PANCE - Pulmonary Embolism and Deep Vein Thrombosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for Physician Assistant National Certifying Examination (PANCE) from the Pulmonary Embolism & Deep Vein Thrombosis tutorial, focusing on clinical recognition, diagnosis, and management that are essential for certification. See the tutorial notes for further details and relevant links.
 4. Multiple Risk Factors: Patients with several predisposing elements have significantly higher risk (e.g., pregnant women on bed rest).
5. Preventable Factors: Many risk factors are modifiable through preventive interventions.
Below is information not explicitly contained within the tutorial but important for the Physician Assistant National Certifying Examination.
4. Multiple Risk Factors: Patients with several predisposing elements have significantly higher risk (e.g., pregnant women on bed rest).
5. Preventable Factors: Many risk factors are modifiable through preventive interventions.
Below is information not explicitly contained within the tutorial but important for the Physician Assistant National Certifying Examination.
- --
VITAL FOR PANCE
Etiology & Pathophysiology
1. Venous Thromboembolism: DVT and PE commonly occur together; the term "venous thromboembolism" describes their combined condition.
2. PE Mechanism: Pulmonary embolism occurs when pulmonary arteries are obstructed, most often by emboli that travel from deep veins of thighs/pelvis.
3. Pathogenesis Process: Clot forms in deep vein → fragment breaks off → travels through IVC → right heart → pulmonary arteries → obstructs blood flow → impairs gas exchange.
4. Nonthrombotic Sources: Air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors can also cause PE.
5. Complications: Pulmonary hypertension, right heart failure, and pulmonary infarction; PE is a leading cause of cardiovascular-related death.
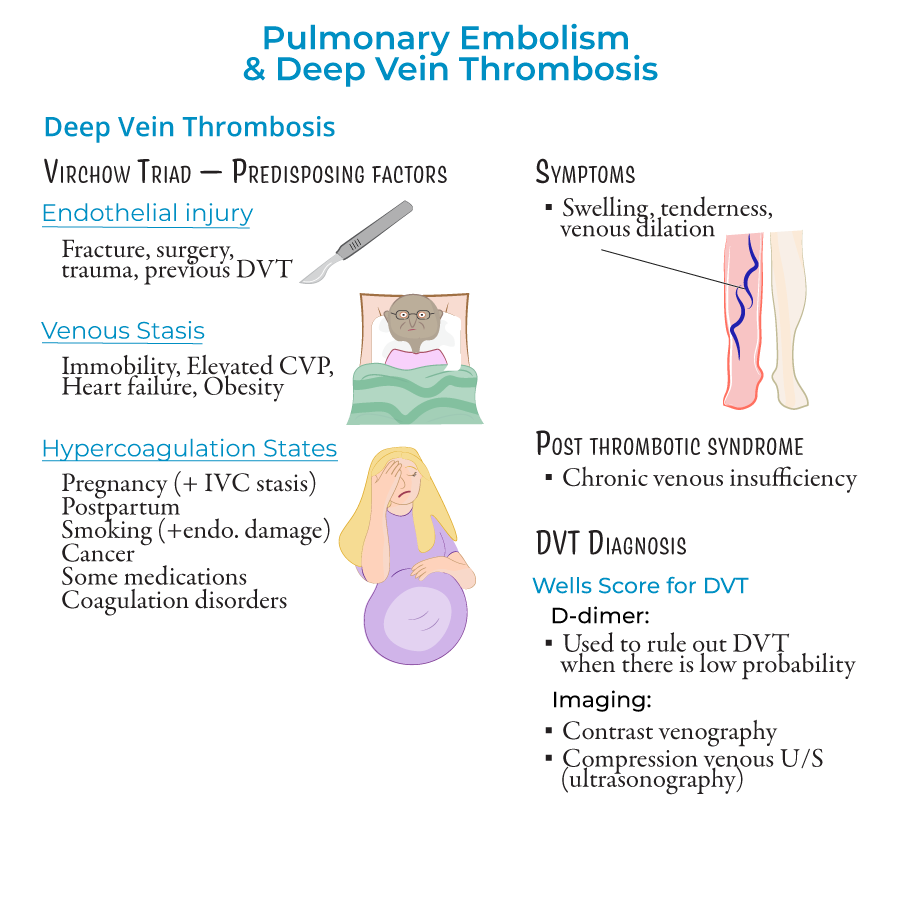
Risk Factors: Virchow's Triad
1. Endothelial Injury:
- Fracture, surgery, trauma, or previous DVT
- Triggers clotting cascade when endothelium is damaged
- Smoking also associated with endothelial damage
- Immobility (bed rest, long flights)
- Elevated central venous pressure
- Heart failure
- Obesity
- Pregnancy and postpartum period (pregnancy also associated with IVC stasis)
- Cancer
- Hormonal medications (contraceptives, replacement therapies)
- Coagulation disorders (Factor V Leiden)
