USMLE/COMLEX 1 - Adrenal Insufficiency
Start your One-Week Free Trial
Already subscribed? Log in »
USMLE Step 1 & COMLEX-USA Level 1: Adrenal Insufficiency
- --
VITAL FOR USMLE/COMLEX 1
Classification of Adrenal Insufficiency (AI)
1. Primary adrenal insufficiency (PAI), also called Addison's disease, is caused by adrenal gland dysfunction.
2. Central adrenal insufficiency is caused by a deficiency in CRH and/or ACTH.
3. Adrenal insufficiency is associated with high morbidity and mortality, which increase when diagnosis is delayed.
Primary Adrenal Insufficiency (PAI)
1. All adrenal cortex hormones are potentially affected (cortisol, aldosterone, and androgens).
2. Characterized by elevated ACTH production resulting in hyperpigmentation of the skin and mucosa.
3. Patients are hypotensive and hyponatremic, with hyperkalemia and metabolic acidosis.
4. Most common cause in the US: autoimmune diseases with anti-adrenal antibodies.
5. Adrenal crisis: life-threatening condition with shock, fever, dehydration, hypoglycemia, weakness.
Central Adrenal Insufficiency
1. Primarily affects cortisol and androgen secretion (not aldosterone).
2. More common than primary AI.
3. Most commonly caused by long-term exogenous steroid use.
4. No hyperpigmentation (since ACTH is deficient).
5. Less hypovolemia or hypotension (since aldosterone secretion is normal).
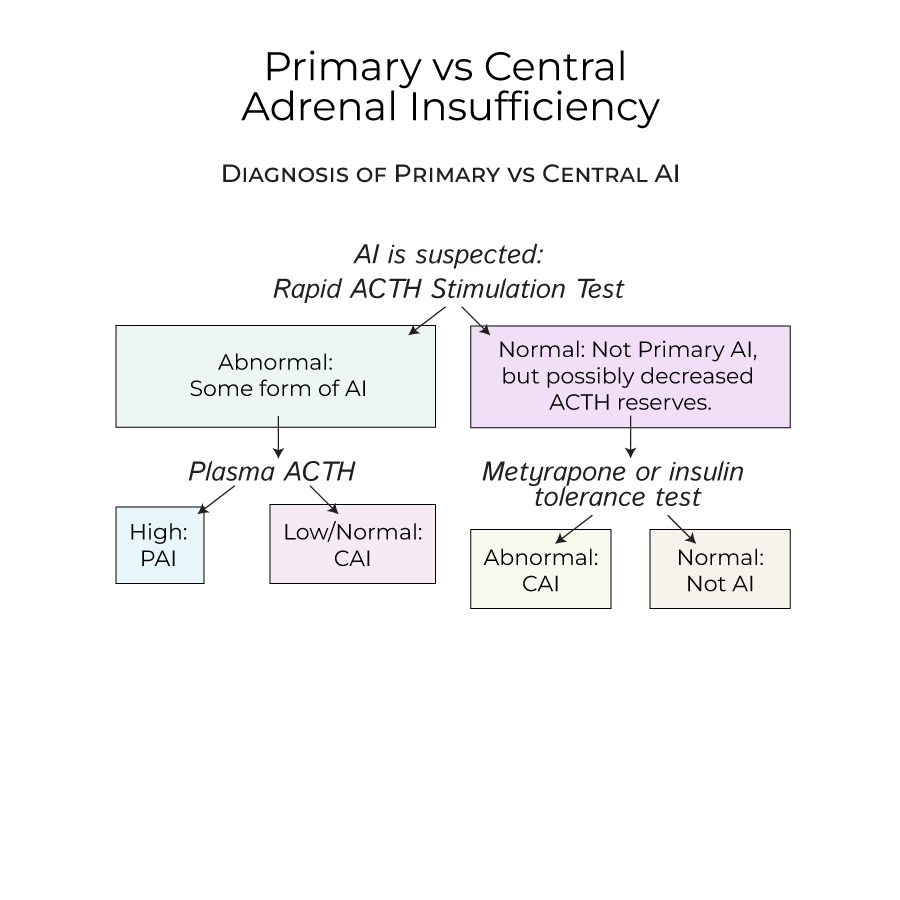
Diagnosis
1. Rapid ACTH stimulation test is key for diagnosis of AI.
2. If abnormal cortisol levels after ACTH stimulation:
- High plasma ACTH indicates Primary AI
- Low/normal plasma ACTH indicates Central AI
- --
HIGH YIELD
Primary Adrenal Insufficiency (PAI)
1. Autoimmune Polyendocrine Syndrome Type 1 (APS-1): onset in childhood, characterized by adrenal insufficiency, hypoparathyroidism, and mucocutaneous candidiasis.
2. Autoimmune Polyendocrine Syndrome Type 2 (APS-2): associated with adrenal insufficiency, Hashimoto's thyroiditis, and Type I diabetes mellitus.
3. Infections are important causes, particularly TB and HIV in endemic countries.
4. John F Kennedy Jr had a famously "bronzed" look due to Addison Disease.
5. Bilateral adrenal hemorrhage: risk factors include anti-coagulation therapy and disorders that increase risk of venous blood clots.
6. Waterhouse-Friderichsen Syndrome: adrenal bleeding caused by septicemia, often with meningococcal or pseudomonas infections.
Central Adrenal Insufficiency
1. Can develop from sudden cessation of steroids or inability of HPA axis to respond to stressors.
2. May be caused by dysfunction in the pituitary or hypothalamus including tumors, infections, and drugs.
3. Immune checkpoint inhibitors, high-dose progestins, and opioids can interrupt ACTH production.
4. Often associated with deficiencies of other pituitary hormones.
5. Symptoms are chronic and nonspecific due to glucocorticoid deficiencies.
Differentiating PAI from CAI
1. No hyperpigmentation in central AI, since ACTH is deficient.
2. Less hypovolemia or hypotension in central AI, since aldosterone secretion is normal.
3. To test for early central AI: metyrapone (prevents cortisol synthesis) or insulin tolerance test.
- --
Beyond the Tutorial
Treatment Approaches
1. Glucocorticoid replacement is essential for all forms of AI.
2. Mineralocorticoid replacement is needed only for primary AI.
3. Must avoid overtreatment with glucocorticoids to prevent Cushing's syndrome.
Prevention and Management of Adrenal Crisis
1. Additional glucocorticoid doses during stressors (surgery, infection, trauma).
2. Patients should carry medical alert cards/jewelry warning of their condition.
3. Immediate treatment for adrenal crisis includes IV fluids, glucose, and hydrocortisone.
Long-term Considerations
1. Regular monitoring of replacement therapy adequacy.
2. Patient education about stress dose adjustments.
3. Screening for associated autoimmune conditions in PAI.
4. Recovery assessment of HPA axis function in iatrogenic central AI.
