PANCE - Myocardial Infarction Symptoms, Diagnosis, & Treatments
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for Physician Assistant National Certifying Examination (PANCE) from the Myocardial Infarctions: Diagnosis & Treatment tutorial, focusing on clinical recognition, diagnosis, and management that are essential for certification. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for the Physician Assistant National Certifying Examination.
Below is information not explicitly contained within the tutorial but important for the Physician Assistant National Certifying Examination.
- --
VITAL FOR PANCE
Epidemiology & Risk Factors
1. Demographic trends: Incidence of myocardial infarctions is declining in high-income countries but rising in middle- and low-income countries.
2. Population distribution: Within the United States, MI incidence after age 35, from highest to lowest: Black males > Black females > White males > White females.
3. Gender patterns: First MI occurs approximately 10 years earlier in men than women, possibly related to risk factors such as smoking and hyperlipidemia.
4. Mortality disparities: Despite overall declining rates, mortality remains higher in women than male peers, especially for young and/or minority women.
5. Modifiable risk factors:
- Dyslipidemia
- Diabetes mellitus
- Hypertension
- Smoking (including e-cigarettes)
- Obesity
- Psychosocial stress
- Alcohol consumption
- Poor diet (low in fruits and vegetables)
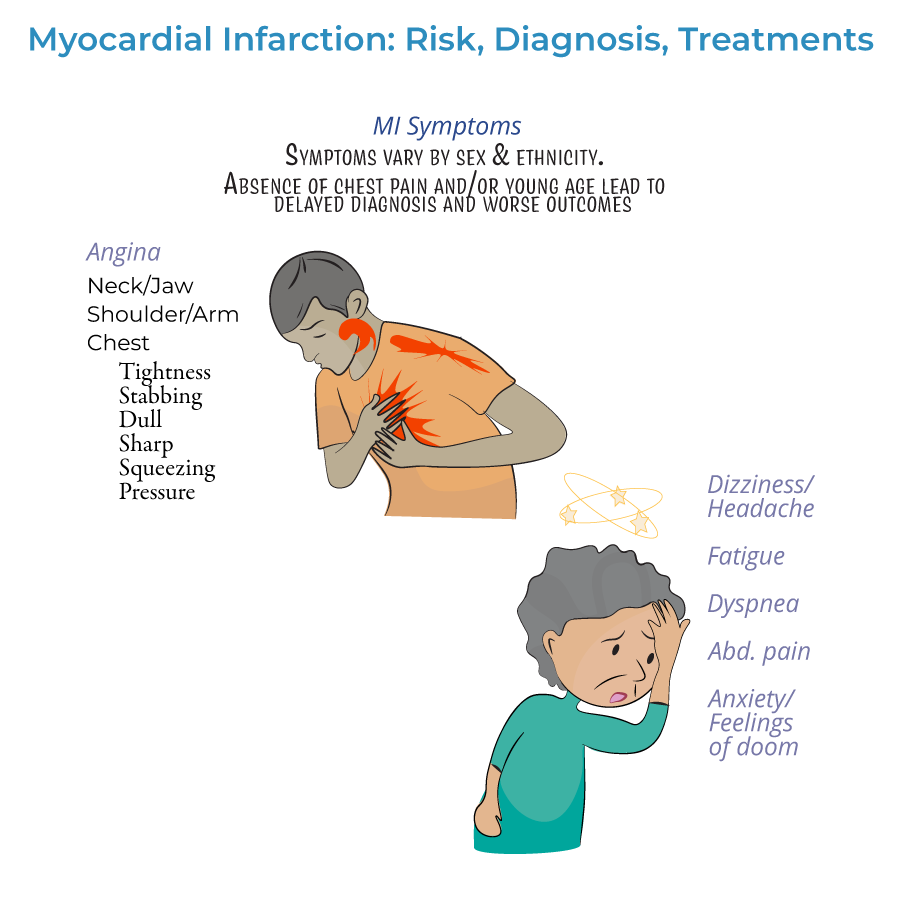
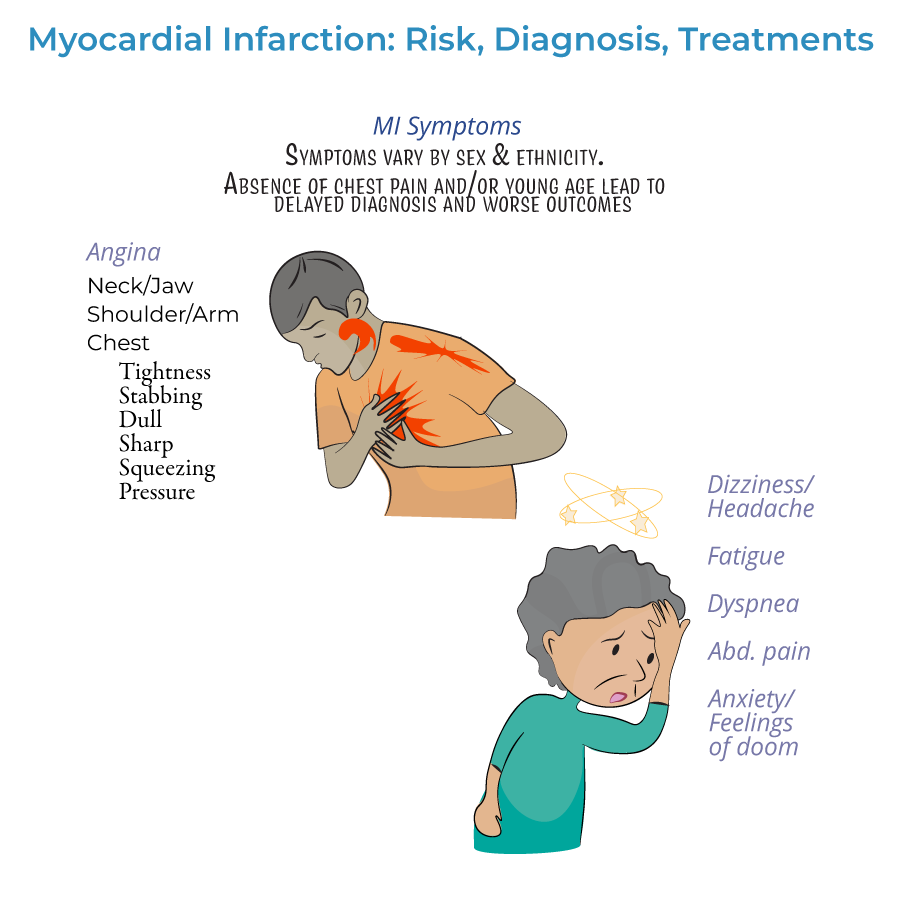
Clinical Presentation & Recognition
1. Definition: Myocardial infarction is defined as myocardial injury with ischemia.
2. Symptom timeline:
- Prodromal symptoms: Days, weeks, or months prior to the heart attack
- Acute symptoms: Experienced at the time of the event
- Silent MI: No noticeable symptoms
- Gastrointestinal issues (nausea, vomiting, indigestion)
- Extreme fatigue, exhaustion, or sleep disturbances
- Headaches, dizziness, lightheadedness
- Shortness of breath (dyspnea)
- Anxiety or sense of impending doom
Diagnostic Approach
1. ECG assessment:
- Should be administered as soon as possible when MI is suspected
- Re-administered frequently to observe the evolution of the infarction
