Interstitial Lung Diseases for PA
Start your One-Week Free Trial
Already subscribed? Log in »
Interstitial Lung Diseases for the Physician Assistant Licensing Exam
Pathophysiology
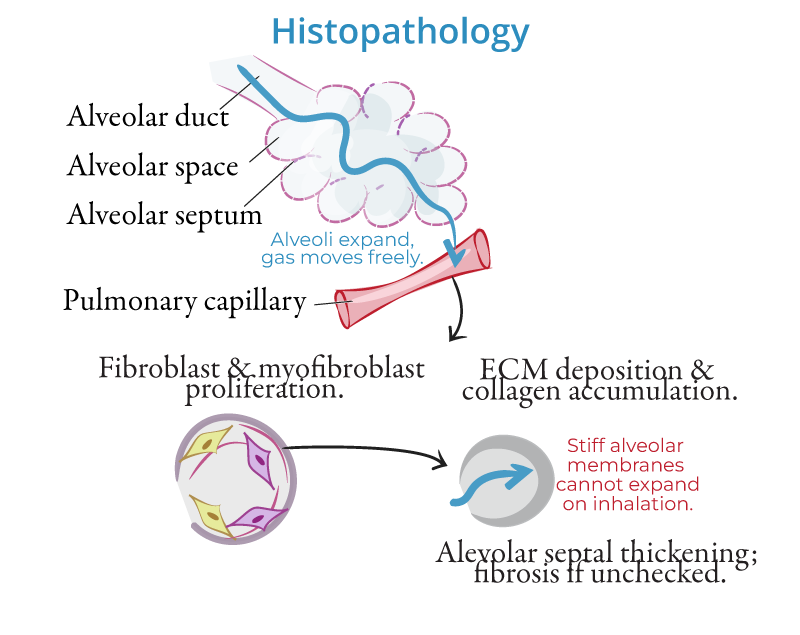
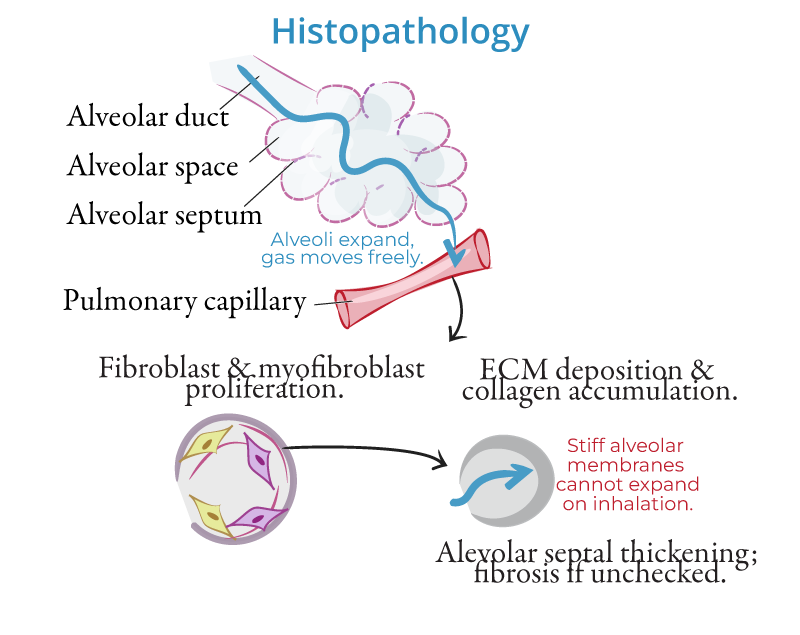
- Chronic Inflammation and Fibrosis:
- Interstitial lung diseases (ILDs) are characterized by chronic inflammation and fibrosis of the lung interstitium, leading to scarring, thickened alveolar walls, and impaired gas exchange.
- Fibrotic Process:
- Fibroblasts deposit excess collagen in response to injury, resulting in lung stiffness and reduced compliance, which limits lung expansion and contributes to respiratory impairment.
Etiologies
- Idiopathic Pulmonary Fibrosis (IPF):
- A common and progressive form of ILD with no known cause. IPF is marked by relentless fibrosis and a poor prognosis, characterized histologically by usual interstitial pneumonia (UIP).
- Pneumoconioses:
- ILDs caused by inhalation of inorganic dusts:
- Asbestosis: From asbestos exposure, often in construction workers.
- Silicosis: From inhalation of silica dust, common in miners.
- Coal Workers' Pneumoconiosis: Known as "black lung" disease.
- Hypersensitivity Pneumonitis (HP):
- An immune response to inhaled organic antigens (e.g., bird feathers, mold), causing granulomatous inflammation and fibrosis with chronic exposure.
- Sarcoidosis:
- A systemic granulomatous disorder often affecting the lungs, characterized by noncaseating granulomas and potential fibrosis in chronic cases.
Clinical Features
- Dyspnea:
- Gradual onset of breathlessness, worsening with exertion.
- Dry Cough:
- Persistent, nonproductive cough commonly associated with ILDs.
- Crackles:
- Fine, velcro-like inspiratory crackles heard on lung auscultation, especially at the bases.
Diagnosis
- High-Resolution CT (HRCT):
- The gold standard for diagnosing ILD. It shows honeycombing (indicative of fibrosis) and ground-glass opacities (inflammation).
- Pulmonary Function Tests (PFTs):
- Reveal a restrictive pattern with reduced total lung capacity (TLC) and forced vital capacity (FVC).
Management
- Antifibrotic Agents:
- Pirfenidone and nintedanib slow progression of idiopathic pulmonary fibrosis (IPF).
- Corticosteroids:
- Used in inflammatory ILDs such as sarcoidosis or hypersensitivity pneumonitis.
- Oxygen Therapy and Pulmonary Rehabilitation:
- Improve quality of life in advanced disease.
Key Points
- ILDs are a group of disorders involving chronic inflammation and fibrosis of the lung interstitium, leading to restrictive lung disease and impaired gas exchange.
- Common causes include idiopathic pulmonary fibrosis (IPF), pneumoconioses, hypersensitivity pneumonitis, and sarcoidosis.
- Diagnosis is based on high-resolution CT (HRCT) and pulmonary function tests showing a restrictive pattern.
- Management includes antifibrotic agents, corticosteroids, oxygen therapy, and pulmonary rehabilitation to slow disease progression and improve quality of life.
