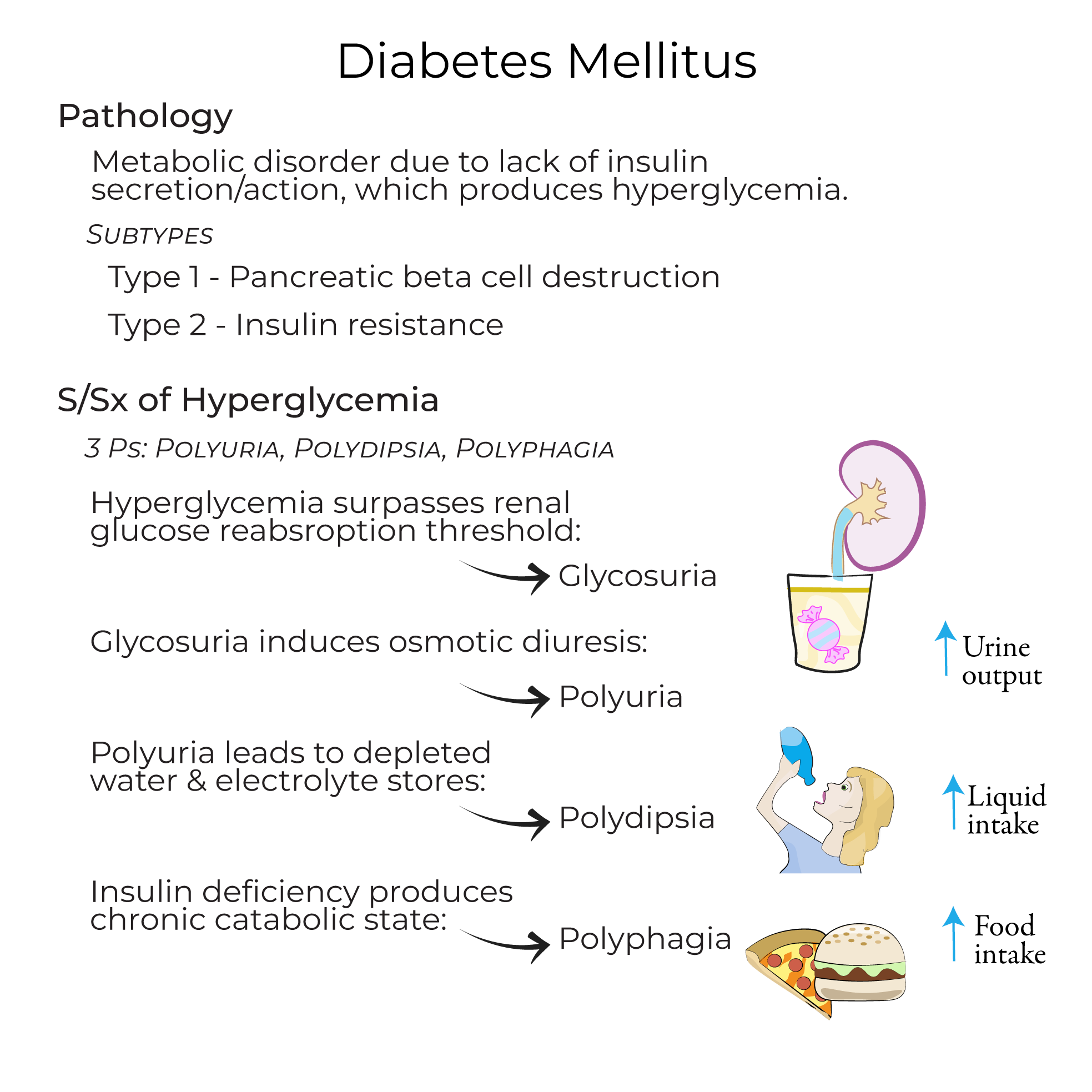 1. The "3 P's": Polyuria, polydipsia, and polyphagia.
