PANCE - Liver Disease Overview
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Liver Pathophysiology Overview tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for PANCE.
Below is information not explicitly contained within the tutorial but important for PANCE.
- --
VITAL FOR PANCE
Liver Disease Staging and Assessment
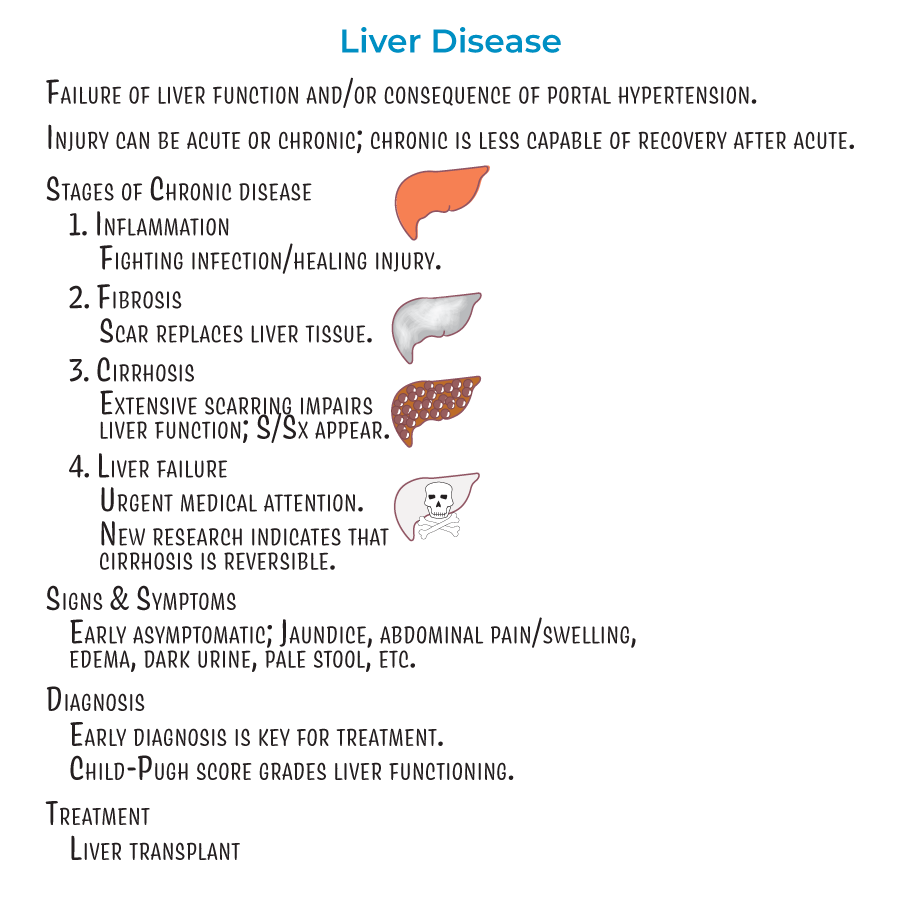
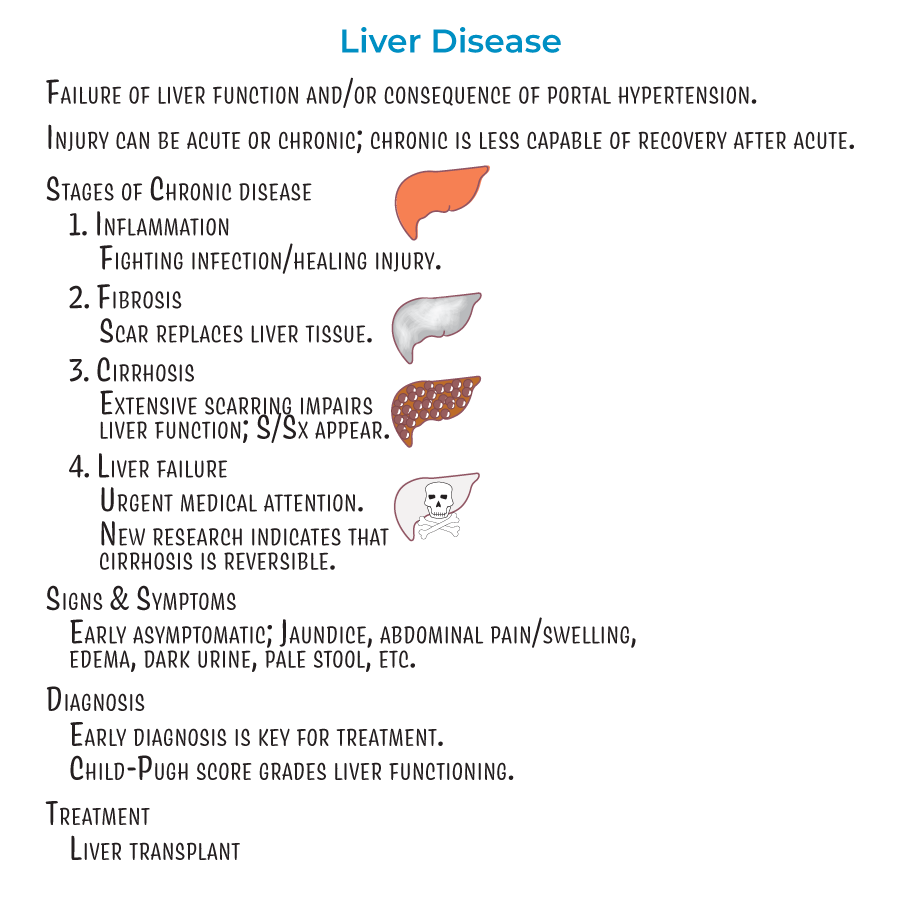
1. Progressive Stages: Liver disease progresses through four stages: inflammation (Stage 1), fibrosis (Stage 2), cirrhosis (Stage 3), and liver failure (Stage 4).
