USMLE/COMLEX 1 - Cortisol Physiology & Pathology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Cortisol Physiology & Pathology tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 1
Definition and Classification
1. Hypercortisolism = Elevated levels of cortisol, also known as Cushing's Syndrome.
2. ACTH-dependent: elevated cortisol is caused by elevated ACTH.
3. ACTH-independent: elevated cortisol is not caused by elevated ACTH.
4. Exogenous glucocorticoids are responsible for most cases of ACTH-Independent hypercortisolism.
5. Must rule out physiologic causes: pregnancy, alcoholism, anorexia, obesity, depression, and uncontrolled diabetes.
Cortisol Regulation
1. HPA axis consists of hypothalamus, pituitary gland, and adrenal glands.
2. Hypothalamus secretes Corticotropin-Releasing Hormone (CRH) to anterior pituitary.
3. CRH triggers release of Adrenocorticotrophic Hormone (ACTH) from corticotrophs.
4. ACTH stimulates cortisol release from the zona fasciculata of adrenal cortex.
5. Negative feedback: Cortisol inhibits both hypothalamus and pituitary.
6. Stress is a key trigger for CRH release from the hypothalamus.
Screening & Diagnosis
1. 24-hour urine samples, midnight salivary samples, or dexamethasone suppression test.
2. If cortisol levels are elevated and/or not suppressed by dexamethasone, Cushing's syndrome is likely.
3. Measure plasma ACTH levels to determine cause of hypercortisolism.
4. Low/suppressed ACTH: Consider adrenal tumor (adenoma more common than carcinoma).
5. Elevated/not suppressed ACTH: ACTH-dependent hypercortisolism.
6. Cushing's Disease = pituitary tumor (adenoma) secreting ACTH (most common endogenous form).
7. Ectopic ACTH = non-pituitary tumors (small cell lung cancer, bronchial tumors).
- --
HIGH YIELD
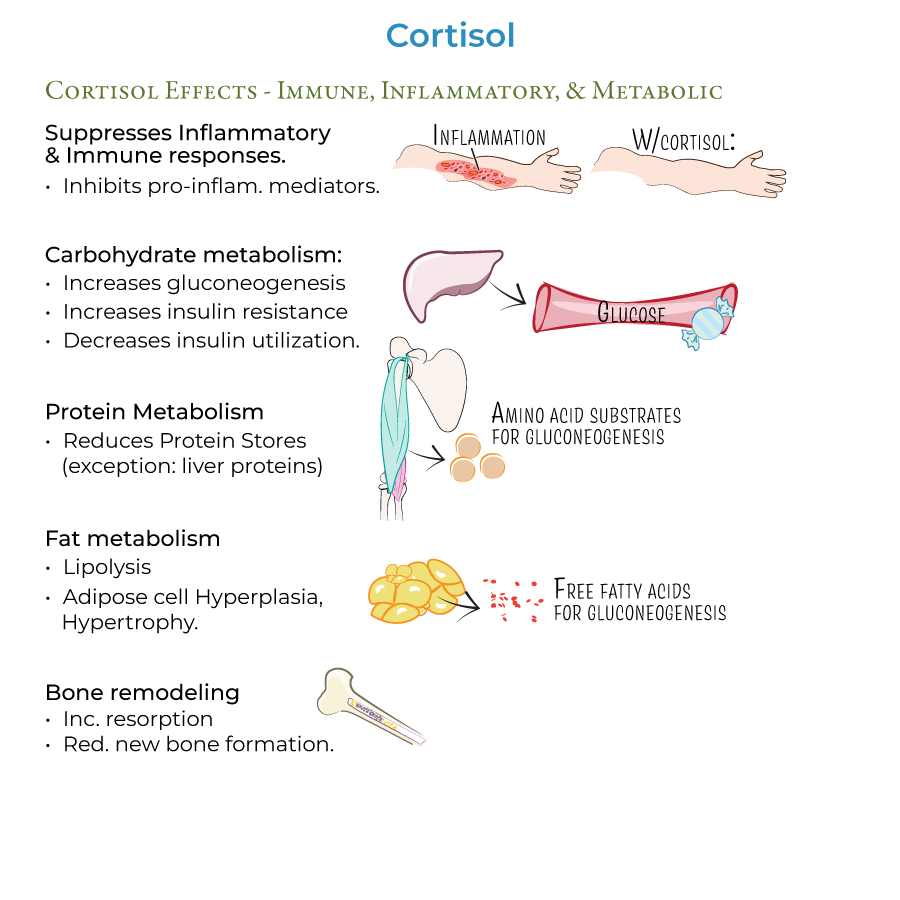
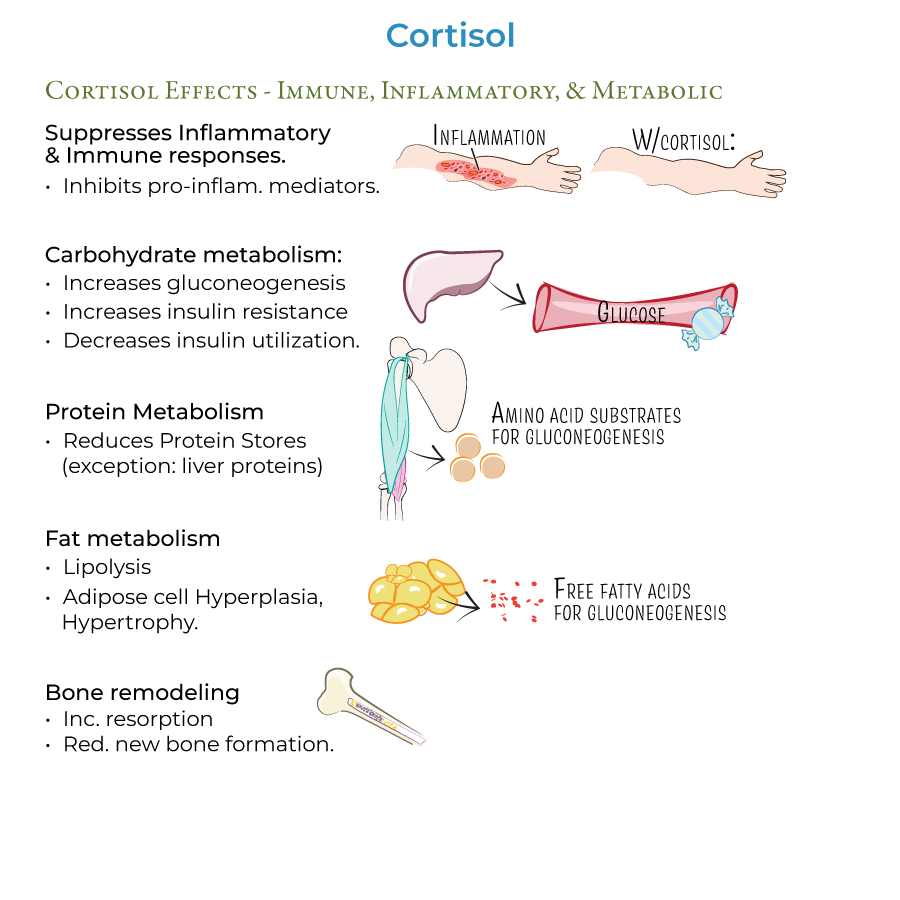
Physiologic Roles of Cortisol
1. Suppression of inflammatory and immune responses via multiple pathways.
2. Increases carbohydrate metabolism: increases gluconeogenesis and insulin resistance.
3. Increases protein metabolism and decreases protein stores (except in liver).
4. Increases fat metabolism: increases lipolysis but paradoxically associated with obesity.
5. Increases bone resorption and reduces formation of new bone tissue.
6. Approximately 85% of cortisol is bound to plasma proteins, giving it a long half-life.