2. Pathophysiologic sequence:
1. The "3 P's": Polyuria, polydipsia, and polyphagia.
2. Pathophysiologic sequence:
- Glycosuria: Hyperglycemia surpasses renal glucose reabsorption threshold
- Polyuria: Glycosuria induces osmotic diuresis
- Polydipsia: Depleted water and electrolyte stores from polyuria
- Polyphagia: Chronic catabolic state causes increased hunger
- --
HIGH YIELD
Type 1 Diabetes
1. T-cell mediation: T-cells with failed self-tolerance for islet antigens mediate beta cell destruction.
2. Environmental factors: Potential triggers include viral infections (particularly enterovirus) and diet during infancy and childhood.
3. Clinical course: Onset often during childhood, but not exclusively; shows progressive reduction in insulin levels as more cells are destroyed.
4. Terminology note: No longer referred to as "juvenile diabetes" to avoid misdiagnosis based on age.
Type 2 Diabetes
1. Genetics: Has strong genetic associations which are polygenic with complex inheritance patterns.
2. Age of onset: Historically adult-onset but increasingly common in children due to higher rates of childhood obesity and inactivity.
3. Insulin dynamics: Patients may initially have elevated insulin levels in response to insulin resistance, but levels eventually fall as pancreatic cells can't keep up.
4. Clinical presentation: Many patients are asymptomatic with diagnosis occurring after routine blood testing.