- Distinguishes between ST-segment elevated (STEMI) or Non-ST elevated (NSTEMI) myocardial infarctions
- Q-wave abnormalities may indicate size/location of current MI, or may indicate a prior MI
- Lateral infarction: Leads I and aVL; left circumflex artery
- Apical infarction: Leads V5 and V6; left circumflex or right coronary arteries
- Anterior infarction: Leads V3 and V4; left anterior descending artery
- Anteroseptal infarction: Leads V1 and V2; proximal left anterior descending artery
- Inferior infarction: Leads II, aVF, and III; right coronary artery or left circumflex artery
- Right ventricular infarction: Requires additional leads V3R through V6R
- Posterolateral infarction: Requires additional leads V7-V9; right coronary or left circumflex artery
- Cardiac troponin is key to diagnosis
- Help distinguish between NSTEMI and unstable angina (only NSTEMI shows troponin elevation)
- Both cardiac troponin I and CK-MB peak within 24 hours of MI and fall to normal levels over time
Management & Treatment
1. Time-dependent approach: Treatment should begin as soon as possible, ideally before hospital arrival, to reduce myocardial necrosis.
2. Pre-hospital treatment:
- Oxygen administration when oxygen saturation is less than 90%
- Aspirin for antiplatelet effects
- Nitrates for chest pain (morphine if nitrates ineffective)
- Vary by severity of infarction
- Include percutaneous coronary intervention (angioplasty), coronary bypass grafting, or fibrinolytic drugs
- STEMI patients should receive emergency PCI; if unavailable, fibrinolytic drugs must be given as soon as possible
- Unstable, complicated NSTEMI often requires immediate PCI or CABG
- Uncomplicated NSTEMI patients may wait longer (a day or two), and revascularization may not be necessary
- Antiplatelets (aspirin, clopidogrel, or others)
- Anticoagulation drugs (unfractionated or low molecular weight heparin)
- Beta-blockers (or calcium-channel blockers)
- Statins
- ACE-inhibitors
Long-Term Management
1. Risk factor modification: Diet, exercise, smoking cessation, and stress management.
2. Medication management: Long-term therapy for hypertension and hyperlipidemia.
3. Disease progression awareness: MI is an important cause of heart failure, which is itself a significant cause of death.