7. Secretion is pulsatile and circadian with highest levels upon waking.
Clinical Features of Cushing's Syndrome
1. Moon facies: rounded shape of face and neck due to fat accumulation.
2. Central/truncal obesity with "buffalo hump" between shoulders.
3. Muscle atrophy particularly in extremities, making limbs appear thin.
4. Red or purple striae on abdomen, breasts, thighs, and buttocks.
5. Hypertension via increased cardiac contractility and extracellular fluid volume.
6. Hyperglycemia that may progress to diabetes mellitus.
7. Immunosuppression increasing vulnerability to infections (TB, fungal).
8. Emotional/psychiatric disturbances including irritability or impaired memory.
9. Hirsutism and menstrual irregularities due to excess androgen (in adrenal tumors).
10. Impaired linear growth in children.
Diagnostic Workup
1. Inferior petrosal sampling helps determine source of excess ACTH.
2. Central ACTH > peripheral: likely pituitary tumor (Cushing's Disease).
3. Central ACTH ≤ peripheral: likely ectopic (non-pituitary) tumor.
4. In Cushing's Disease, HPA axis is dysfunctional and no longer responsive to negative feedback.
5. Treatment of Cushing's Disease involves removal of pituitary tumor or bilateral adrenalectomy.
- --
Beyond the Tutorial
Complications and Related Conditions
1. Nelson syndrome: potential complication after bilateral adrenalectomy, with pituitary tumor, headaches, elevated ACTH, and hyperpigmentation.
2. Adrenal insufficiency may occur after treatment, requiring hormone replacement therapy.
3. Bilateral macro- and micro-nodular adrenal hyperplasias are rare causes of ACTH-independent Cushing's syndrome.
4. Pseudo-Cushing's states can mimic true Cushing's but are caused by conditions like alcoholism, depression, and obesity.
5. Cyclic Cushing's syndrome with periods of normal cortisol alternating with hypercortisolism.
Treatment Considerations
1. Ketoconazole and metyrapone can be used to block cortisol synthesis as medical therapy.
2. Mifepristone (glucocorticoid receptor antagonist) useful for hyperglycemia management.
3. Radiotherapy may be used for pituitary tumors when surgery is not curative.
4. Pasireotide specifically targets corticotroph adenomas in Cushing's Disease.
5. Long-term follow-up is essential as recurrence is common.
