USMLE/COMLEX 1 - Atherosclerosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Atherosclerosis Tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 1
Definitions and Histology
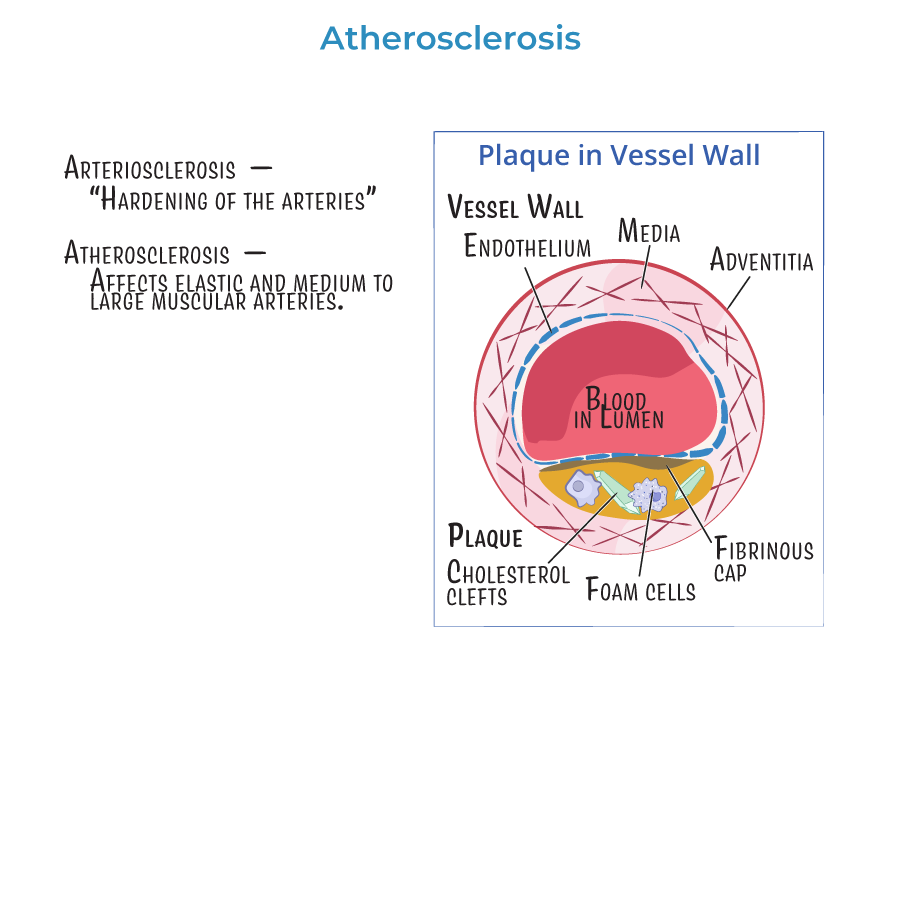
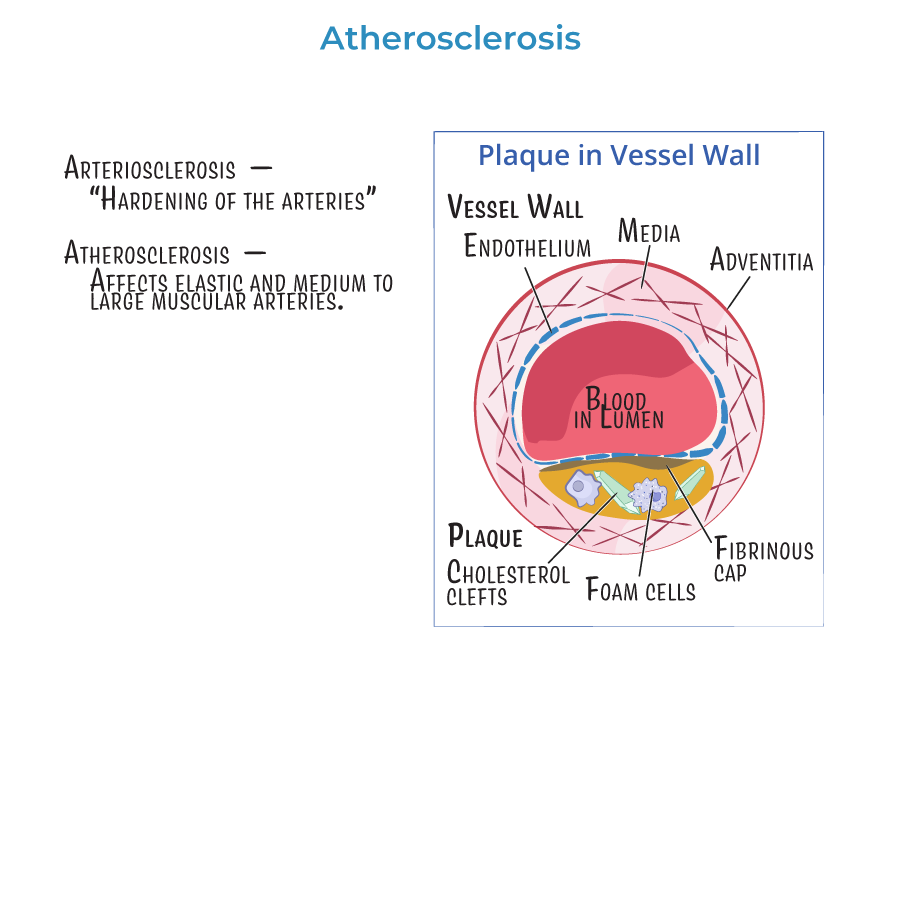
1. Atherosclerosis is a specific type of arteriosclerosis involving elastic and large-to-medium muscular arteries.
2. Vessel wall structure includes tunica intima (endothelial cells), tunica media (smooth muscle cells), and adventitia (outer connective tissue layer).
3. Foam cells are lipid-laden macrophages seen in atherosclerotic plaques.
4. A fibrous cap overlays the plaque; cap integrity determines plaque stability and risk of rupture.
Pathogenesis
5. Endothelial injury and dysfunction are the initiating events of atherosclerosis, triggering inflammation and increased vascular permeability.
6. Fatty streaks are early lesions formed by macrophages and smooth muscle cells engulfing lipids.
7. Mature atheromas consist of a fibrous cap (smooth muscle cells and collagen) and a necrotic lipid core (extracellular and intracellular lipids, macrophages, T cells, debris).
8. Smooth muscle cells stabilize plaques by depositing collagen; inflammatory cells destabilize plaques by degrading the matrix.
Risk Factors
9. Major modifiable risk factors for atherosclerosis include hyperlipidemia (especially elevated LDL), hypertension, smoking, and diabetes mellitus.
10. Non-modifiable risk factors include age, male gender, and family history.
11. Hypercholesterolemia, particularly elevated LDL, promotes plaque formation through cholesterol accumulation in vessel walls.
Clinical Consequences
12. Atherosclerosis leads to coronary artery disease (CAD), myocardial infarction, stroke, aortic aneurysm, and peripheral vascular disease (PVD).
13. Vessel stenosis causes ischemia and organ dysfunction; vessel wall weakening may cause aneurysm, dissection, or rupture.
14. C-reactive protein (CRP) is a marker of inflammation that correlates with cardiovascular risk.
- --
HIGH YIELD
Detailed Pathogenesis
1. Endothelial cells respond to injury by releasing cytokines, chemokines, and pro-coagulant factors.
2. Hemodynamic stresses (e.g., turbulent blood flow) are significant triggers of endothelial injury, especially at arterial branch points like the carotid bifurcation and posterior abdominal aorta.
3. LDL accumulation in the intima stimulates further macrophage recruitment and foam cell formation.