4. Patient education: Many patients, especially women, are unaware of risk factors and symptoms—education is crucial.
5. Social determinants: Unawareness is a significant obstacle to prevention and treatment of myocardial infarction.
- --
HIGH YIELD
Clinical Recognition Pearls
1. Atypical presentations: Not all patients experience classic angina—maintain high index of suspicion.
2. Prodromal recognition: Symptoms in days to months before acute MI may include fatigue, sleep disturbances, or vague discomfort.
3. Pain radiation patterns: May radiate from chest to arms, neck, jaw, or back—radiation patterns help confirm diagnosis.
4. Women's presentation: More likely to present with atypical symptoms and have higher mortality.
5. Young patients: Often experience missed/delayed diagnosis due to low clinical suspicion despite presentation.
ECG Interpretation Essentials
1. Timing importance: ECG should be performed ASAP when MI is suspected, with serial ECGs to monitor evolution.
2. STEMI vs. NSTEMI differentiation: Critical for determining treatment pathway and urgency.
3. Localization correlation: Different lead changes indicate specific coronary territories:
- Anterior (V3-V4): Left anterior descending artery
- Anteroseptal (V1-V2): Proximal left anterior descending artery
- Lateral (I, aVL): Left circumflex artery
- Inferior (II, III, aVF): Right coronary artery (or left circumflex in ~10% with left dominance)
Biomarker Utilization
1. Diagnostic hierarchy: Cardiac troponin is key to diagnosis of myocardial infarction.
2. Temporal pattern: Both cardiac troponin I and CK-MB peak within 24 hours of MI.
3. NSTEMI vs. unstable angina: Only NSTEMI shows rising/falling troponin levels—crucial for treatment decisions.
4. Serial measurements: More valuable than single determinations for diagnosis.
5. Integration with clinical findings: Always interpret biomarkers in context of symptoms and ECG findings.
Treatment Decision-Making
1. Reperfusion timing: Earlier treatment leads to better myocardial salvage and outcomes.
2. STEMI management: Emergency PCI preferred; if unavailable, immediate fibrinolytic therapy.
3. NSTEMI approach: Risk stratification guides timing of intervention—unstable patients need immediate care.
4. Pre-hospital initiation: Early oxygen (when indicated), aspirin, and nitrates can limit infarct size.
5. Pharmacotherapy selection: Comprehensive approach with antiplatelets, anticoagulants, beta-blockers, statins, and ACE inhibitors.
Special Population Considerations
1. Women: Higher mortality rates, more atypical presentations, first MI approximately 10 years later than men.
2. Racial/ethnic disparities: Black males have highest incidence after age 35, followed by Black females.
3. Young patients: Often experience missed or delayed diagnosis due to low clinical suspicion.
4. Health literacy impact: Many patients, especially women, lack knowledge about risk factors and symptoms.
5. Risk factor clusters: Combinations of risks like smoking, dyslipidemia, and diabetes significantly increase MI probability.
- --
Beyond the Tutorial
Differential Diagnosis
1. Aortic dissection: Sharp, tearing pain; widened mediastinum; pulse deficits.
2. Pulmonary embolism: Sudden dyspnea, tachycardia, hypoxemia; risk factors for DVT.
3. Pericarditis: Pleuritic chest pain relieved by sitting forward; diffuse ST elevations.
4. Pneumothorax: Sudden chest pain and dyspnea; decreased breath sounds; hyperresonance.
5. Gastroesophageal disorders: Pain often related to meals; may improve with antacids.
Risk Stratification Tools
1. TIMI Risk Score: Predicts 14-day outcomes in ACS patients.
2. GRACE Risk Score: Predicts in-hospital and 6-month mortality.
3. HEART Score: Stratifies chest pain patients in the emergency department.
4. CRUSADE Score: Assesses bleeding risk in ACS patients.
5. Ottawa ACS Rule: Identifies low-risk chest pain patients.
Procedural Considerations
1. Coronary angiography: Indications, contraindications, and post-procedure monitoring.
2. Thrombolytic administration: Inclusion/exclusion criteria and management of complications.
3. Arterial access site care: Monitoring for bleeding and hematoma formation.
4. Temporary pacemaker management: Indications and care for patients with high-grade AV blocks.
5. IABP and mechanical support: Basic understanding of indications and management.
Complications Management
1. Cardiogenic shock: Recognition, initial management, and indications for mechanical support.
2. Arrhythmias: Identification and management of post-MI dysrhythmias.
3. Mechanical complications: Early recognition of papillary muscle rupture, ventricular septal defect, free wall rupture.
4. Post-MI pericarditis (Dressler syndrome): Timing, presentation, and management.
5. Heart failure: Recognition and initial management of acute heart failure post-MI.
Rehabilitation & Secondary Prevention
1. Cardiac rehabilitation: Components, benefits, and patient selection.
2. Secondary prevention targets: LDL <70 mg/dL, BP <130/80 mmHg, HbA1c <7%.
3. Return to activities: Evidence-based guidance for driving, exercise, work, and sexual activity.
4. Depression screening: Recognition and management of post-MI depression.
5. Patient education strategies: Techniques to improve medication adherence and lifestyle modifications.
