PANCE - Large Vessel Vasculitis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Large Vessel Vasculitis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR PANCE
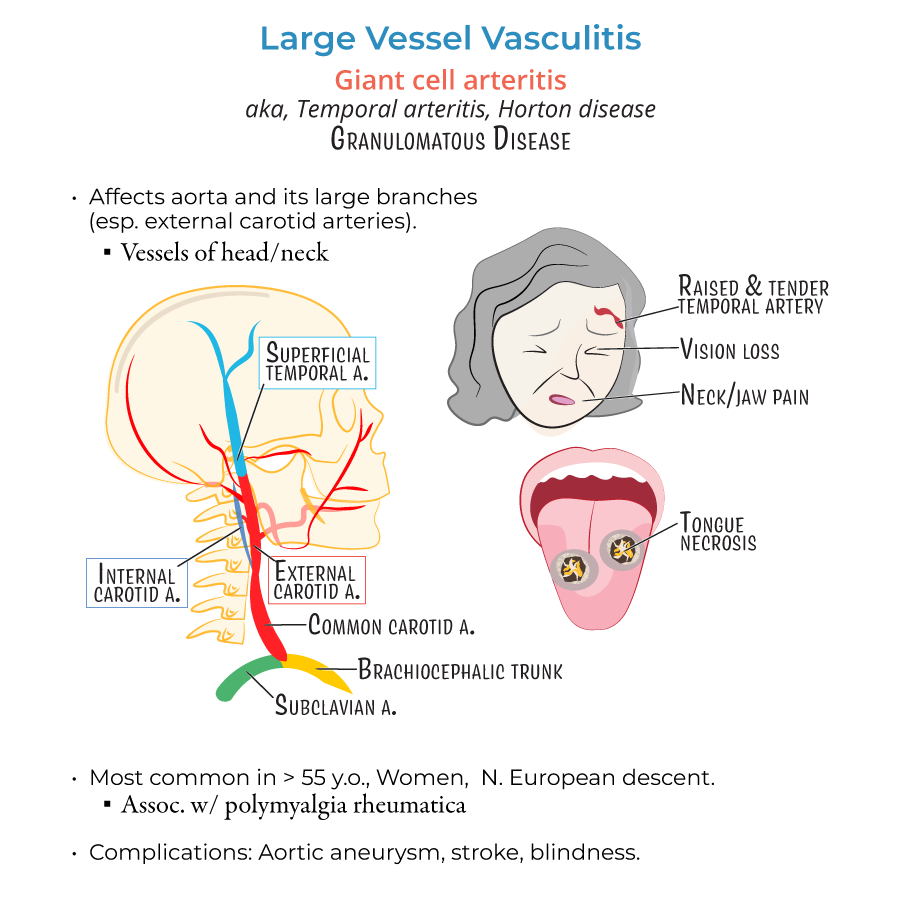
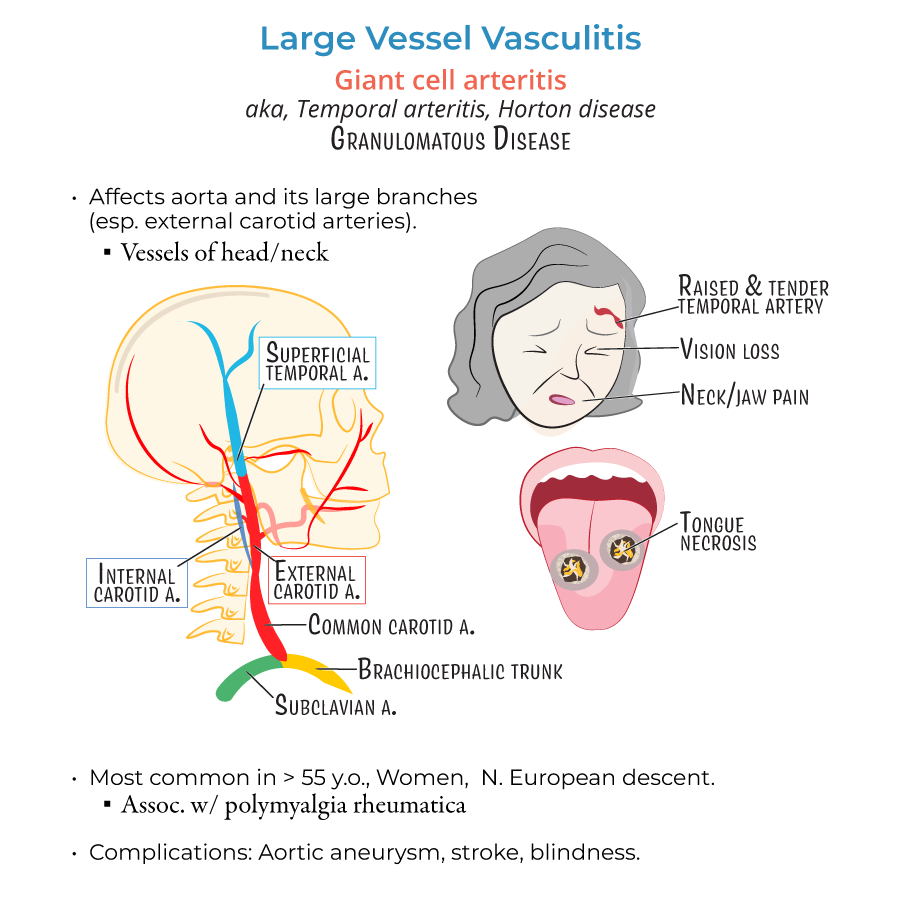
Giant Cell Arteritis (GCA)
1. Giant Cell Arteritis affects large vessels, particularly branches of the external carotid artery (e.g., temporal artery).
