
Start your One-Week Free Trial
Already subscribed? Log in »
Menstrual Cycle (Ovarian and Uterine Cycles)
Overview
HPO axis
 Estrogen and progesterone exert negative feedback effects at the anterior pituitary and hypothalamus during most of the menstrual cycle; the inhibins, another set of gonadal hormones, also inhibit gonadotropin secretion.
However, as the dominant follicle secretes increasing quantities of estrogen, a threshold is surpassed and estrogen’s inhibitory effect “switches” to a positive feedback loop, leading to a “surge” in gonadotropin release – as we’ll see, this triggers ovulation.
Notice that our diagram implies that the gonadotrophs and ovarian hormones are released at the same time in response to the same triggers – it’s a little more complicated than that, so we need to create a diagram that shows how events unfold throughout the cycle.
Estrogen and progesterone exert negative feedback effects at the anterior pituitary and hypothalamus during most of the menstrual cycle; the inhibins, another set of gonadal hormones, also inhibit gonadotropin secretion.
However, as the dominant follicle secretes increasing quantities of estrogen, a threshold is surpassed and estrogen’s inhibitory effect “switches” to a positive feedback loop, leading to a “surge” in gonadotropin release – as we’ll see, this triggers ovulation.
Notice that our diagram implies that the gonadotrophs and ovarian hormones are released at the same time in response to the same triggers – it’s a little more complicated than that, so we need to create a diagram that shows how events unfold throughout the cycle.
Menstrual Cycle
Two ovarian phases: follicular and luteal.
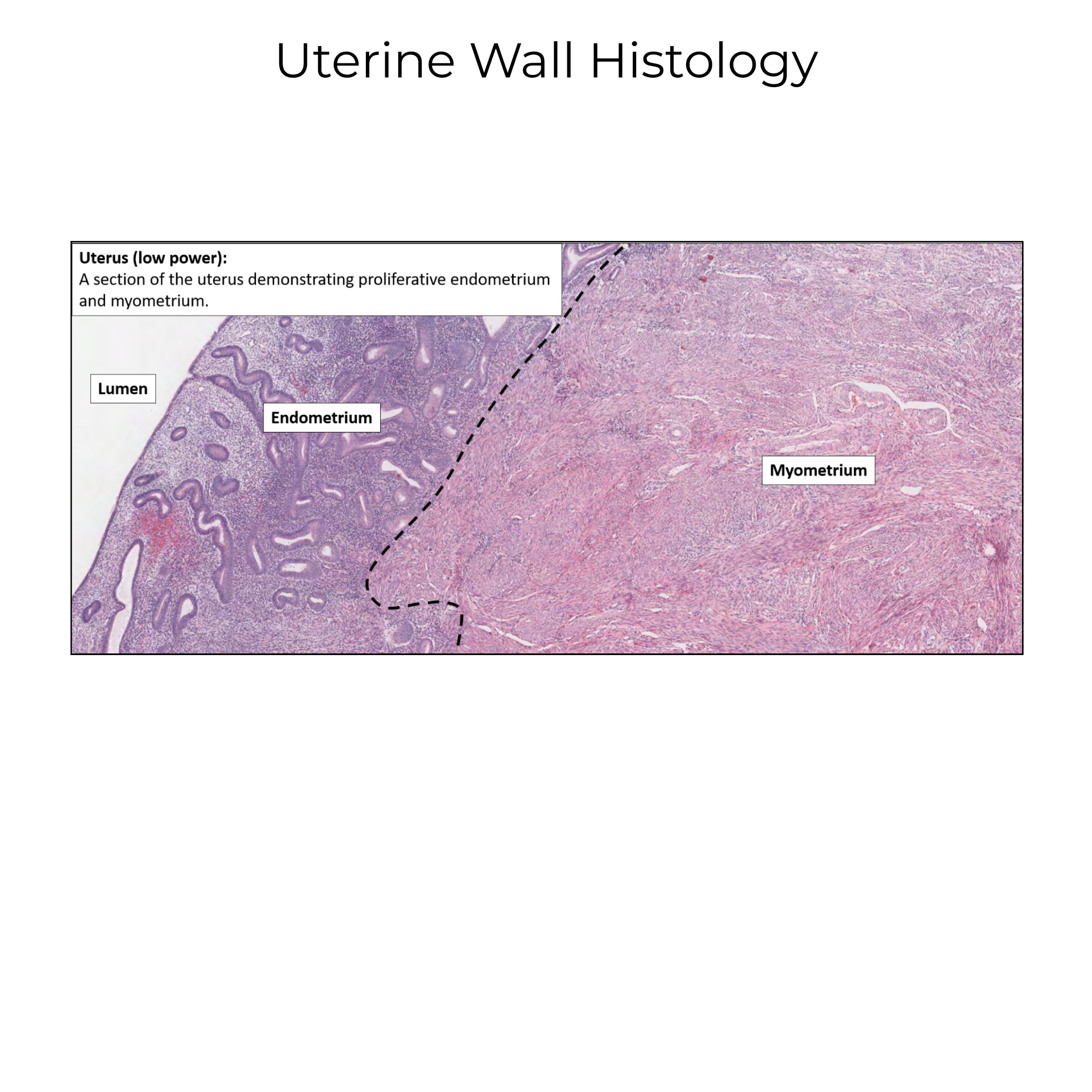
Three stages of endometrial changes:
Menses, when the outermost layer is shed.
