PANCE Aortic Aneurysm & Dissection
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Aortic Aneurysm & Dissection, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.

- --
VITAL FOR PANCE
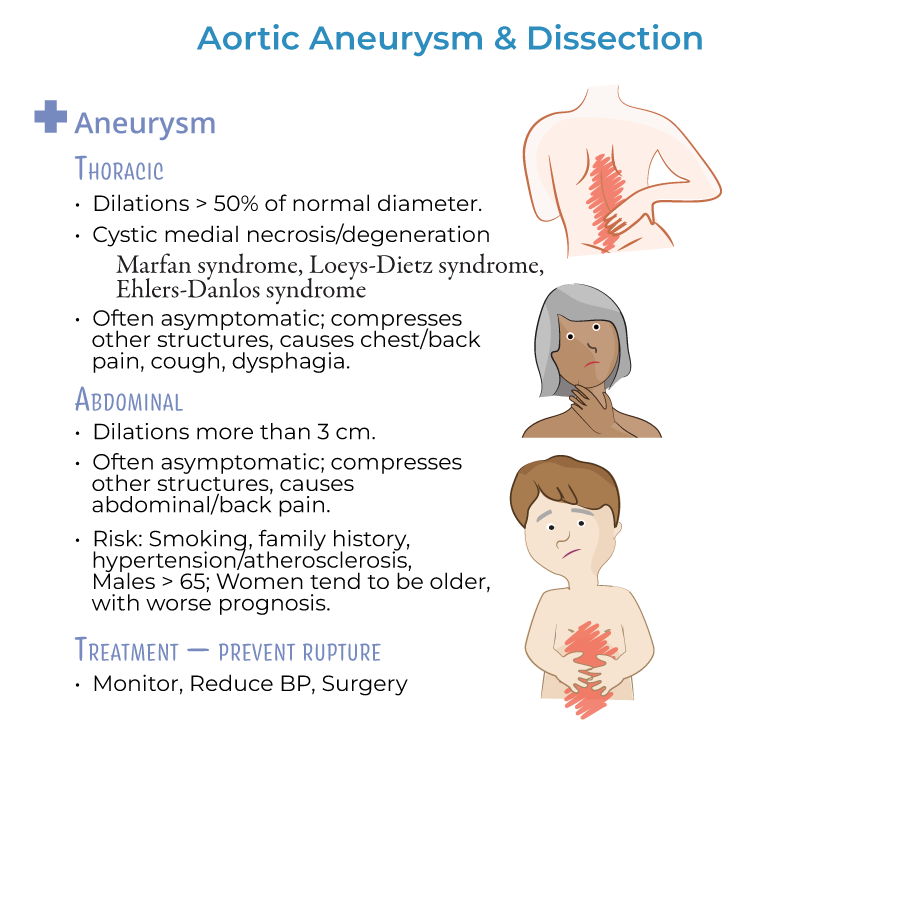
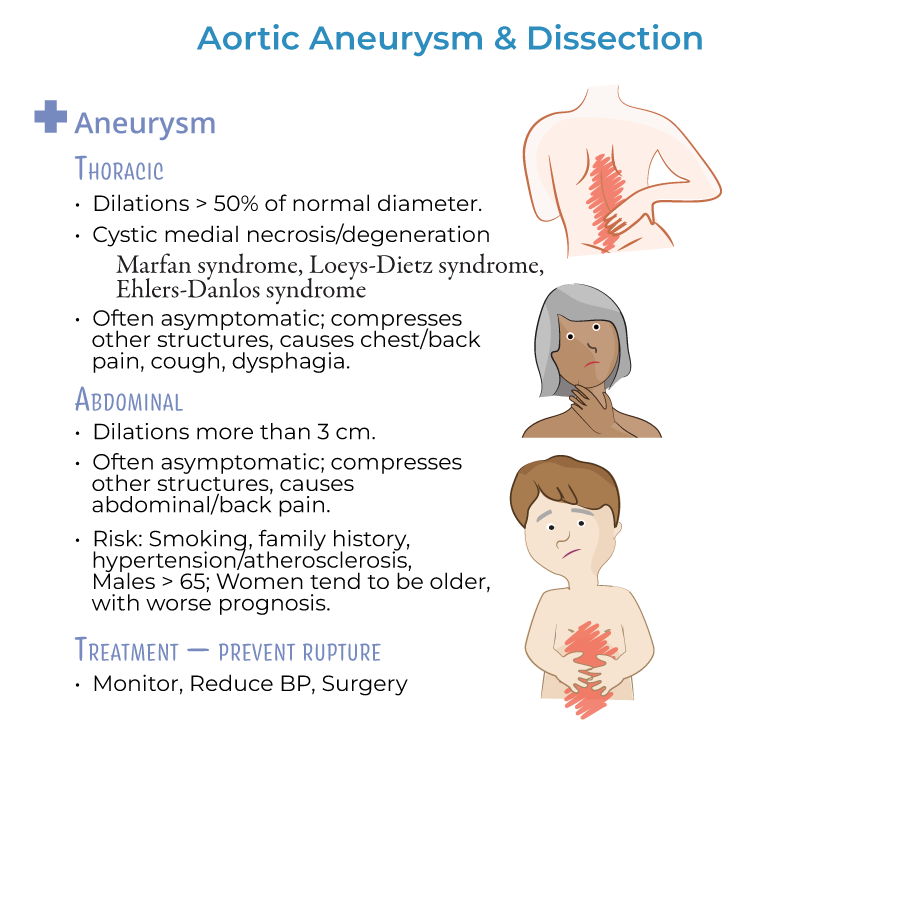
Aortic Aneurysm
1. Abdominal Aortic Aneurysm (AAA) typically affects men over 65 years with smoking history, hypertension, and atherosclerosis.