2. Clinical Recognition: Early stages of liver disease are asymptomatic; later stages can present with jaundice, abdominal pain and swelling, edema, dark urine, pale stool, and other signs of liver dysfunction and portal hypertension.
3. Diagnostic Approach: Early diagnosis is key for proper treatment, and even reversal, of damage.
4. Clinical Grading: The Child-Pugh score is used to grade liver functioning.
5. Treatment Options: In cases of cirrhosis or failure, transplants may be the best option.
Pathophysiology Fundamentals
1. Essential Functions: Liver plays key roles in energy metabolism, plasma protein synthesis, storage of nutrients, and degradation/detoxification/clearance of substances.
2. Critical Etiologies: Sources of liver injury include infections (viral hepatitis, Schistosomiasis), fatty liver disease (alcoholic and nonalcoholic), genetic disorders (hemochromatosis), autoimmune hepatitis, and biliary tract diseases.
3. Structural Changes: Cirrhosis is characterized by fibrosis and regenerative nodules with fatty changes.
4. Vascular Dynamics: Portal hypertension is increased hepatic blood pressure (above 6 mmHg).
5. Treatment Potential: Newer research indicates that cirrhosis (stage 3) is also reversible, not just stages 1 and 2.
Neurological Assessment
1. Encephalopathy Mechanism: Hepatic encephalopathy is the result of toxin build-up in the blood; ammonia is thought to be a key culprit.
2. Physical Finding: Asterixis or "flapping hand tremor" is the inability for a patient to sustain a posture due to involuntary, brief, "shock-like" movements.
3. Examination Technique: To test for asterixis, have a patient sit with closed eyes, outstretched arms, dorsiflexed wrists, and spread fingers – sudden "flapping" indicates asterixis.

- --
HIGH YIELD
Portal Hypertension Complications
1. Varices: Collateral blood vessels that form to provide alternative blood flow routes; pose significant risk for hemorrhage and are an important cause of GI bleeding.
2. Ascites: Accumulation of fluid in the peritoneum caused by systemic dilation that allows fluid leakage; a main complication of cirrhosis that can lead to peritonitis.
3. Spontaneous Bacterial Peritonitis: Acute infection resulting from bacteria and endotoxins leaking from the GI tract; can lead to septic shock if not treated promptly.
Multisystem Complications
1. Coagulation Abnormalities: Coagulopathy results from decreased storage of vitamin K and synthesis of clotting factors.
2. Physical Stigmata: Elevated estrogen levels can cause spider angiomas, palmar erythema, and gynecomastia.
3. Metabolic Derangements: Glucose metabolism is dynamically altered in liver damage so that patients can be hyper- or hypoglycemic.
4. Gastrointestinal Effects: Impaired bile flow can lead to hyperlipidemia, jaundice, and malabsorption of GI contents.
Organ System Failures
1. Renal Complications: Renal insufficiency and failure are the result of local vasoconstriction and inflammatory processes that reduce filtration.
2. SBP Connection: Spontaneous bacterial peritonitis is often a trigger for renal failure, inducing pro-inflammatory molecules that contribute to renal dysfunction.
3. Pulmonary Involvement: Hepatopulmonary syndrome involves pulmonary vasodilation leading to ventilation/perfusion mismatch, reduced oxygenation, and hypoxemia.
4. Malignancy Risk: Increased risk of liver cancer in progressive liver disease.
- --
Beyond the Tutorial
Clinical Workup
1. Laboratory Assessment: LFTs, coagulation studies, CBC, comprehensive metabolic panel, ammonia level, viral hepatitis serologies.
2. Imaging Studies: Ultrasound with Doppler (for portal hypertension), CT, MRI, transient elastography (FibroScan).
3. Specialized Testing: MELD-Na score calculation, endoscopy for varices, diagnostic paracentesis with fluid analysis.
4. Biopsy Considerations: Indications, contraindications, and complications of liver biopsy.
Management Strategies
1. Ascites Treatment: Sodium restriction (2g/day), diuretics (spironolactone as first-line, furosemide as adjunct), therapeutic paracentesis, TIPS for refractory cases.
2. Variceal Hemorrhage: Acute stabilization, vasoactive drugs (octreotide), antibiotic prophylaxis, endoscopic band ligation, non-selective beta-blockers for prevention.
3. Hepatic Encephalopathy: Lactulose titrated to 2-3 soft bowel movements daily, rifaximin for recurrent episodes, identification and treatment of precipitating factors.
4. SBP Management: Empiric antibiotics (third-generation cephalosporins), albumin administration, prophylaxis for high-risk patients.
Special Considerations
1. Medication Dosing: Adjustments for hepatic metabolism, avoiding hepatotoxic medications, monitoring for adverse effects.
2. Nutritional Support: Adequate protein intake (contrary to outdated practices), frequent small meals, micronutrient supplementation.
3. Screening Protocols: HCC surveillance with ultrasound every 6 months, varices screening with endoscopy.
4. Transplant Referral: Timing of referral, absolute and relative contraindications, management while awaiting transplantation.
Patient Education
1. Lifestyle Modifications: Alcohol cessation, weight management, dietary guidance, medication compliance.
2. Self-Monitoring: Recognition of red flag symptoms requiring immediate medical attention.
3. Vaccination: Importance of hepatitis A/B vaccines and annual influenza vaccination.
4. Prognosis Counseling: Discussing disease trajectory, treatment goals, and advanced care planning when appropriate.