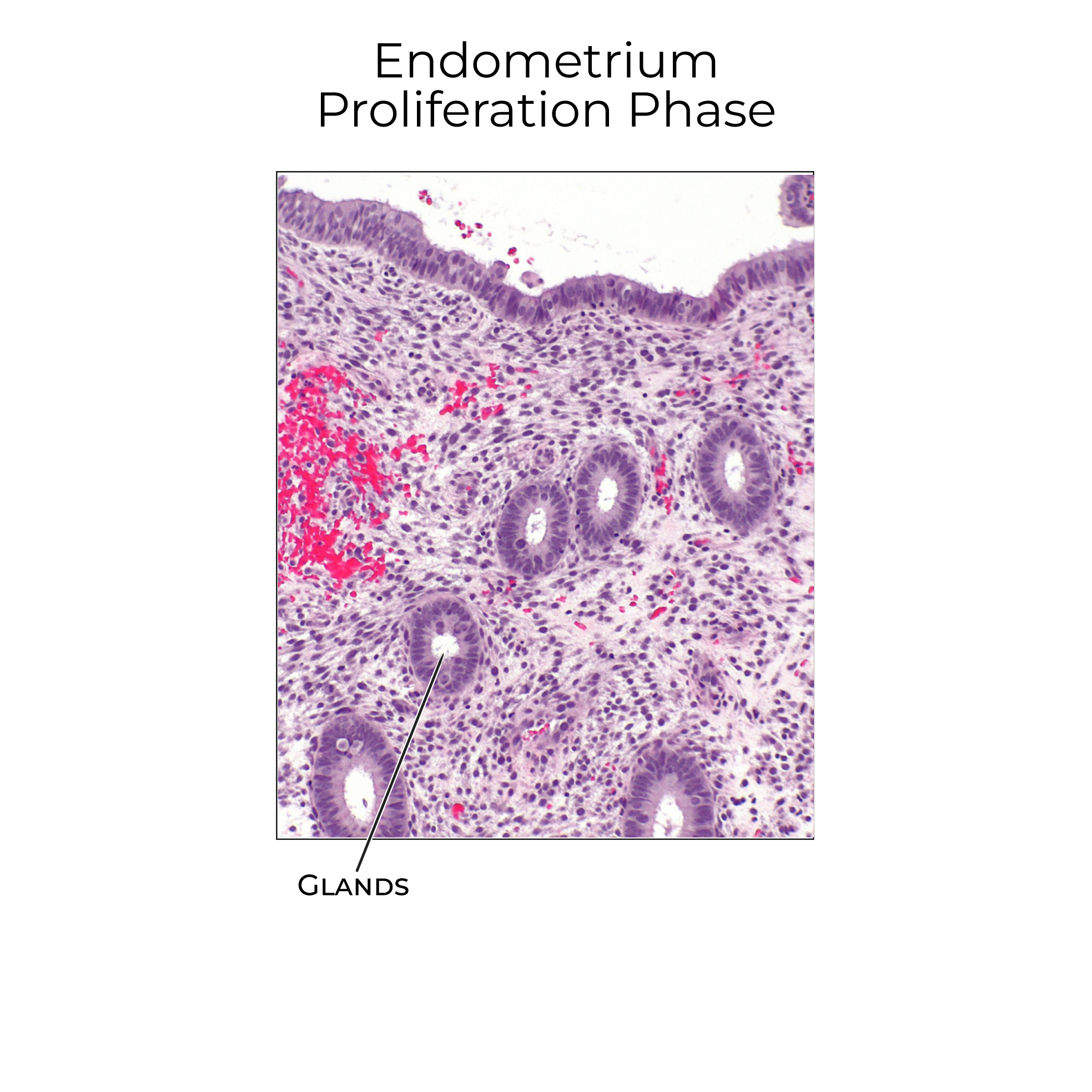
Proliferation, when the endometrium begins the process of renewal.
