PANCE - Thyroid Gland Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Thyroid Gland Pathophysiology tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for PANCE & PANRE.
Below is information not explicitly contained within the tutorial but important for PANCE & PANRE.
- --
VITAL FOR PANCE
Thyroid Pathophysiology Fundamentals
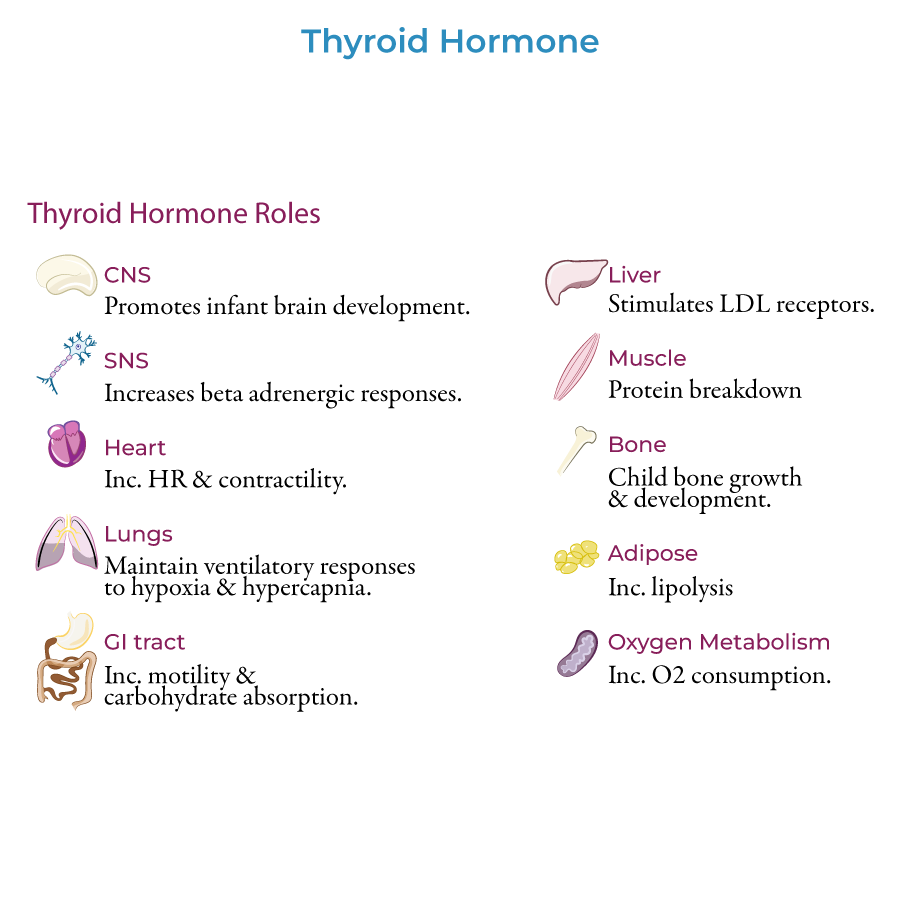
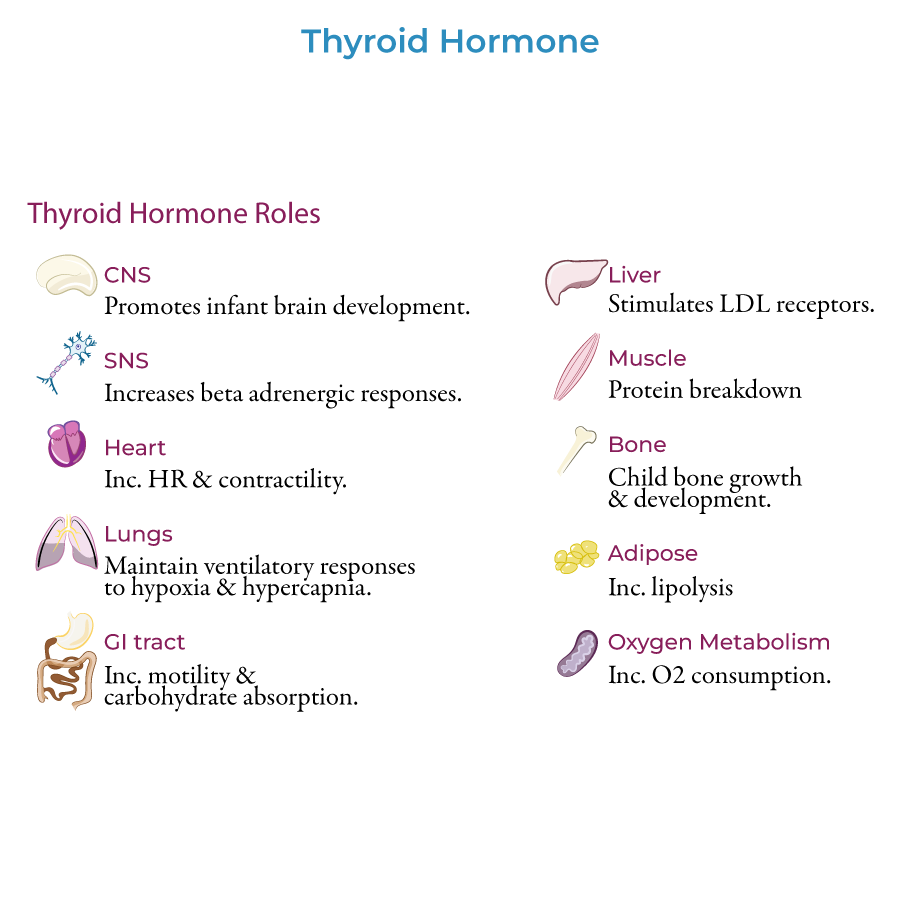
1. Essential Functions: Thyroid hormones T3 and T4 are responsible for: CNS development in infants, Bone growth and maturation in children, Proper functioning in multiple organ systems in adults.
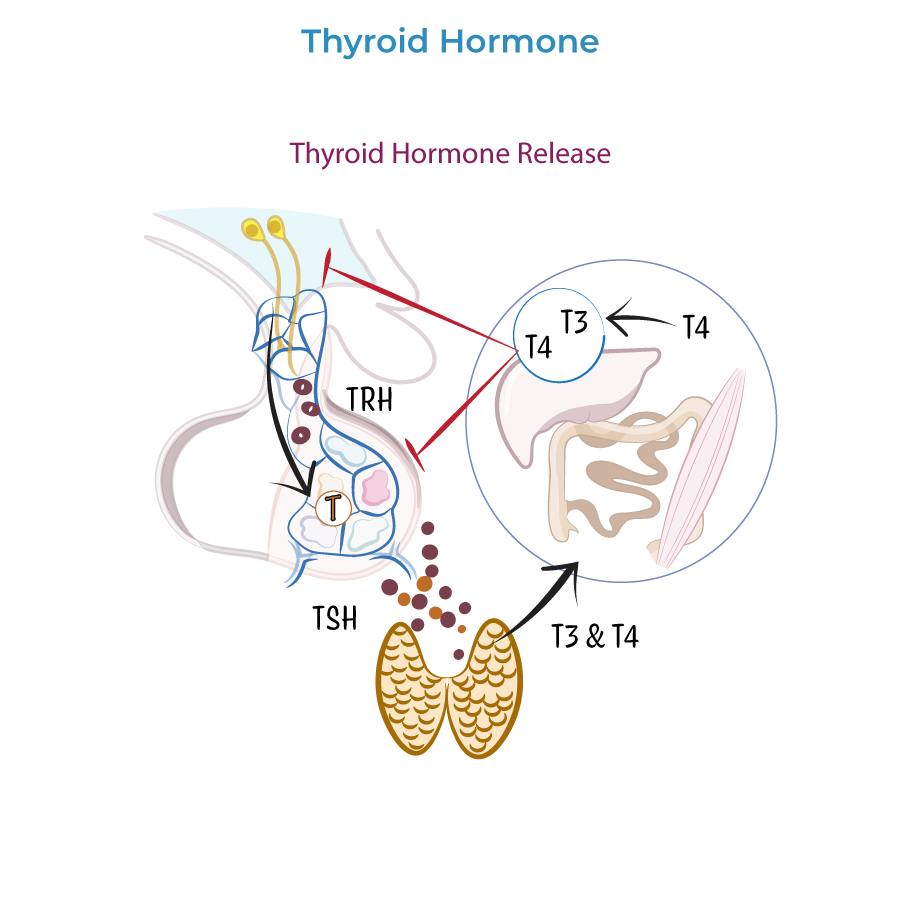
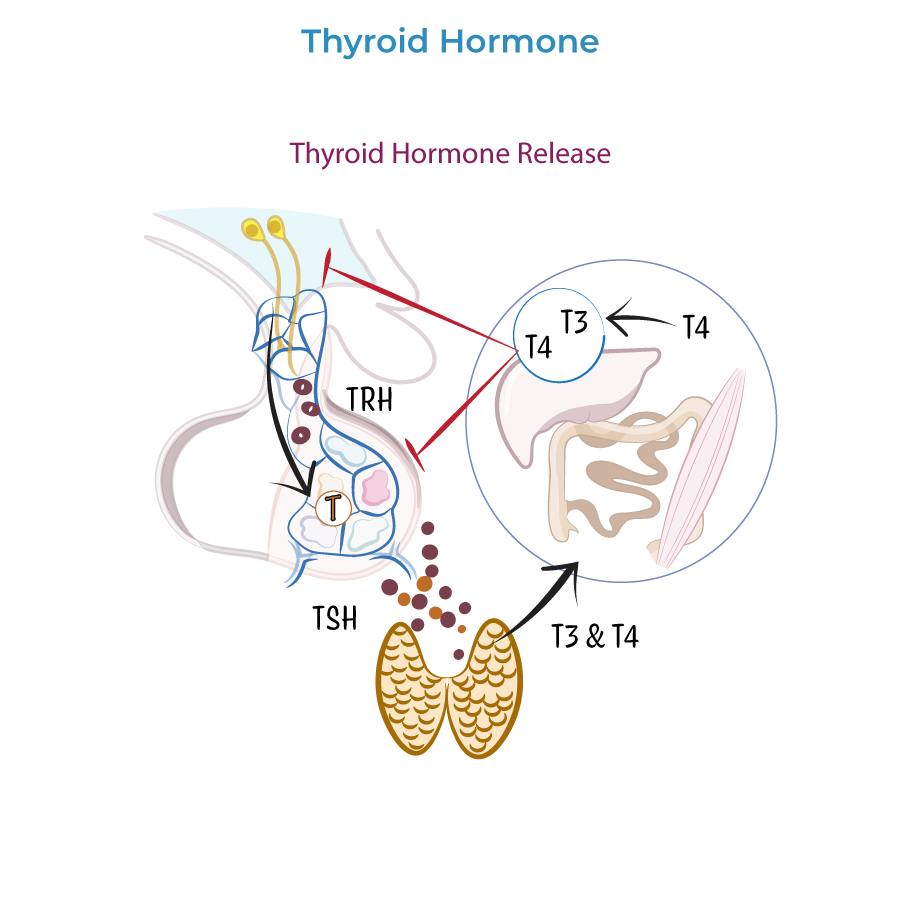
