USMLE/COMLEX 1 - Abdominal Pain
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for USMLE Step 1 & COMLEX-USA Level 1 from the Abdominal Pain tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR USMLE/COMLEX 1
GI Causes of Abdominal Pain
1. Esophagitis: Inflammation of the esophagus, most often caused by acid reflux, medications, and eosinophilic esophagitis.
2. Gastritis/ulcer disease: Caused by H. pylori infection, drugs, stress, and in the case of gastritis, autoimmune dysfunction.
3. GI strictures and obstruction: Caused by hernias, adhesions, volvulus, tumors, inflammatory narrowing, foreign bodies, and fecal impaction.
4. Diverticulitis: Inflammation (often with bacterial infection) in diverticula, which are pouch-like outcroppings of the intestinal wall.
5. Intestinal ischemia: Result of systemic hypotension, atherosclerosis, blood clots, and constricting fibrosis or strictures.
6. Inflammatory bowel disease: Chronic/remitting autoimmune disorders including Crohn's disease and ulcerative colitis.
7. Functional bowel disorders: Characterized by disordered brain-gut interactions, most commonly Irritable bowel syndrome.
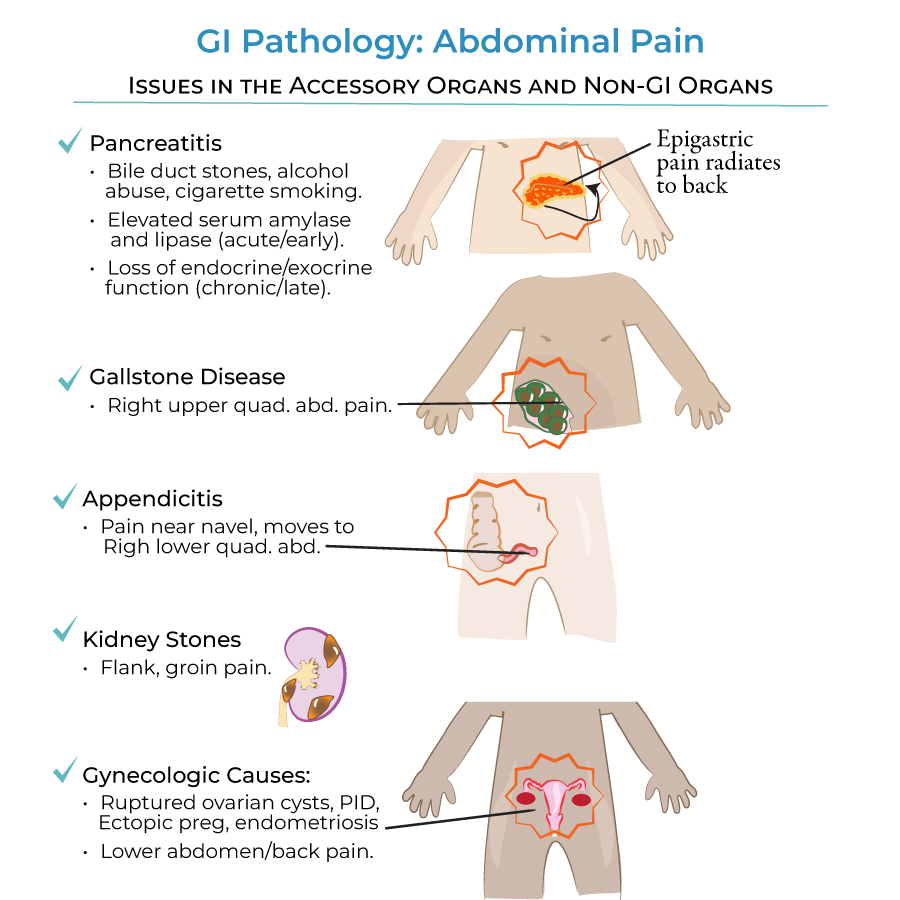
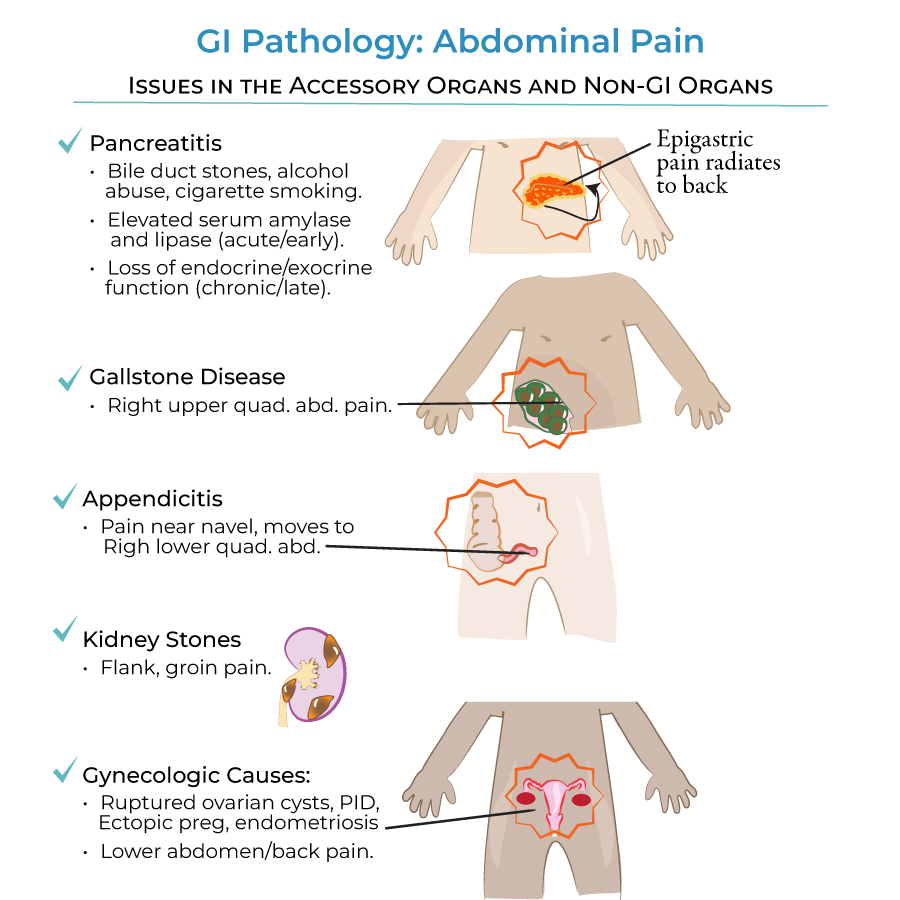
Accessory Organ and Non-GI Causes
1. Pancreatitis: Result of bile duct stones, alcohol abuse, and/or cigarette smoking.
2. Gallstone disease: Causes pain in the right upper abdominal quadrant.
3. Appendicitis: Often presents with pain in the peri-navel area that later moves to the right lower abdominal quadrant.
4. Kidney stones: Cause "flank" pain that can travel to the groin area.
5. Gynecological causes: Include ruptured ovarian cysts, pelvic inflammatory disease, ectopic pregnancy, and endometriosis.
- --
HIGH YIELD
GI Causes of Abdominal Pain
1. Esophagitis: Treatments include proton pump inhibitors to reduce acid production by the stomach.
2. Gastritis and stomach ulcers: Inflammation can travel up and down the esophagus to and from the stomach. Treatments include proton pump inhibitors, antacids, H2 blockers, and prostaglandins.
