PANCE - Supraventricular & Ventricular Arrhythmias
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Supraventricular & Ventricular Arrhythmias tutorial, as well as points of interest that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for PANCE.
Below is information not explicitly contained within the tutorial but important for PANCE.
- --
VITAL FOR PANCE
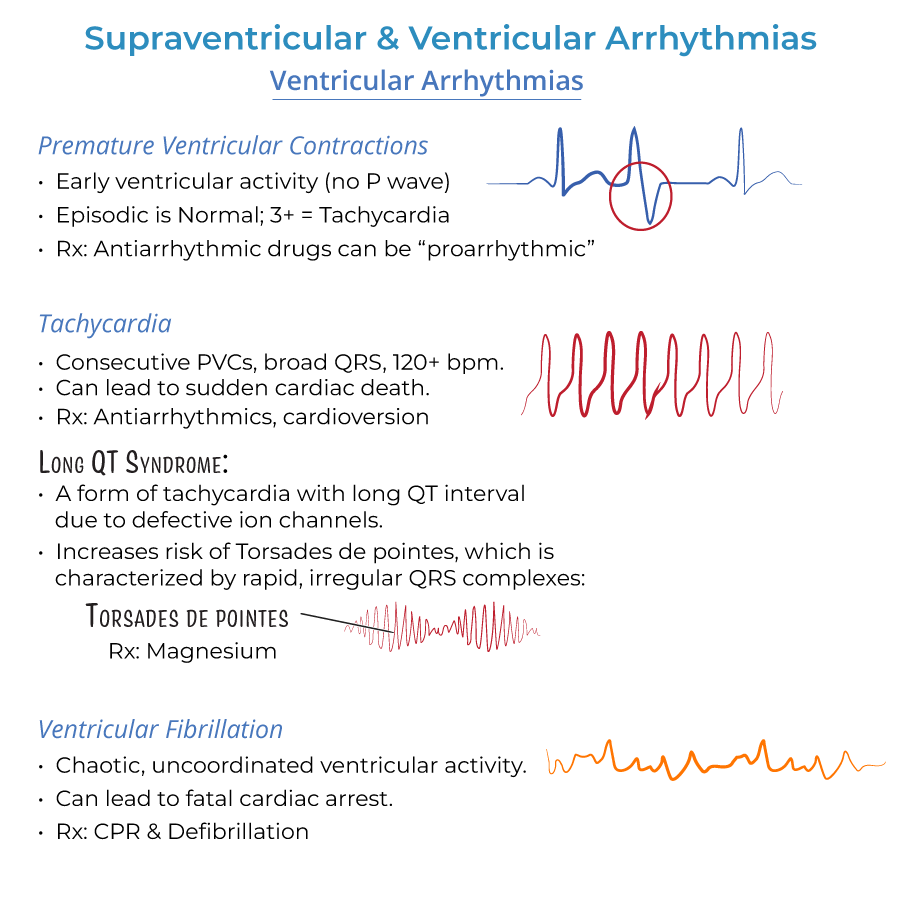
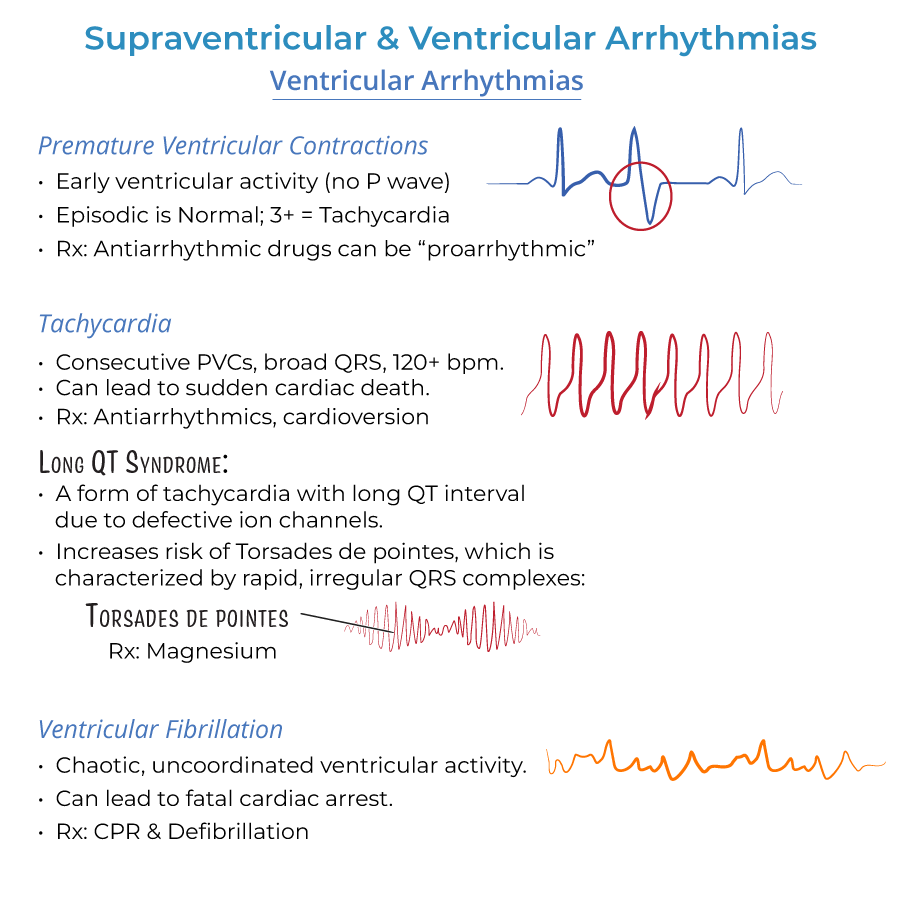
Arrhythmia Recognition
1. Atrial Flutter: Rapid, regular P waves give ECG "sawtooth" appearance. Atria beat ~300 beats/minute. Only ½ - 1/3 of the electrical impulses make it through the AV node.