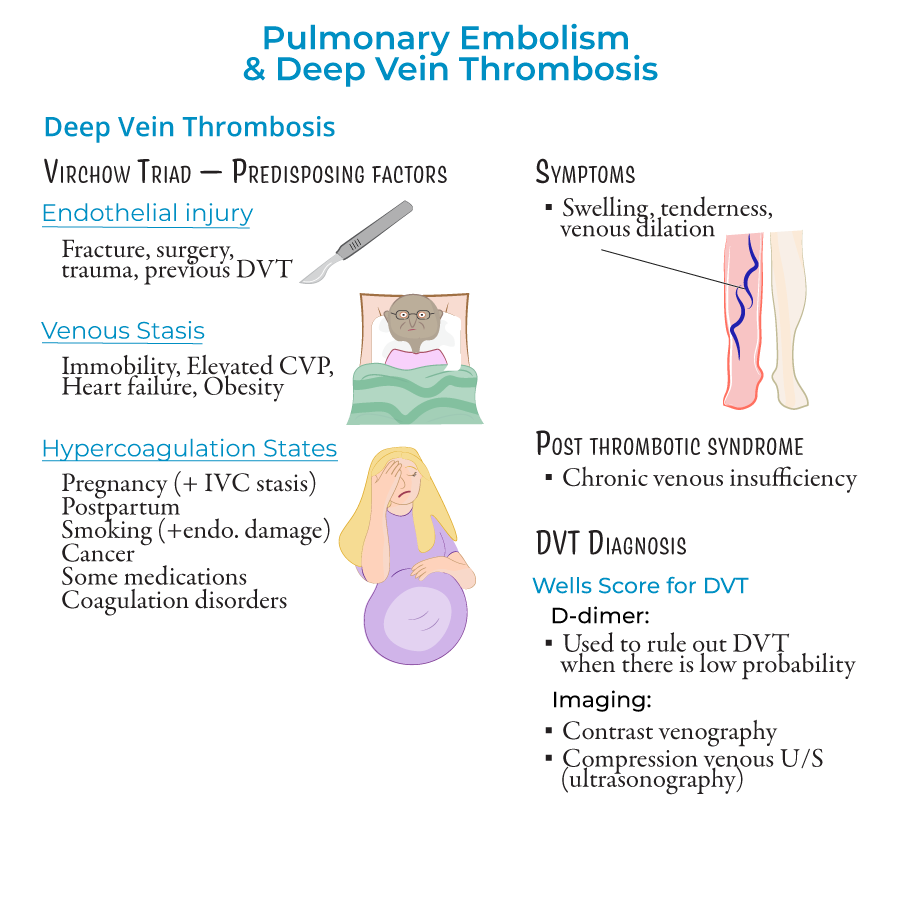 4. Multiple Risk Factors: Patients with several predisposing elements have significantly higher risk (e.g., pregnant women on bed rest).
5. Preventable Factors: Many risk factors are modifiable through preventive interventions.
4. Multiple Risk Factors: Patients with several predisposing elements have significantly higher risk (e.g., pregnant women on bed rest).
5. Preventable Factors: Many risk factors are modifiable through preventive interventions.
Clinical Manifestations
1. DVT Presentation:
- Unilateral leg swelling, tenderness, venous dilation
- Can occur in upper body (less common)
- May be asymptomatic
- Post-thrombotic syndrome if venous valves are damaged
- Dyspnea, tachypnea (rapid breathing)
- Chest pain
- Hypoxemia and ventilation-perfusion mismatch
- Respiratory alkalosis
- Tachycardia
- Right heart failure possible
- By risk: massive (high risk), intermediate (submassive), low risk
- By location: saddle (at pulmonary trunk bifurcation), lobar, segmental, subsegmental
Diagnostic Approach
1. Clinical Probability Assessment:
- Wells Score for DVT: Based on swelling, edema, likelihood of alternative diagnosis
- Wells Score for PE: ≥4 indicates PE likely; <2 low probability, 2-6 moderate, >6 high probability
- D-dimer: >500 ng/mL indicates possible PE/DVT requiring further testing
- Useful to rule out low-probability cases
- Chest CT with angiography: Most widely used; visualizes pulmonary arterial disruption
- Ventilation-perfusion scan: Non-invasive test for blood clot detection
- Chest X-ray: May show atelectasis, Hampton hump (pulmonary infarction), Westermark sign (oligemic areas), pleural effusion
- Venous ultrasonography with compression: Verifies thrombus presence
- Contrast venography: Alternative method
- ECG: May show sinus tachycardia; S1Q3T3 pattern (S wave in lead I, inverted Q and T waves in lead III)
- Thrombi characteristics: Premortem thrombi display lines of Zahn (layers of fibrin, RBCs, platelets)
Treatment & Management
1. Supportive Therapy:
- Oxygen administration when saturation <90%
- Saline for fluid management
- Vasopressors if hemodynamically unstable
- Short-term: Heparin, enoxaparin, or fondaparinux
- Long-term: Warfarin
- Monitoring: Assess for complications including heparin-induced thrombocytopenia
- Embolectomy or clot dissolution for severe cases to restore pulmonary arterial flow