3. Intestinal ischemia: More common in the intestines than in the stomach or esophagus. Treatment includes surgery and/or medications to restore blood flow.
4. Inflammatory bowel disease: Patients often experience diarrhea in addition to abdominal cramping. In ulcerative colitis, the diarrhea is frequently bloody. Treatments include anti-inflammatories and immune suppressors.
5. Functional bowel disorders: Etiologies are uncertain, but are thought to include infection and/or psychosocial causes.
Accessory Organ and Non-GI Causes
1. Pancreatitis: Early/acute pancreatitis is characterized by elevated serum amylase and lipase levels. Late/chronic pancreatitis can result in loss of endocrine and exocrine functions. Causes epigastric pain that radiates towards the back.
2. Gallstone disease: Pain occurs because gallstones get stuck in the biliary system, which is towards the right side of the abdomen.
3. Appendicitis: Characteristic pain migration from peri-navel to right lower quadrant is a key diagnostic feature.
4. Gynecological causes: Essentially, anything that causes inflammation and swelling of the uterus or ovaries can cause lower abdominal and back pain.
- --
Beyond the Tutorial
Diagnostic Approaches
1. Abdominal quadrant assessment: Understanding the relationship between pain location and likely underlying pathology.
2. Laboratory markers: Specific tests for different conditions (e.g., amylase/lipase for pancreatitis, WBC count for appendicitis).
3. Imaging modalities: When to use ultrasound vs. CT vs. MRI for different abdominal conditions.
4. Acute vs. chronic presentation: Differentiating features based on time course.
Clinical Pearls
1. Referred pain patterns: How visceral structures typically refer pain to specific locations.
2. Red flag symptoms: Features that suggest serious underlying pathology requiring urgent intervention.
3. Age-related considerations: Frequency of different causes across lifespan.
4. Medical vs. surgical management: Decision-making framework for intervention.
5. Complications to watch for: Progression of untreated conditions and potential systemic effects.