4. Cholesterol crystals found within plaques contribute to further inflammation and injury.
5. Chronic inflammation in atherosclerosis involves macrophages, T lymphocytes, cytokines (especially IL-1), and triggers a positive feedback loop of vessel wall damage.
6. Smooth muscle cells migrate from the media to the intima, proliferate, and secrete extracellular matrix proteins, notably collagen.
Histology and Morphology
7. Fatty streaks are composed mainly of lipid-laden macrophages and are reversible early in disease.
8. Advanced plaques show cholesterol clefts, foam cells, fibrous caps, and necrotic lipid cores.
9. Unstable plaques have thin fibrous caps and are more prone to rupture, causing thrombosis.
Clinical Settings and Monitoring
10. Measurement of CRP levels can help assess systemic inflammation and cardiovascular risk.
11. Statins lower cholesterol by inhibiting HMG-CoA reductase and are first-line therapy to reduce cardiovascular events.
12. Clinical assessment of cardiovascular risk incorporates lipid profile, CRP levels, family history, and comorbidities like diabetes and hypertension.
- --
Beyond the Tutorial
Deeper Molecular Pathogenesis
1. LDL oxidation is a key event that makes LDL more atherogenic and chemotactic for macrophages.
2. Scavenger receptors on macrophages mediate the uptake of oxidized LDL, leading to foam cell formation.
3. Matrix metalloproteinases (MMPs) secreted by macrophages degrade collagen in the fibrous cap, contributing to plaque rupture.
Sites of Plaque Predilection
4. Common locations for atherosclerotic plaque formation include:
- Abdominal aorta
- Coronary arteries
- Popliteal arteries
- Internal carotid arteries
- Circle of Willis
Types of Plaques
5. Stable plaques have a thick fibrous cap and cause chronic ischemia through progressive stenosis.
6. Vulnerable (unstable) plaques have a thin fibrous cap, large lipid core, and numerous inflammatory cells, leading to acute thrombosis.
Clinical Presentations
7. Stable angina results from fixed atherosclerotic narrowing.
8. Unstable angina and myocardial infarction result from acute plaque rupture and thrombosis.
9. Transient ischemic attacks (TIAs) or ischemic stroke can occur due to plaque rupture in carotid arteries.
Therapeutic Strategies
10. Anti-inflammatory therapies targeting pathways like IL-1 are under investigation as adjuncts to lipid-lowering treatments in atherosclerosis.