2. Typical demographic: women over 50 years, especially Northern European descent.
3. Classic symptoms:
- New-onset temporal headache
- Jaw claudication (pain with chewing)
- Visual symptoms (blurred vision, amaurosis fugax)
- Scalp tenderness
- Polymyalgia rheumatica association in ~50% of cases (proximal muscle pain/stiffness)
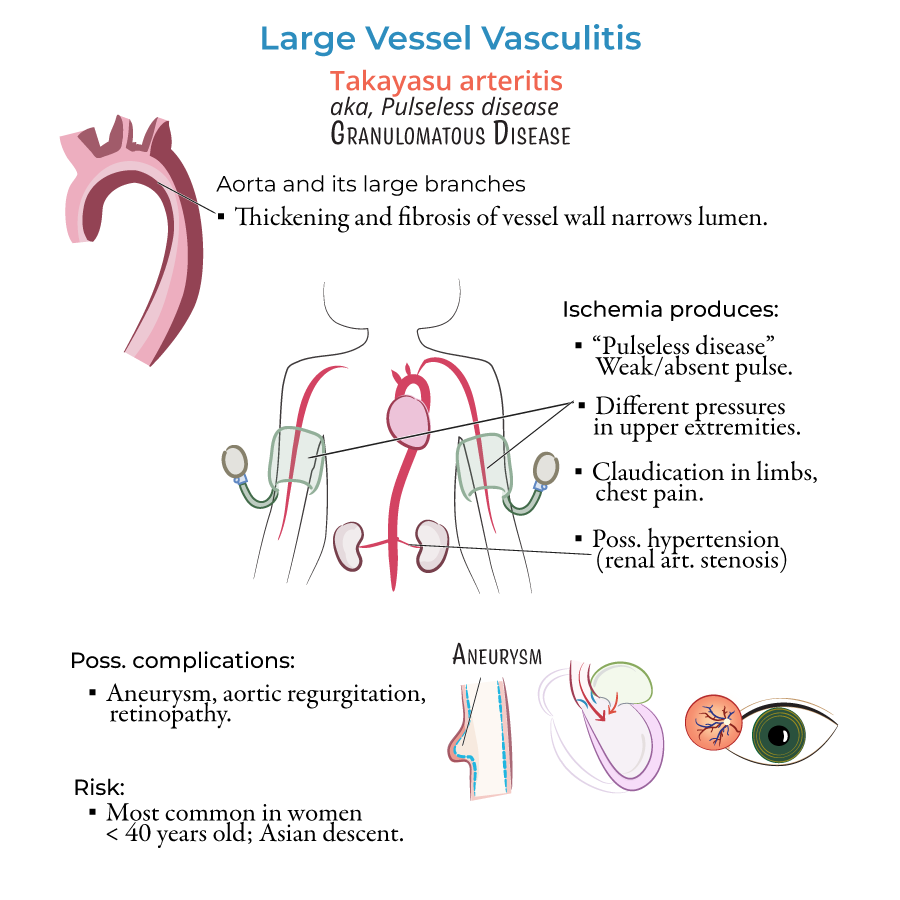
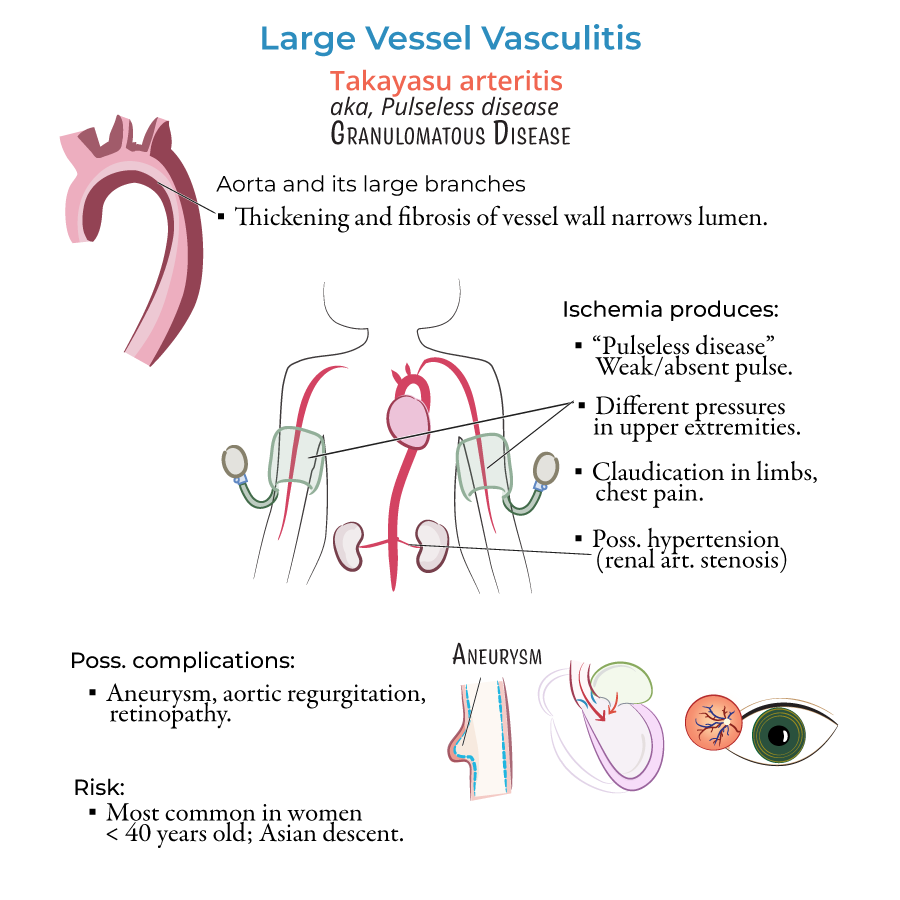
Takayasu Arteritis
8. Takayasu arteritis affects the aorta and its major branches, especially the subclavian and carotid arteries.
9. Typical demographic: women <40 years, especially of Asian descent.
10. Hallmark signs:
- Absent or diminished pulses
- Blood pressure discrepancy between arms (>10 mmHg)
- Arm or leg claudication
- Carotid or subclavian bruits
- --
HIGH YIELD
Pathology and Mechanism
1. Both GCA and Takayasu arteritis are granulomatous vasculitides of large vessels.
2. Histological features include:
- Multinucleated giant cells
- Chronic inflammatory infiltrates
- Destruction of the internal elastic lamina
- Intimal hyperplasia causing luminal narrowing
Diagnostic Workup
4. In GCA, temporal artery biopsy is the gold standard but biopsy can be negative due to segmental involvement.
5. Imaging for Takayasu: CT angiography or MR angiography to visualize arterial changes.
6. Elevated ESR and CRP support diagnosis in both GCA and Takayasu.
