Chlamydia, Gonorrhea, Syphilis for ABIM
Chlamydia, Gonorrhea, Syphilis for the American Board of Internal Medicine Exam
Chlamydia
- Etiology:
- Caused by Chlamydia trachomatis, an obligate intracellular bacterium with serotypes D–K responsible for urogenital infections.
- Epidemiology:
- Most common bacterial sexually transmitted infection (STI) in the U.S. with highest rates among young adults (ages 15–24).
- Clinical Manifestations:
- Men: Often asymptomatic but may present with urethritis, dysuria, and mucoid or clear urethral discharge.
- Women: Frequently asymptomatic; symptomatic infections include cervicitis (mucopurulent discharge, friable cervix), urethritis, pelvic inflammatory disease (PID), which may lead to chronic pelvic pain and infertility.
- Complications: Epididymitis in men, PID in women, and risk of ectopic pregnancy and infertility if untreated.
- Diagnosis:
- Nucleic Acid Amplification Test (NAAT): Gold standard for diagnosing C. trachomatis, can be performed on urine or swab specimens from genital sites.
- Treatment:
- First-line: Doxycycline 100 mg PO twice daily for 7 days or azithromycin 1 g PO single dose.
- Alternative: For pregnancy, azithromycin is preferred due to doxycycline contraindication.
- Partner Notification and Treatment: Essential to prevent reinfection; partners should be evaluated and treated.
Gonorrhea
- Etiology:
- Caused by Neisseria gonorrhoeae, a gram-negative diplococcus.
- Epidemiology:
- High prevalence in individuals aged 15–24; co-infection with chlamydia is common.
- Clinical Manifestations:
- Men: Urethritis with purulent discharge, dysuria; can lead to epididymitis if untreated.
- Women: Asymptomatic in up to 50%; when symptomatic, cervicitis (purulent discharge), PID, and urethritis are common.
- Extragenital Manifestations: Pharyngeal and rectal infections from oral and anal sex; ocular infections from direct inoculation.
- Disseminated Gonococcal Infection (DGI): Bacteremia leading to dermatitis-arthritis syndrome, tenosynovitis, and septic arthritis.
- Diagnosis:
- NAAT: Preferred for detecting N. gonorrhoeae from urine or swabs of urogenital and extragenital sites.
- Gram Stain: Useful in symptomatic men, showing gram-negative intracellular diplococci.
- Treatment:
- First-line: Ceftriaxone 500 mg IM single dose; if co-infected with chlamydia, add doxycycline 100 mg PO twice daily for 7 days.
- Alternative: For severe beta-lactam allergy, gentamicin plus azithromycin, though resistance concerns exist.
- Partner Treatment: Partners should be notified and treated to prevent reinfection.
Syphilis
- Etiology:
- Caused by Treponema pallidum, a spirochete bacterium.
- Epidemiology:
- Rising incidence in the U.S., particularly among men who have sex with men (MSM) and individuals co-infected with HIV.
- Stages and Clinical Manifestations:
- Primary Syphilis:
- Occurs ~3 weeks post-infection with a painless chancre at the site of inoculation (often genital but may be extragenital).
- Chancre heals spontaneously within 3–6 weeks without treatment.
