USMLE/COMLEX 1 - Aortic Aneurysm & Dissection
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Aortic Aneurysm & Dissection, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.

 Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
Below is information not explicitly contained within the tutorial but important for USMLE & COMLEX 1.
- --
VITAL FOR USMLE/COMLEX 1
Aneurysms: Definitions and Types
1. An aneurysm is a dilation involving all three layers of the vessel wall.
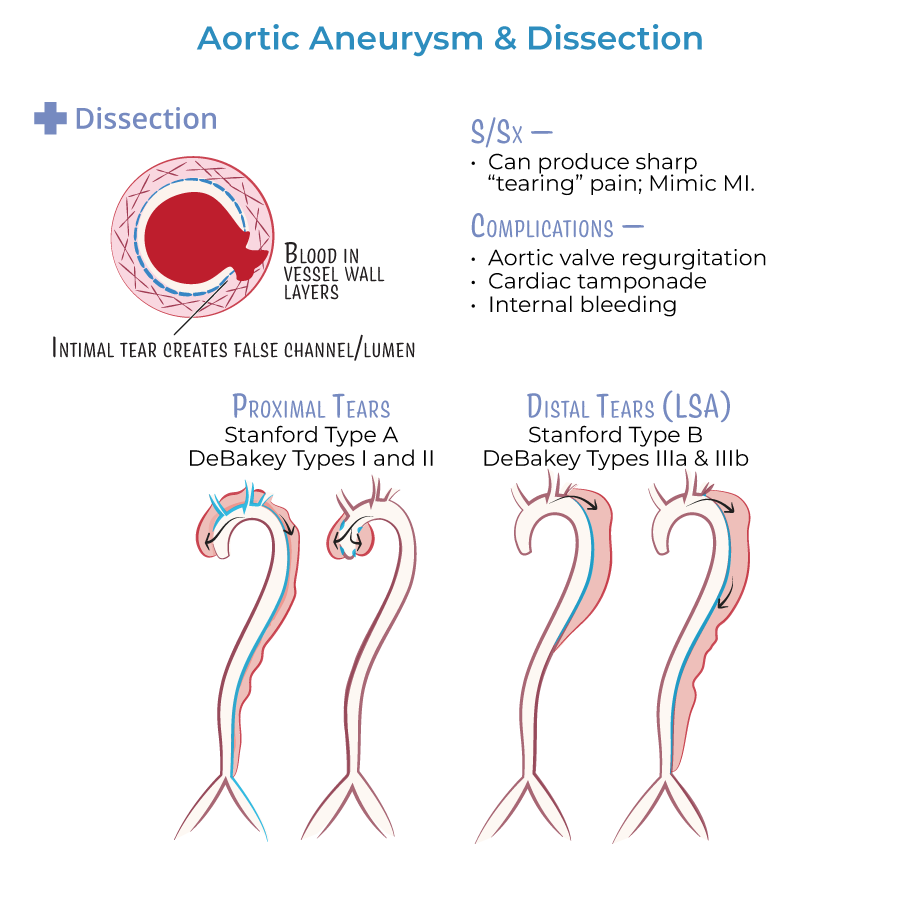
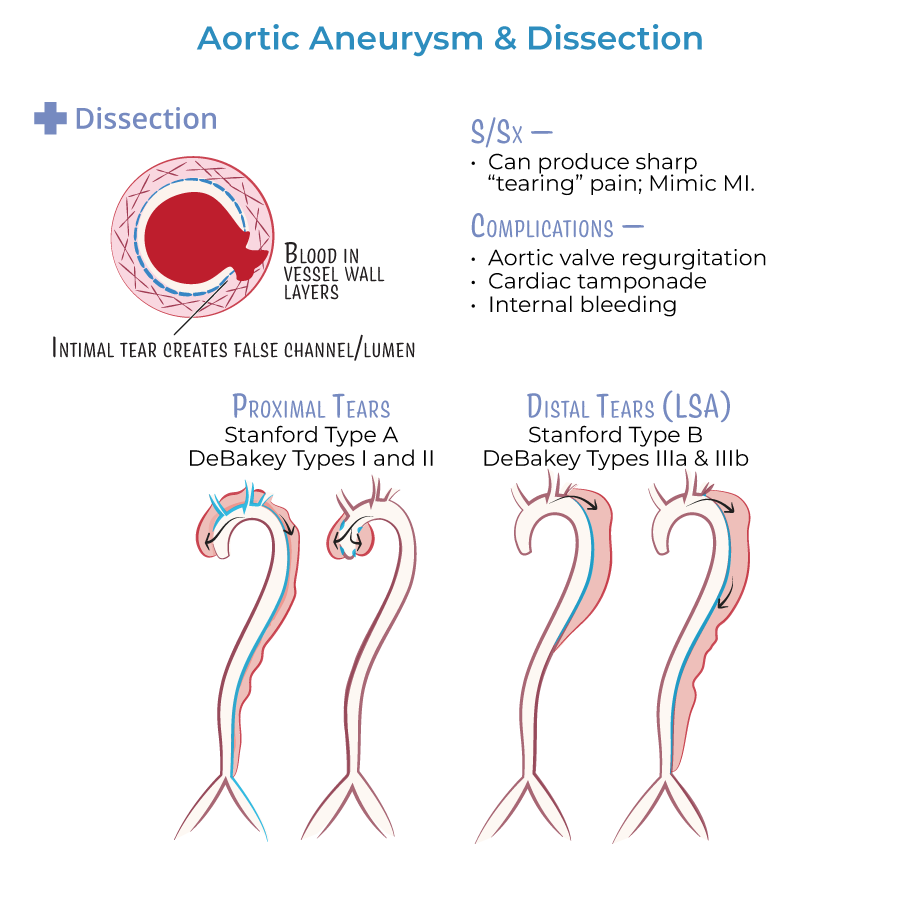
2. A dissection involves blood entering between layers of the vessel wall, creating a false lumen.
3. A pseudoaneurysm (false aneurysm) is not a true aneurysm; it occurs when blood escapes the vessel wall but is contained by surrounding tissue.

Aneurysms by Location
4. Thoracic aortic aneurysms are often due to cystic medial degeneration, commonly associated with Marfan, Loeys-Dietz, and Ehlers-Danlos syndromes.
5. Abdominal aortic aneurysms (AAAs) are associated with atherosclerosis, hypertension, smoking, and male sex over 65 years.
6. AAA is defined as a dilation greater than 3.0 cm; often asymptomatic but may present as a pulsatile abdominal mass.
Aortic Dissection
7. Aortic dissection involves an intimal tear that allows blood to enter between layers, producing sharp, tearing chest pain that may radiate to the back.
8. Stanford Type A dissections involve the ascending aorta; Type B involve the descending aorta.
9. DeBakey Type I involves both ascending and descending; Type II only ascending; Type III only descending.
10. Chest x-ray showing widened mediastinum suggests aortic dissection.
11. Esmolol, a short-acting beta-blocker, is the first-line medical treatment to lower shear stress in dissection.
Complications
12. Dissections can lead to aortic regurgitation, cardiac tamponade, stroke, or rupture.
13. Aneurysms and dissections may both lead to rupture, a life-threatening emergency causing hemorrhage and shock.
- --
HIGH YIELD
Etiology and Pathophysiology
1. Vessel wall weakening results from loss of smooth muscle cells, elastic fibers, and collagen.
2. Contributing factors include hypertension, atherosclerosis, trauma, vasculitis, and infection.
3. Cystic medial degeneration shows abnormal smooth muscle and elastic fibers with ground substance in the media.
4. Mycotic aneurysms result from infections, including bacterial endocarditis or sepsis.