5. Treatment options: May include diet and exercise, Metformin, insulin, GLP-1 receptor agonists, or SGLT2-inhibitors.
Prediabetes
1. Definition: Condition where glucose levels are elevated but not high enough to be classified as diabetes.
2. Epidemiology: The CDC reports that 1 in 3 Americans is pre-diabetic.
3. Clinical significance: Pre-diabetic patients are at high risk for Type 2 diabetes and cardiovascular complications.
4. Management: Patients are advised to take preventive steps such as increasing physical activity and losing weight.
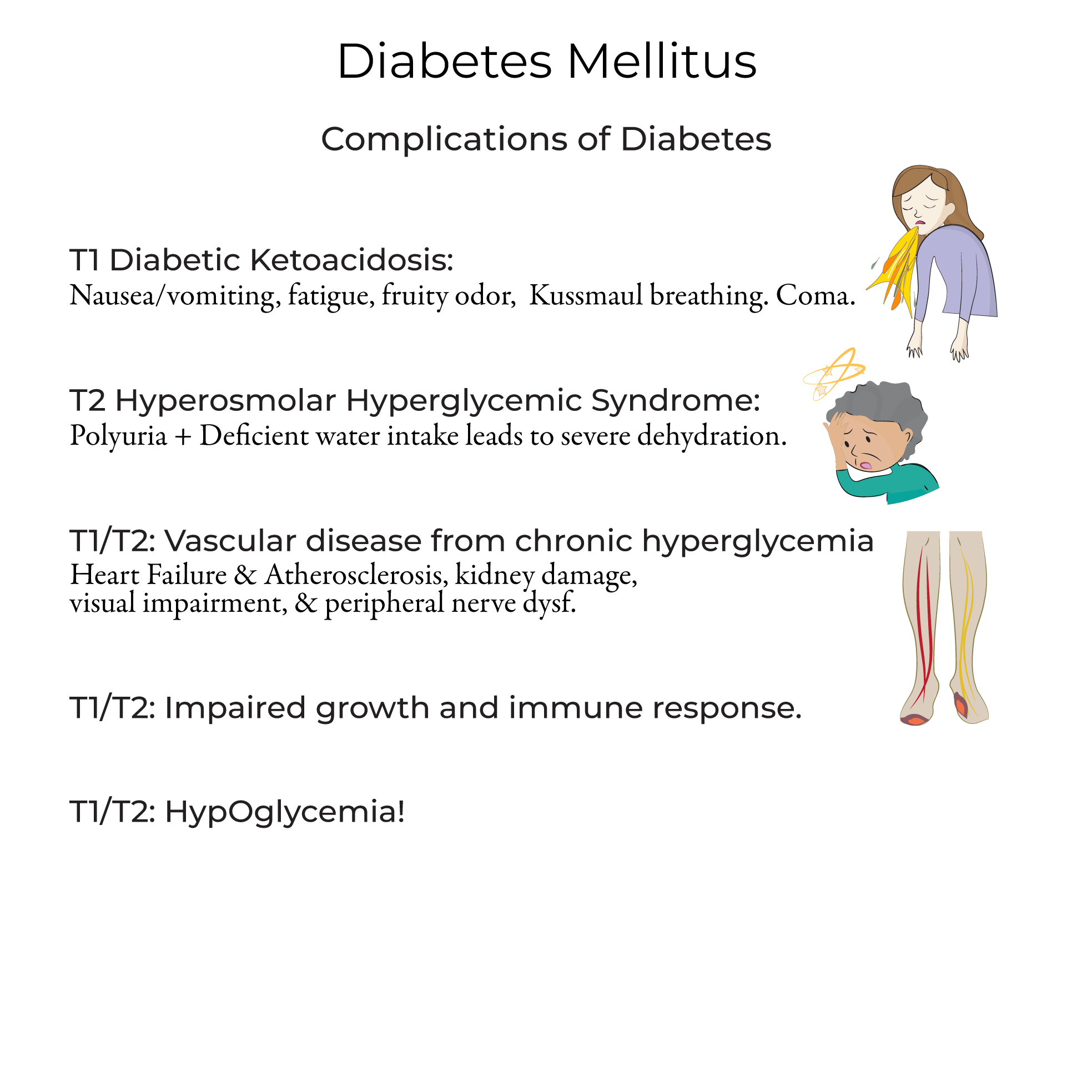
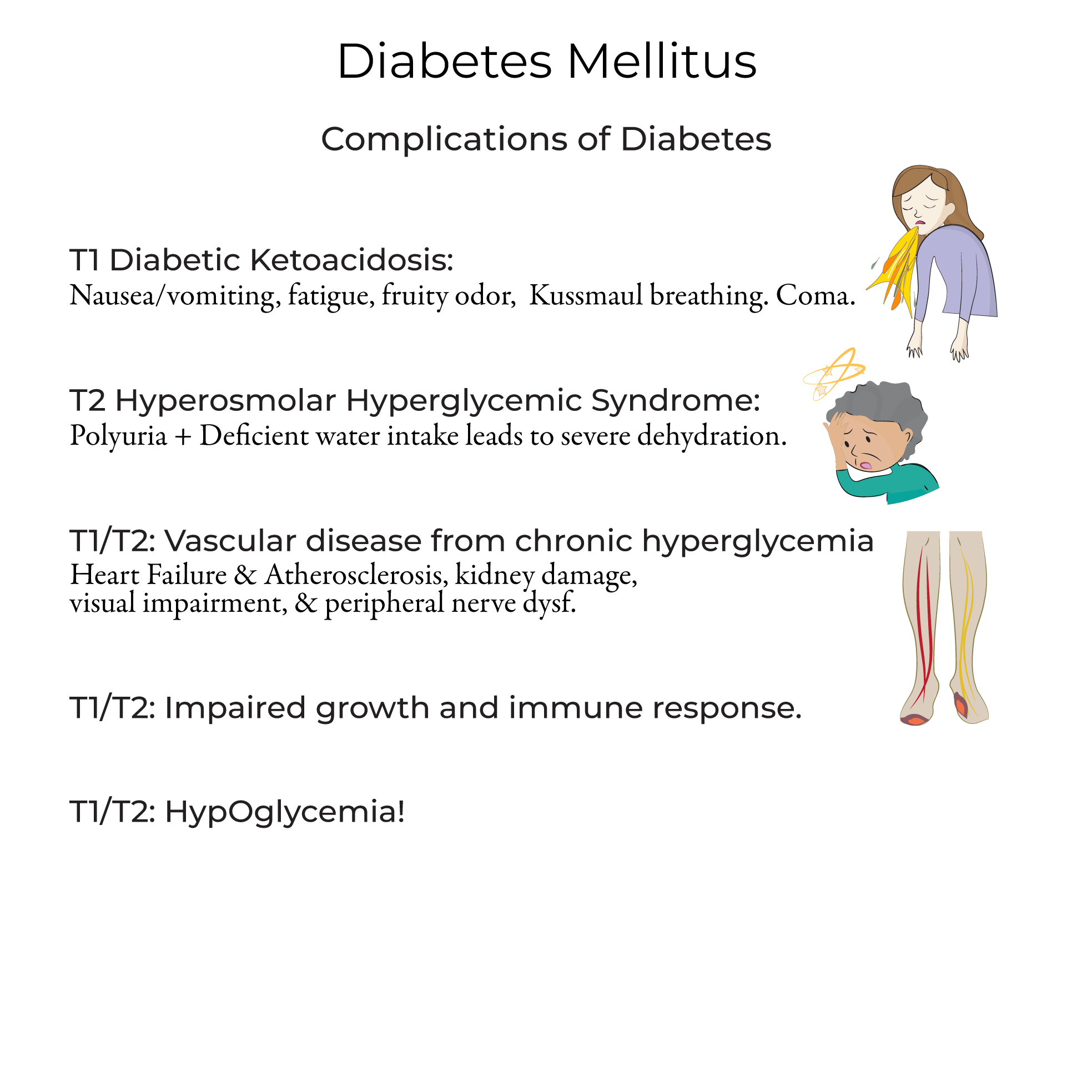
Complications of Diabetes
1. Diabetic Ketoacidosis (DKA):
- Associated with under-treated Type 1 diabetes
- Symptoms include nausea, vomiting, fatigue, "fruity" odor, and Kussmal breathing
- Management includes fluids, electrolytes, and insulin
- More common in Type 2 diabetes
- Occurs when a patient with polyuria is also deficient in water intake
- Has a mortality rate of up to 20% - higher than DKA
- Treatment requires saline, insulin, and electrolytes
- Patients at higher risk due to chronic hyperglycemia
- Can lead to heart failure, atherosclerosis, kidney damage, visual impairment, and peripheral nerve dysfunction
- Impaired growth in children
- Increased susceptibility to infection due to immune suppression