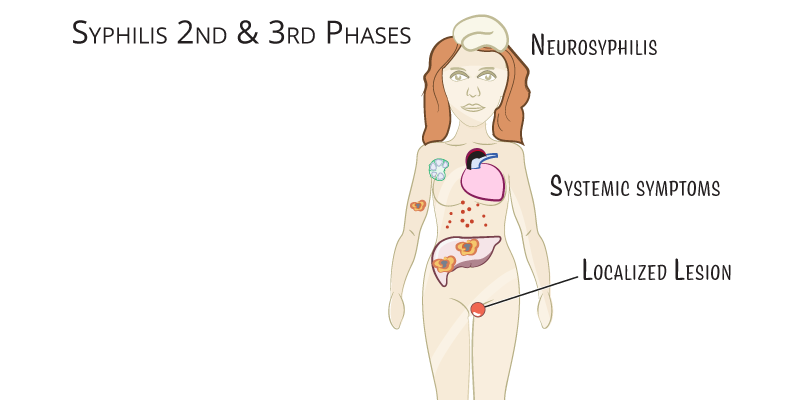
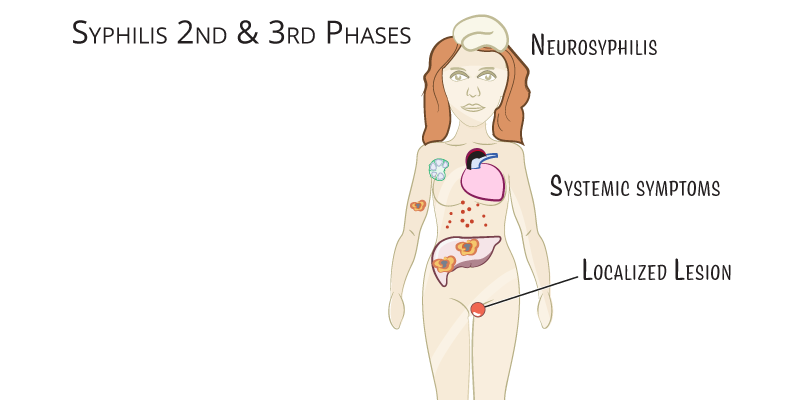
- Secondary Syphilis:
- Occurs weeks to months after initial infection, presenting with systemic symptoms: maculopapular rash (involving palms and soles), condylomata lata (moist papules in anogenital area), lymphadenopathy, and mucosal lesions.
- These symptoms also resolve without treatment.
- Latent Syphilis:
- Defined as asymptomatic infection following secondary syphilis.
- Early Latent: Infection within the last year; Late Latent: Infection of more than one year.
- Tertiary Syphilis:
- May develop years after untreated infection, with severe complications including gummatous lesions, cardiovascular involvement (aortitis), and neurosyphilis (Tabes dorsalis, general paresis).
- Diagnosis:
- Nontreponemal Tests (Screening): Rapid plasma reagin (RPR) or venereal disease research laboratory (VDRL) test; used for screening and to monitor treatment response.
- Treponemal Tests (Confirmatory): Fluorescent treponemal antibody absorption (FTA-ABS) or T. pallidum particle agglutination (TPPA); remain positive for life, confirming infection history.
- Treatment:
- Primary, Secondary, and Early Latent Syphilis: Benzathine penicillin G 2.4 million units IM single dose.
- Late Latent and Tertiary Syphilis (without neurosyphilis): Benzathine penicillin G 2.4 million units IM weekly for 3 weeks.
- Neurosyphilis: Aqueous crystalline penicillin G 18–24 million units per day IV for 10–14 days.
- Alternative Therapy for Penicillin Allergy: Doxycycline or tetracycline for primary and secondary stages; desensitization recommended for neurosyphilis.
- Follow-Up:
- Serial RPR or VDRL titers at 6 and 12 months to ensure treatment efficacy.
- Partner testing and treatment are critical to control transmission.
Key Points
- Chlamydia:
- Caused by Chlamydia trachomatis and is often asymptomatic, especially in women.
- Can lead to PID, ectopic pregnancy, and infertility in untreated women.
- Diagnosed by NAAT; treated with doxycycline or azithromycin.
- Partner treatment is essential to prevent reinfection.
- Gonorrhea:
- Caused by Neisseria gonorrhoeae, often co-infecting with chlamydia.
- Men typically present with urethritis, while women are often asymptomatic.
- NAAT is the preferred diagnostic method; treated with ceftriaxone plus doxycycline if chlamydia is present.
- Important to treat partners to prevent reinfection.
- Syphilis:
- Caused by Treponema pallidum, presenting in distinct stages: primary (chancre), secondary (rash, systemic symptoms), latent (asymptomatic), and tertiary (cardiovascular and neurosyphilis).
- Diagnosed by nontreponemal and confirmatory treponemal tests.
- Treated with penicillin, with the duration depending on stage; follow-up serology and partner treatment are essential to prevent spread.
