PANCE - Ischemic Heart Disease Symptoms and Treatments
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Ischemic Heart Disease Symptoms and Treatments tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for PANCE.
Below is information not explicitly contained within the tutorial but important for PANCE.
- --
VITAL FOR PANCE
Ischemic Heart Disease Fundamentals
1. Angina pectoris is the hallmark of ischemic heart disease, characterized by pain or discomfort in the chest, which often radiates through the upper extremities, face, and other areas of the body, and is due to the heart's inability to meet its metabolic needs.
2. Stable angina is characterized by predictable triggers, duration, and frequency; triggered by physical or mental exertion and resolves with rest and/or nitrates.
3. Unstable angina is unpredictable, does not resolve with rest or medications, and is a medical emergency that can lead to myocardial infarction.
4. Non-ischemic causes of angina include aortic stenosis, anemia, arrhythmias, and hypertrophic cardiomyopathy.
5. Silent ischemia refers to asymptomatic ischemic heart disease; "silent" does not mean "harmless" and is associated with increased morbidity and mortality.
Angina Classification
1. Stable angina (effort angina): triggered by physical or mental exertion such as climbing stairs or psychological stress; resolves with rest and/or nitrates.
2. Unstable angina: new onset or worsening angina that is unpredictable; occurs spontaneously during activity or rest, and does not resolve with rest or medications; a form of acute coronary syndrome.
3. Vasospastic angina (variant/Prinzmetal angina): occurs when vasospasm contracts vessels and reduces blood flow; occurs spontaneously and often at rest, typically at night or early morning; most common in women and cigarette smokers.
4. Microvascular angina: result of coronary microvascular dysfunction or vasospasm; accounts for chest pain in up to half of patients without obstructive coronary artery disease; occurs with exertion and at rest but may respond less well to nitrates.
- --
HIGH YIELD
Clinical Presentation
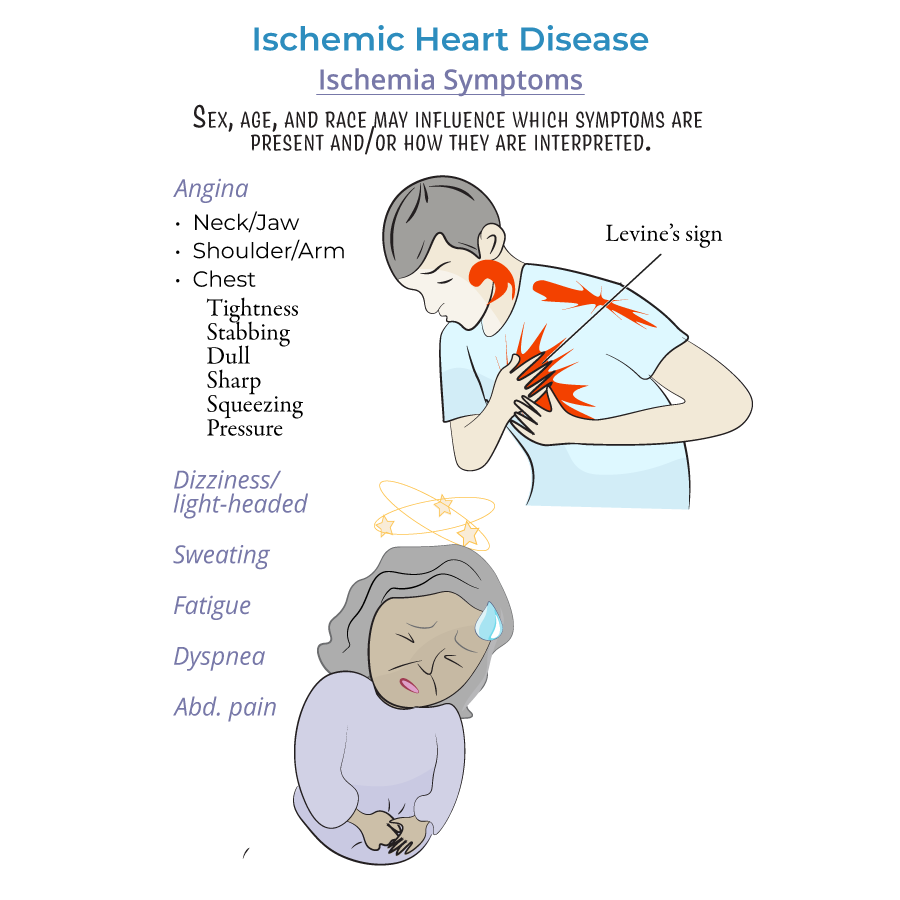
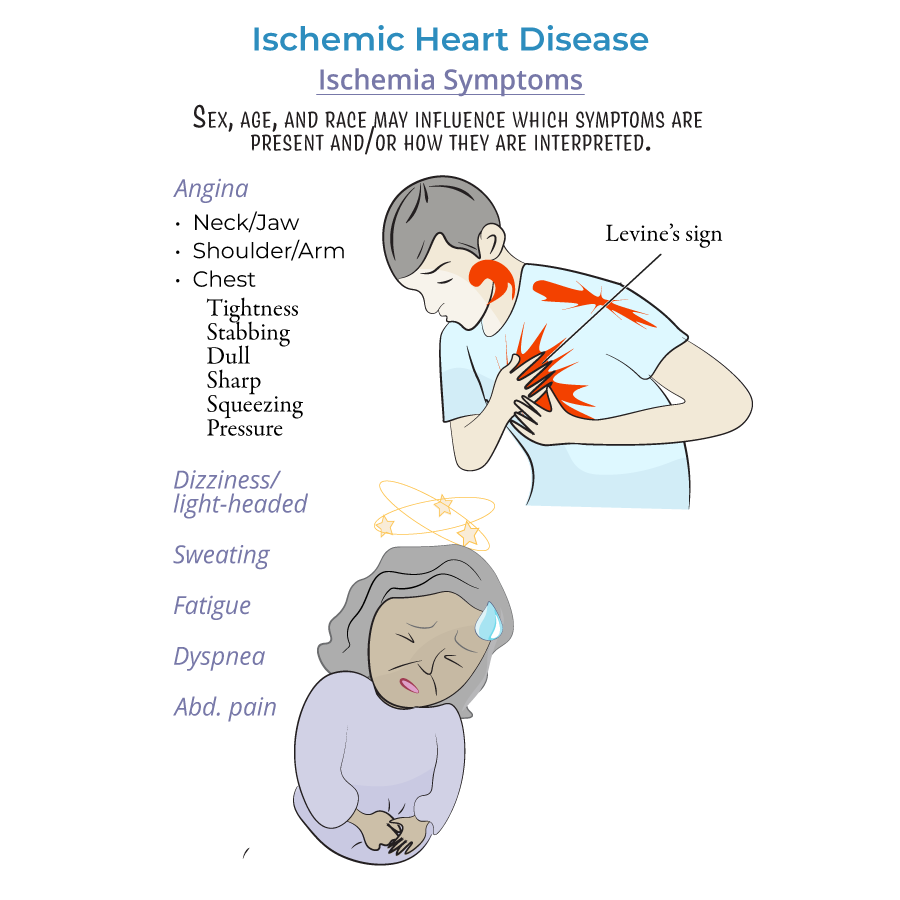
1. Sex, age, and race may influence which symptoms are present and how they are interpreted.
2. Angina presents as chest discomfort or pain, variably described as: tightness, dull, sharp, or stabbing pain, squeezing, or pressure on the heart.
3. Levine's sign, a clenched fist held over the sternum, is a gesture many patients use to describe chest discomfort.
4. Patients report discomfort radiating to the shoulders, arms, neck, and jaw.
5. Patients of African descent often experience gastrointestinal discomfort that may be misinterpreted as indigestion or heartburn.
6. Women with ischemic heart disease frequently experience light-headedness, dizziness, and persistent fatigue.