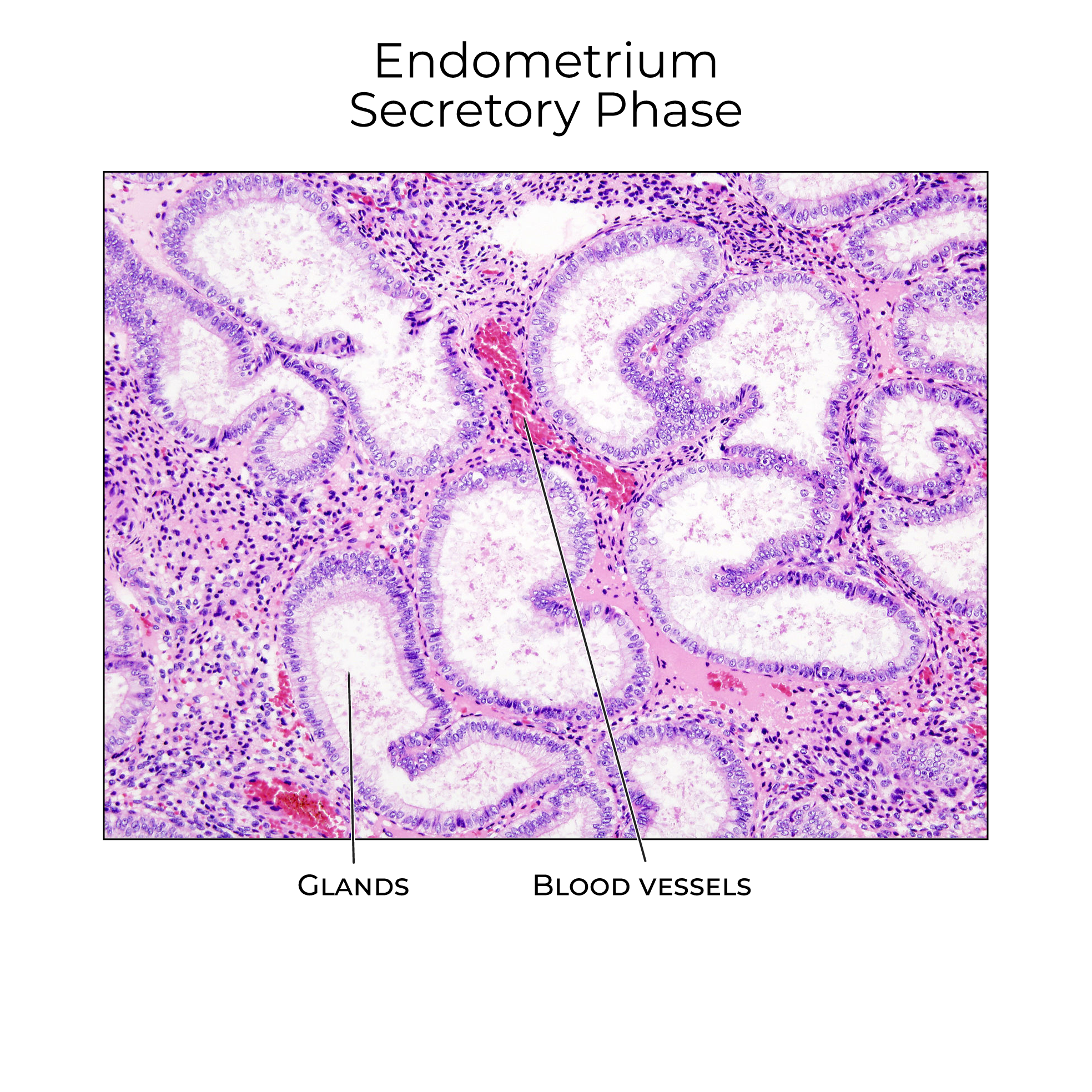
And, secretory, when the endometrium becomes rich in glandular tissue and reaches maximal thickness.