2. Atrial Fibrillation: Rapid, irregular and indiscrete P waves on ECG. Atria do not contract in coordinated fashion, but send fast and irregular signals to ventricles.
3. Wolff-Parkinson-White Syndrome: Short PR interval and positive delta wave at beginning of broad QRS complex; delta wave reflects early depolarization.
4. Ventricular Tachycardia: 3+ consecutive beats 120+ beats/minute; abnormal ventricular automacy.
Emergency Management
1. Unstable Arrhythmias: Direct-current cardioversion therapy is preferred for WPW; Cardioversion for ventricular tachycardia.
2. Ventricular Fibrillation: CPR & Defibrillation.
3. Torsades de Pointes: Magnesium.
4. Cardiac Arrest: Both asystole and pulseless electrical activity can lead to cardiac arrest.
Pharmacologic Management
1. Atrial Flutter/Fibrillation: Rate control with drugs: beta-blockers, calcium channel blockers (verapamil, diltiazem). Rhythm control with antiarrhythmics.
2. Anticoagulation: Anticoagulants (warfarin) are used to prevent thromboembolism in atrial flutter/fibrillation.
3. Critical Medication Cautions: Beware digoxin/nondihydropyridine calcium channel blockers to WPW patients, as they may trigger ventricular fibrillation (fatal).
4. Chronic Management: Long term treatment of WPW may require catheter ablation.
- --
HIGH YIELD
Clinical Presentations
1. Atrial Flutter: May be none. Or, may cause palpitations, and reduced CO, difficulty breathing, weakness, chest discomfort, syncope.
2. Atrial Fibrillation: May be asymptomatic. Or, may experience lack of energy, fast, irregular pulse, difficulty breathing, palpitations, chest discomfort, dizziness.
3. Premature Beats: Palpitations, "skipped" beats.
4. Ventricular Tachycardia: May be asymptomatic if duration is short (aka, paroxysmal) or rate is not excessive; If sustained, palpitations, difficulty breathing, chest pain, dizziness, fainting, death.
Risk Factors
1. Atrial Flutter: Commonly occurs in healthy people, but risk increases with other cardiac conditions, binge alcohol consumption, diabetes.
2. Atrial Fibrillation: Other cardiac problems, hyperthyroidism, obesity, diabetes, lung disease, binge alcohol consumption.
3. Premature Beats: Stress, caffeine, alcohol, hypoxia, electrolyte imbalances. Heart disease, pulmonary disease, and scarring can also interfere with normal electrical activity.
4. Ventricular Arrhythmias: Heart disease, electrolyte imbalances, medications.
Diagnostic Evaluation
1. Atrial Fibrillation Workup: Echocardiography to check for structural defects, thyroid function tests.
2. Long QT Syndrome: Long QT interval on ECG, reflects defective ion channels.
3. Torsades de Pointes: Rapid, irregular QRS complexes "spiral" around baseline, as ventricular rate varies from cycle to cycle.
4. WPW Associated Conditions: Associated with Ebstein anomaly, displaced tricuspid valve.
Complications & Clinical Concerns
1. Atrial Flutter: When coupled with other cardiac complications, can lead to stroke, makes heart work more difficult, ventricular weakening, and coagulation is more likely. Patients may have periods of atrial fibrillation.
2. Atrial Fibrillation: Stroke, systemic emboli. Must rule out Wolff-Parkinson-White Syndrome before prescribing AV-node blocking drugs.
3. Premature Beats: Can develop flutter/fibrillation.
4. Ventricular Tachycardia: Can lead to heart failure, unconsciousness, sudden death by cardiac arrest.
- --
Beyond the Tutorial
Clinical Decision Making
1. Differentiating Narrow vs. Wide Complex Tachycardias: Approach to distinguishing supraventricular from ventricular causes of tachycardia.
2. ACLS Protocol Application: Implementation of current advanced cardiac life support algorithms for various arrhythmias.
3. Determining Hemodynamic Stability: Assessment techniques to determine if a patient with an arrhythmia requires immediate intervention.
4. Risk Stratification: Tools to determine which patients with arrhythmias need hospitalization versus outpatient management.
Procedural Considerations
1. Cardioversion Preparation: Pre-procedure checklist including anticoagulation status, NPO status, and sedation considerations.
2. Defibrillation Technique: Proper pad placement, energy selection, and safety considerations.
3. Temporary Pacing: Indications and basic management of transcutaneous and transvenous temporary pacing.
4. Post-Procedure Monitoring: Essential observations following cardioversion, defibrillation, or other arrhythmia interventions.
Medication Management
1. Antiarrhythmic Classification: Vaughan Williams classification and clinical applications of each class.
2. Anticoagulation Selection: Factors influencing choice between warfarin and direct oral anticoagulants.
3. Drug Interactions: Clinically significant interactions between antiarrhythmics and other commonly prescribed medications.
4. Rate Control Strategies: Dosing and titration of beta blockers and calcium channel blockers for rate control.
Primary Care Considerations
1. Screening Recommendations: When to screen for arrhythmias in asymptomatic patients with risk factors.
2. Preoperative Evaluation: Arrhythmia assessment before non-cardiac surgery.
3. Exercise Recommendations: Activity guidelines for patients with various arrhythmias.
4. Coordination of Care: When to refer to electrophysiology and ongoing co-management strategies.