5. Smoking is the most modifiable risk factor for AAA.
6. Women with AAAs tend to present later in life with a worse prognosis.
Morphologic Types of Aneurysms
7. Saccular aneurysms are asymmetrical, sac-like outpouchings.
8. Fusiform aneurysms are symmetrical, spindle-shaped dilations.
9. Pseudoaneurysms may result from trauma or iatrogenic injury and lack all normal vessel layers.
Dissection Classification and Presentation
10. Stanford Type A dissections require emergency surgery due to risk of aortic regurgitation and tamponade.
11. Stanford Type B dissections are managed medically first, unless complications arise.
12. Distinction between Type A and B is essential for treatment decisions.
Clinical Presentation and Diagnosis
13. Classic dissection pain is sudden, severe, tearing and radiates to the interscapular area.
14. BP discrepancy between arms may be present in aortic dissection.
15. Dysphagia, hoarseness, or cough can result from compression by thoracic aneurysms.
Pharmacologic Considerations
16. Negative inotropes, especially beta-blockers, reduce shear stress and should be started before vasodilators.
17. Fluoroquinolones have been associated with increased risk of aneurysm rupture and should be avoided in at-risk patients.
- --
Beyond the Tutorial
Molecular and Genetic Concepts
1. Marfan syndrome involves FBN1 gene mutation affecting fibrillin, leading to medial degeneration.
2. Ehlers-Danlos syndrome (vascular type) involves COL3A1 mutations affecting type III collagen.
3. Loeys-Dietz syndrome involves mutations in TGF-beta signaling pathways and can lead to widespread arterial aneurysms.
Diagnostic Tools
4. CT angiography is the imaging modality of choice for suspected dissection.
5. Transesophageal echocardiography (TEE) is preferred in unstable patients or in the OR.
6. Ultrasound is first-line screening tool for abdominal aortic aneurysm.
Clinical Screening Guidelines
7. One-time screening abdominal ultrasound is recommended for men aged 65 to 75 who have ever smoked.
8. Surgical repair of AAA is recommended when diameter exceeds 5.5 cm, it expands rapidly, or becomes symptomatic.
Emergency Medicine
9. Aortic rupture presents with hypotension, flank or back pain, and a pulsatile mass and requires emergent surgery.
10. In trauma, aortic isthmus is the most common site of traumatic aortic rupture due to deceleration injury.