- Mechanical: Sequential compression devices (SCDs) to prevent venous stasis
- Pharmacologic: Low-dose enoxaparin or heparin in selected patients
- --
HIGH YIELD
Clinical Decision Making
1. When to Suspect DVT: Unilateral leg swelling, tenderness, venous dilation; may be asymptomatic.
2. When to Suspect PE: Unexplained dyspnea, tachypnea, chest pain, hypoxemia; altered mental status in elderly.
3. Risk Assessment: Identifying patients with multiple Virchow's Triad elements who require heightened vigilance.
4. Diagnostic Challenges: PE diagnosis can be difficult due to nonspecific symptoms and signs.
5. Clinical Probability Interpretation: Utilizing Wells Scores appropriately to guide further testing.
Diagnostic Test Selection & Interpretation
1. D-dimer Utilization: Rule-out test for low-probability cases; levels >500 ng/mL warrant further investigation.
2. Imaging Selection:
- CT angiography as first-line for suspected PE
- Ultrasonography with compression for suspected DVT
- Hampton Hump: Wedge-shaped shadow indicating pulmonary infarction, typically in lower lobes
- Westermark Sign: Focal oligemia appearing as area of poor perfusion
Treatment Decision Points
1. Anticoagulation Initiation: When to start therapy based on clinical suspicion and risk assessment.
2. Supportive Care Decisions: Oxygen, fluid, and hemodynamic support based on presentation.
3. Advanced Intervention Selection: Determining candidates for embolectomy or thrombolysis.
4. Prophylaxis Decision-Making: Identifying high-risk patients requiring preventive measures.
5. Monitoring Requirements: Appropriate surveillance for treatment efficacy and complications.
DVT Prevention Strategies
1. Mechanical Prophylaxis: Sequential compression devices (SCDs) prevent venous stasis in hospitalized patients.
2. Pharmacologic Prophylaxis: Low-dose anticoagulants (enoxaparin or heparin) for selected high-risk patients.
3. Early Mobilization: Encouraging movement to prevent stasis when appropriate.
4. Patient Education: Teaching about risk factors and preventive measures.
5. Risk Factor Modification: Addressing modifiable elements of Virchow's Triad.
Complication Recognition & Management
1. Pulmonary Infarction: Small emboli causing tissue ischemia; Hampton Hump on X-ray.
2. Pulmonary Hypertension: Can result from PE; monitor for signs of right heart strain.
3. Right Heart Failure: PE complication requiring prompt intervention.
4. Heparin-Induced Thrombocytopenia: Serious complication of anticoagulant therapy.
5. Post-thrombotic Syndrome: Long-term DVT complication from venous valve damage.
- --
Beyond the Tutorial
Differential Diagnosis
1. Acute Coronary Syndrome: Chest pain, dyspnea, ECG changes; distinguishing features include cardiac biomarkers.
2. Pneumonia: Fever, productive cough, focal findings on exam and imaging; may coexist with PE.
3. Aortic Dissection: Tearing chest pain, pulse deficits, widened mediastinum on imaging.
4. Pneumothorax: Sudden-onset pleuritic pain, decreased breath sounds, hyperresonance.
5. Musculoskeletal Pain: Reproducible with palpation, normal oxygenation, no risk factors for PE.
Advanced Pharmacologic Considerations
1. Direct Oral Anticoagulants: Role in PE/DVT treatment, advantages and limitations.
2. Thrombolytic Therapy: Indications, contraindications, and administration protocols.
3. Bridging Anticoagulation: Management during transitions of therapy.
4. Inferior Vena Cava Filters: Indications, placement, and removal considerations.
5. Anticoagulation in Special Populations: Renal dysfunction, pregnancy, cancer, obesity.
Clinical Pearls & Pitfalls
1. Silent PE: May be present without typical symptoms, especially in elderly or chronically ill.
2. Upper Extremity DVT: Consider in patients with central venous catheters, pacemakers, or IV drug use.
3. Saddle Embolus: Often causes significant hemodynamic compromise requiring aggressive management.
4. Subsegmental PE: Management controversies regarding anticoagulation necessity.
5. Wells Score Limitations: Clinical judgment remains essential, as scoring systems have limitations.
Procedural Considerations
1. CT Angiography Technique: Contrast timing, breath-holding, and interpretation pearls.
2. Ultrasound Technical Aspects: Compression techniques, Doppler assessment, limitations.
3. Arterial Blood Gas Sampling: Technique, interpretation, and integration with clinical findings.
4. Central Line Placement: Avoiding complications in patients on anticoagulation.
5. Thrombolytic Administration: Monitoring protocols and emergency response to complications.
Long-Term Management
1. Anticoagulation Duration: Risk-based approach to determining treatment length.
2. Recurrent VTE Prevention: Strategies for patients with prior events.
3. Post-PE Functional Assessment: Evaluating exercise capacity and cardiopulmonary function.
4. Chronic Thromboembolic Pulmonary Hypertension: Recognition and management approaches.
5. Patient Education Topics: Symptom recognition, medication adherence, lifestyle modifications.