Follicular Phase
Start in the follicular phase of the ovarian cycle and show that:
The endometrial layer is shed during menses; it will be expelled along with the oocyte in the menstrual blood.
Also during the follicular phase, FSH and LH levels slowly rise, which promotes the growth of the ovarian follicles; as a result of follicular growth and the selection of a dominant follicle, estrogen levels increase.
In response to rising estrogen levels, the endometrium enters the proliferative stage and tissue regeneration begins.
As the dominant follicle enlarges, its estrogen secretion surpasses threshold and stimulates the anterior pituitary to produce the LH surge. This is the positive feedback loop we drew in our previous diagram.
The LH surge triggers ovulation – the release of the oocyte from the dominant follicle; ovulation marks the shift from the follicular phase to the luteal phase (ovulation is not a phase, per se, but an event).
Luteal Phase
The oocyte travels through the uterine tubes to the uterus. If fertilization occurs, it typically happens within the uterine tube.
Now, show that LH, FSH, and estrogen levels decline after ovulation due to the rupture of the dominant follicle.
The remnants of the dominant follicle differentiate to become a new endocrine structure: the corpus luteum, which produces progesterone.
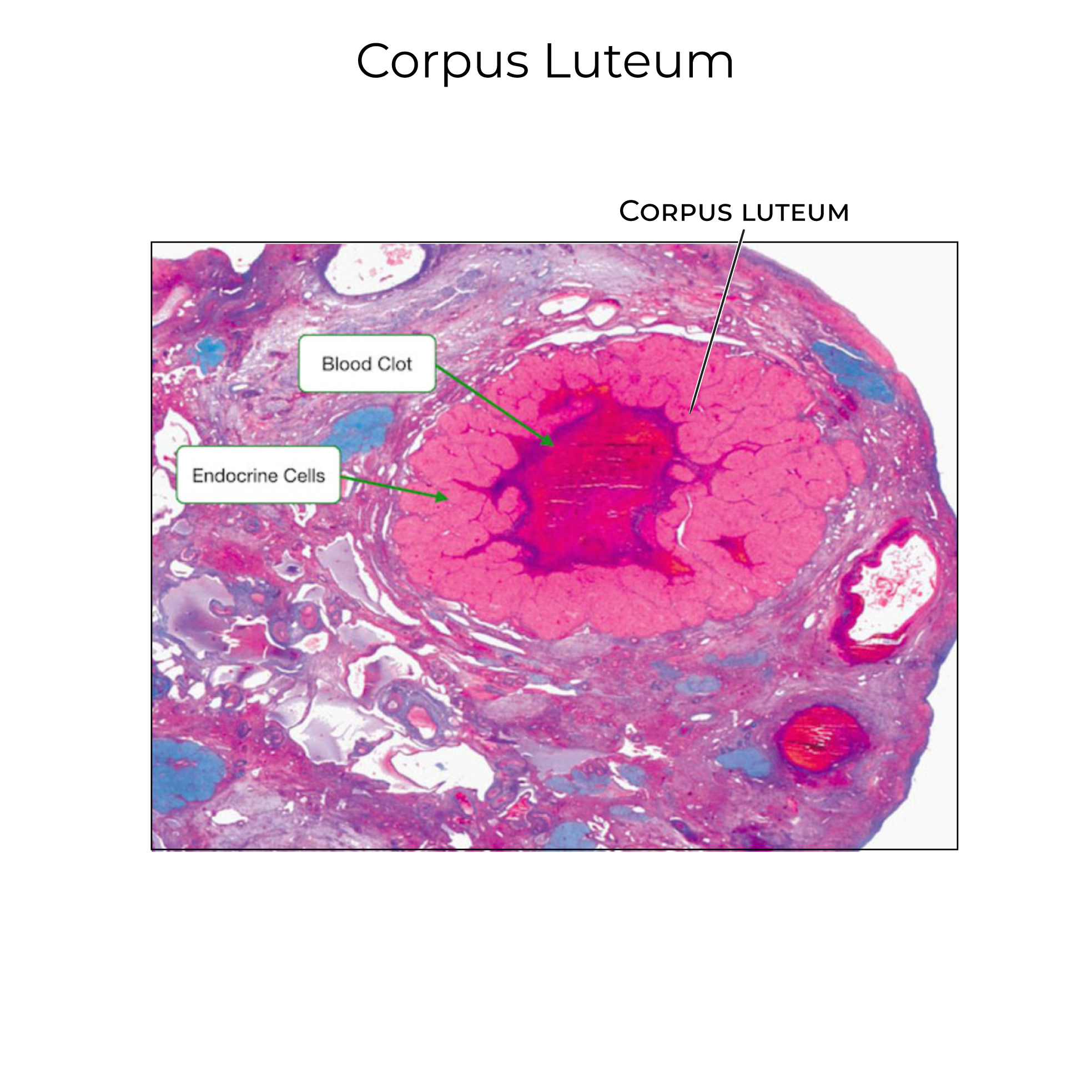 Rising progesterone levels induces the endometrial shift to the secretory stage; notice the increased glandular tissue in our diagram, and that the network of spiral arteries expands to meet the demands of the growing tissue.
In most cases, fertilization does not occur, and the corpus luteum differentiates again to become the corpus albicans, and progesterone secretion decreases. Ultimately, reduced progesterone levels allow endometrial shedding to begin again and menses occurs – thus beginning a new menstrual cycle.
If fertilization had occurred, the corpus luteum would have persisted and continued to secrete progesterone, thus maintaining the endometrial environment required for implantation.
Rising progesterone levels induces the endometrial shift to the secretory stage; notice the increased glandular tissue in our diagram, and that the network of spiral arteries expands to meet the demands of the growing tissue.