- Hypoglycemia due to missing meals, excessive exertion, or excessive insulin
- --
Beyond the Tutorial
Pathophysiology and Biochemistry
1. Insulin signaling pathway: Detailed molecular mechanisms of insulin receptor substrate, PI3K, and GLUT4 translocation.
2. Hexosamine pathway: Role in diabetic complications through protein glycosylation.
3. Polyol pathway: Sorbitol accumulation and its contribution to microvascular complications.
Diagnostic Criteria and Testing
1. HbA1c: Role in diagnosis (≥6.5%) and monitoring of diabetes.
2. Glucose tolerance test: Methodology and interpretation of results.
3. C-peptide testing: Use in differentiating Type 1 from Type 2 diabetes.
Pharmacology
1. Insulin formulations: Pharmacokinetics of rapid-acting, short-acting, intermediate-acting, and long-acting insulins.
2. Oral hypoglycemic agents: Mechanism of action, side effects, and contraindications of sulfonylureas, thiazolidinediones, DPP-4 inhibitors.
3. Drug interactions: Important interactions between antidiabetic medications and other commonly prescribed drugs.
Complications - Detailed Pathophysiology
1. Advanced glycation end products (AGEs): Formation and role in diabetic complications.
2. Diabetic nephropathy progression: From microalbuminuria to end-stage renal disease.
3. Diabetic foot ulcers: Pathophysiology involving neuropathy, vascular insufficiency, and immunocompromise.