2. Regulatory Pathway: Thyrotropin-releasing hormone (TRH) is released from the hypothalamus and carried in the pituitary circulation. In the anterior pituitary gland, TRH stimulates thyrotrophs (aka, tyrotropes) to release thyroid-stimulating hormone (TSH). TSH travels in the systemic circulation to its target organ, the thyroid, where it triggers release of the thyroid hormones, T3 and T4.
3. Negative Feedback: Via negative feedback at the hypothalamus and the anterior pituitary gland, thyroid hormones inhibit further secretion of TRH and TSH.
4. Hormone Activity: T3 is more biologically active than T4. Thyroid hormones travel to the peripheral tissues, where some T4 is deiodinated to T3.
Key Clinical Conditions
1. Primary Disorders: Pathology can be broadly categorized as hyperthyroidism, which produces thyrotoxicosis, or hypothyroidism, which produces myxedema.
2. Lab Findings - Hyperthyroidism: Hyperthyroidism is characterized by elevated levels of T3 and T4, low LDL (due to increased LDL receptors in the liver), and, if in the case of primary hyperthyroidism, low levels of TSH due to negative feedback on the pituitary.
3. Lab Findings - Hypothyroidism: Hypothyroidism is characterized by low levels of T3 and T4, hypercholesterolemia, and, in the case of primary hypothyroidism, high TSH.
4. Common Etiologies: Most common cause Hyperthyroidism: in the US is Graves disease" and "Hypothyroidism: Hashimoto thyroiditis.