In most cases, fertilization does not occur, and the corpus luteum differentiates again to become the corpus albicans, and progesterone secretion decreases. Ultimately, reduced progesterone levels allow endometrial shedding to begin again and menses occurs – thus beginning a new menstrual cycle.
If fertilization had occurred, the corpus luteum would have persisted and continued to secrete progesterone, thus maintaining the endometrial environment required for implantation.
Timing and Duration
Menstrual Cycle Length
Most menstrual cycles last 23-35 days, with an average cycle length of 28 or 29 days, depending on the study. Be aware that any given individual will also experience cycles of different lengths. For more on cycle length variability, see our notes.
The mean duration of menses, that is, days of menstrual bleeding, is about 4 days, with an average of 30 mL of blood lost. Menstrual fluid isn’t just blood though, it also contains cervical mucus, vaginal secretions, and endometrial tissue.
Anovulation
Up to 12% of cycles in healthy, normally cycling individuals are anovulatory, meaning that an egg is not released from the ovary.
Anovulation rates are higher in the years following menarche (onset of first menses) and during perimenopause (the time leading up to menopause). Stress and other factors can also lead to anovulation, which reflects the body’s ability to shift energetic priorities in response to environmental changes.
See ovulatory disorders
The Fertile Window
The fertile window is the approximately 6-day window when intercourse can lead to pregnancy; indicate that it includes the 5 days preceding ovulation and the day of ovulation. This window is set by the lifespan of sperm cells.
Sexual intercourse in the days preceding and following the fertile window is unlikely to result in pregnancy. However, variation in the timing of ovulation makes it nearly impossible to predict the fertile window. This is why calendar-based birth control methods, which assume to know the date of ovulation, are unreliable.
Embryo Viability
On a related note, 30-50% of fertilized eggs do not implant, and more than 20% of implanted embryos are expelled during menses without the menstruating person’s awareness. These spontaneous abortions, or miscarriages, are most often due to genetic abnormalities that are incompatible with life.
Review fertilization & implantation