7. Blood pressure should be measured in both arms when suspecting Takayasu.
Clinical Management Nuances
8. In suspected GCA with visual symptoms, hospital admission and IV methylprednisolone may be appropriate.
9. Long-term steroid therapy requires monitoring for side effects: osteoporosis, hyperglycemia, infection.
10. Calcium, vitamin D supplementation, and possibly bisphosphonates are necessary for bone protection during long-term steroid use.
11. Consider steroid-sparing agents (e.g., methotrexate) for recurrent or refractory disease.
- --
Beyond the Tutorial
Patient Follow-Up and Complications
1. Monitor ESR and CRP levels serially to track disease activity and treatment response.
2. Annual imaging may be necessary in Takayasu patients to monitor for progression.
3. Aortic aneurysm screening is important in both diseases due to large vessel involvement.
4. Preventive care:
- Manage cardiovascular risk factors (e.g., BP, cholesterol)
- Encourage smoking cessation
- New vision changes
- Limb claudication
- New headaches or scalp tenderness
Special Considerations
7. Patients with Takayasu may develop secondary hypertension from renal artery stenosis.
8. Low-dose aspirin may be added to prevent thrombotic events in Takayasu and GCA patients with significant vascular involvement.
9. Important to monitor for subclinical disease recurrence with inflammatory markers even if the patient is asymptomatic.