- --
HIGH YIELD
Clinical Manifestations by System
Cardiovascular
1. Hyperthyroidism: tachycardia with palpitations. Patients experience dyspnea and chest pain and have systolic hypertension.
2. Hypothyroidism: bradycardia with reduced cardiac output. Patients experience dyspnea on exertion and are at risk for hypoventilation.
3. Normal thyroid function includes: Chronotropic and inotropic effects on the heart (heart rate and contractility).
Neuropsychiatric
1. Hyperthyroidism: hyperactivity, restlessness, anxiety, and insomnia. Patient have increased reflexes and fine motor tremors.
2. Hypothyroidism has the opposite effects: patients are hypoactive, fatigued, and experience weakness and depressed mood with slow reflexes.
Musculoskeletal
1. Hyperthyroidism: breaks down proteins and muscles, producing proximal weakness with normal levels of creatine kinase and accelerates bone growth and tissue turnover; thus, patients are at risk for osteoporosis and bone fractures.
2. Hypothyroidism also produces proximal weakness, but with myalgia; creatine kinase levels are often elevated. In children, it produces impaired bone formation and growth.
Gastrointestinal and Metabolism
1. Hyperthyroidism: more bowel movements, possibly with diarrhea, and appetite is increased.
2. Hypothyroidism: constipation and reduced appetite.
3. Hyperthyroidism: heat intolerance with increased sweating; patients have elevated basal metabolic rate with weight loss.
4. Hypothyroidism: cold intolerance and reduced sweating; patients have lower basal metabolic rates with weight gain, and possibly hyponatremia.
5. Normal thyroid functions include: Stimulate LDL receptors in the liver, Promote GI motility and carbohydrate absorption," and "Promote lipolysis in adipose tissue.
Dermatologic
1. Hyperthyroidism: vasodilation produces warm, moist skin; hair is often fine (thin diameter).
2. Hypothyroidism: patients have reduced blood flow with cool, dry skin. Hair is often coarse and brittle, and patients may have alopecia. Nails are brittle.
3. Hypothyroidism is often characterized by nonpitting edema and puffy facies, due to water retention – thus its alternative name, myxedema.
Reproductive
1. Hyperthyroidism: irregular or reduced menstrual flow, gynecomastia, lower libido, and possibly reduced fertility.
2. Hypothyroidism: similar effects, but gynecomastia is not common.
Ocular
1. Both hyper- and hypothyroidism: can produce periorbital edema.
2. Hyperthyroidism is also associated with exophthalmos, aka, proptosis, which is characterized by 'bulging' eyeballs due to inflammation around the eyes.
3. Lid retraction can also occur in hyperthyroidism due to increased sympathetic stimulation of the muscles of the eyelid.
Diagnostic Indicators
1. Goiter: Goiter = an enlarged thyroid gland. Goiter can be benign or a sign of underlying thyroid disease.
2. Wolff-Chaikoff Effect: In cases of excessive iodine exposure, the thyroid inhibits iodine organification, thereby avoiding over-production of thyroid hormone (the Wolff-Chaikoff effect).
3. Beta-Adrenergic Effects: Sympathetic nervous system: thyroid hormone increases beta adrenergic receptor numbers and sensitivity. This can help us predict the physiological roles of thyroid hormone and the pathology that results when there is too much or too little hormone activity.
- --
Beyond the Tutorial
Clinical Management
1. Hyperthyroidism treatment: Anti-thyroid medications, radioactive iodine ablation, beta-blockers for symptom control, surgical options.
2. Hypothyroidism treatment: Levothyroxine replacement therapy, dosing principles, monitoring parameters.
3. Subclinical disease management: Approach to abnormal labs without overt clinical manifestations.
Special Populations
1. Pregnancy considerations: Management modifications, fetal effects, postpartum thyroiditis.
2. Pediatric patients: Growth monitoring, developmental assessment, congenital hypothyroidism screening.
3. Elderly patients: Atypical presentations, dose adjustments, comorbidity considerations.
Emergency Management
1. Thyroid storm: Recognition, immediate treatment, supportive care.
2. Myxedema coma: Clinical features, management priorities, prevention strategies.
3. Post-surgical complications: Hypocalcemia, recurrent laryngeal nerve injury, management approach.