2. One-time abdominal ultrasound screening is recommended for males aged 65–75 who have ever smoked.
3. AAA is defined as a dilation greater than 3.0 cm; surgical repair is indicated if ≥5.5 cm or rapidly enlarging.
4. Symptomatic AAAs (pain, pulsatile mass, hypotension) require emergency surgical repair.
5. Asymptomatic small AAAs are managed with periodic ultrasound surveillance.

Thoracic Aortic Aneurysm
6. Thoracic aortic aneurysms are associated with genetic connective tissue disorders like Marfan syndrome and Ehlers-Danlos.
7. Indications for surgery include size ≥5.5 cm or if symptomatic.
8. Diagnosis is confirmed with CT angiography.
Aortic Dissection
9. Stanford Type A dissections (ascending aorta) require emergency surgical repair.
10. Stanford Type B dissections (descending aorta) are typically managed medically first unless complications arise.
11. Clinical presentation includes sudden onset tearing chest or back pain, often with pulse deficits or BP differences between limbs.
12. Initial management is IV beta-blocker (e.g., esmolol) to lower heart rate and blood pressure.
13. Chest x-ray may show widened mediastinum; CT angiography is the gold standard for stable patients.
- --
HIGH YIELD
Risk Factors
1. Hypertension is the number one risk factor for aortic dissection.
2. Smoking is the major modifiable risk factor for AAA.
3. Genetic conditions like Marfan syndrome predispose to thoracic aneurysm and dissection.
Clinical Presentation
4. Aortic rupture presents with hypotension, back or flank pain, and shock.
5. Hoarseness, dysphagia, and cough can occur due to compression by thoracic aneurysms.
6. New diastolic murmur may suggest aortic regurgitation due to dissection.
7. Pain from dissection may migrate as the dissection propagates.
Diagnostics
8. In stable patients, perform CT angiography for suspected dissection.
9. In unstable patients or those with renal failure, use transesophageal echocardiography (TEE).
Management Principles
10. For aortic dissection, lower heart rate to 60 bpm and systolic blood pressure to 100-120 mmHg.
11. Use nitroprusside only after beta-blockade if BP remains high.
12. Avoid vasodilators alone without prior beta-blockade due to risk of reflex tachycardia worsening dissection.
Pharmacologic Considerations
13. Avoid fluoroquinolones in patients with known aneurysms due to rupture risk.
14. Long-term management after dissection repair includes strict blood pressure control and lifelong imaging surveillance.
- --
Beyond the Tutorial
Pathophysiology and Genetics
1. Cystic medial degeneration underlies many thoracic aneurysms and dissections.
2. Fibrillin-1 mutation (FBN1) in Marfan syndrome leads to defective connective tissue.
Surveillance and Follow-up
3. After AAA repair, patients need routine imaging surveillance with CT or ultrasound.
4. Smoking cessation is critical to slow progression of small aneurysms.
Special Clinical Cases
5. In trauma (e.g., motor vehicle accident), aortic isthmus rupture is the most common site of injury.
6. Monitor for cardiac tamponade in patients with ascending aortic dissection affecting the pericardium.
7. Recognize stroke-like symptoms as possible manifestations of proximal dissection involving carotid arteries.
Emergency Room and Acute Care
8. Initiate immediate cardiothoracic surgery consultation in cases of Stanford Type A dissection.
9. Know that Stanford Type B dissection with malperfusion, expansion, or rupture also requires surgical repair despite initially being treated medically.
10. AAA rupture carries extremely high mortality without emergent operative intervention.