7. Other common symptoms include dyspnea (difficulty breathing) and excessive sweating.
Diagnostic Approach
1. Diagnosis of ischemic heart disease may involve ECG, echocardiogram, stress testing, angiograms, and CT scans.
2. Although angina is often due to obstructive coronary artery disease, it can also occur in absence of clinically significant blockage.
3. Microvascular angina can be difficult to distinguish from epicardial angina; positron emission tomography (PET) or cardiac magnetic resonance (CMR) can assess coronary microvascular blood flow.
Management Strategies
1. Life-style modifications such as smoking cessation and a heart-healthy diet are generally recommended.
2. Nitroglycerin, often administered as a sublingual tablet, dilates vessels and prevents spasms; can be taken prophylactically or in response to an angina episode.
3. Beta-blockers slow the heart rate, reducing myocardial oxygen demands; can exacerbate vasospastic angina.
4. Calcium channel blockers promote vessel dilation; effective for vasospastic angina.
5. Sodium channel inhibitors (Ranolazine) increase myocardial relaxation, reducing oxygen demand and increasing blood flow.
6. ACE-inhibitors promote vessel dilation.
7. Statins reduce hyperlipidemia, vessel inflammation, and endothelial dysfunction.
8. Daily aspirin may be prescribed, but benefits must be weighed against the risk of bleeding.
9. Percutaneous coronary intervention (angioplasty) is performed using a catheter with balloon to widen obstructed vessels; a stent may be added to keep the vessel open.
10. Coronary artery bypass grafting (CABG) involves grafting another vessel (saphenous vein, radial artery, or left internal mammary artery) to bypass an obstruction.
11. Refractory angina refers to ischemia with angina that persists despite medical intervention; innovative treatments for these "no-option" patients are eagerly sought.
- --
Beyond the Tutorial
Advanced Assessment
1. Pre-test probability assessment using Diamond-Forrester criteria or ASCVD risk calculator guides diagnostic workup.
2. HEART score aids in risk stratification for patients presenting with chest pain.
3. Troponin trends are more valuable than single values in diagnosing ACS.
4. Biomarker patterns can distinguish between type 1 and type 2 myocardial infarction.
Pharmacotherapy Considerations
1. P2Y12 inhibitor selection (clopidogrel, ticagrelor, prasugrel) depends on patient factors and clinical context.
2. DAPT duration protocols vary based on stent type, clinical indication, and bleeding risk.
3. Proton pump inhibitors should be considered for patients on dual antiplatelet therapy with high bleeding risk.
4. SGLT2 inhibitors and GLP-1 receptor agonists provide cardiovascular benefit in patients with diabetes and established CAD.
