PANCE - Ischemic Heart Disease Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE (Physician Assistant National Certifying Examination) from the Ischemic Heart Disease tutorial, focusing on clinical assessment, diagnosis, and management considerations, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards.
 1. Obstructive coronary artery disease: Atherosclerotic plaques obstructing ≥50% of epicardial artery lumen.
2. INOCA (Ischemia with No Obstructive Coronary Artery Disease): Plaques <50% obstruction.
3. Plaque complications: Rupture or erosion of plaques leading to thrombus formation.
4. Coronary microvascular dysfunction: Structural and/or functional impairment of the coronary microvasculature.
5. Vasospasm: Abnormal vasoconstriction of coronary vessels.
1. Obstructive coronary artery disease: Atherosclerotic plaques obstructing ≥50% of epicardial artery lumen.
2. INOCA (Ischemia with No Obstructive Coronary Artery Disease): Plaques <50% obstruction.
3. Plaque complications: Rupture or erosion of plaques leading to thrombus formation.
4. Coronary microvascular dysfunction: Structural and/or functional impairment of the coronary microvasculature.
5. Vasospasm: Abnormal vasoconstriction of coronary vessels.
 Below is additional information important for PANCE not explicitly contained within the tutorial.
Below is additional information important for PANCE not explicitly contained within the tutorial.
- --
VITAL FOR PANCE
Cardiac Ischemia: Clinical Framework
1. Definition: Cardiac ischemia occurs when coronary blood flow is insufficient to meet myocardial metabolic needs.
2. Consequences: Impaired mechanical and/or electrical cardiac function.
3. Clinical significance: Leading cause of death in both men and women.
4. Acute coronary syndrome (ACS): Umbrella term for events from sudden cardiac ischemia (unstable angina, MI, sudden cardiac death).
Risk Factor Assessment and Stratification
1. Traditional factors: Family history, age, smoking, hypertension, diabetes, hyperlipidemia, obesity, low physical activity.
2. Sex-specific factors: Early menopause, gestational diabetes and hypertension.
3. Additional considerations: Chronic inflammatory rheumatoid diseases.
4. Clinical pearl: Risk factors may have stronger impacts in women than men.
Comprehensive Diagnostic Approach
1. Key clinical insight: Up to 50% of patients with suspected ischemia have no significant coronary obstruction on angiogram.
2. Diagnostic implications: Normal angiogram does not exclude ischemic heart disease.
3. Clinical patterns to recognize:
- Obstructive CAD (≥50% stenosis): More common in men >45, women >55
- INOCA (<50% stenosis): More common in women, present in ~30% of men
- Clinical significance: INOCA associated with elevated MACE risk, especially in younger women
Differential Diagnosis of Ischemic Patterns
 1. Obstructive coronary artery disease: Atherosclerotic plaques obstructing ≥50% of epicardial artery lumen.
2. INOCA (Ischemia with No Obstructive Coronary Artery Disease): Plaques <50% obstruction.
3. Plaque complications: Rupture or erosion of plaques leading to thrombus formation.
4. Coronary microvascular dysfunction: Structural and/or functional impairment of the coronary microvasculature.
5. Vasospasm: Abnormal vasoconstriction of coronary vessels.
1. Obstructive coronary artery disease: Atherosclerotic plaques obstructing ≥50% of epicardial artery lumen.
2. INOCA (Ischemia with No Obstructive Coronary Artery Disease): Plaques <50% obstruction.
3. Plaque complications: Rupture or erosion of plaques leading to thrombus formation.
4. Coronary microvascular dysfunction: Structural and/or functional impairment of the coronary microvasculature.
5. Vasospasm: Abnormal vasoconstriction of coronary vessels.
- --
HIGH YIELD
Coronary Blood Supply Considerations
1. Epicardial coronary arteries: Surface vessels (left and right coronary arteries and branches).
2. Coronary microvasculature: Deeper vessels (prearterioles, arterioles, capillaries).
3. Functional role: Prearterioles and arterioles provide resistance and regulation of blood flow.
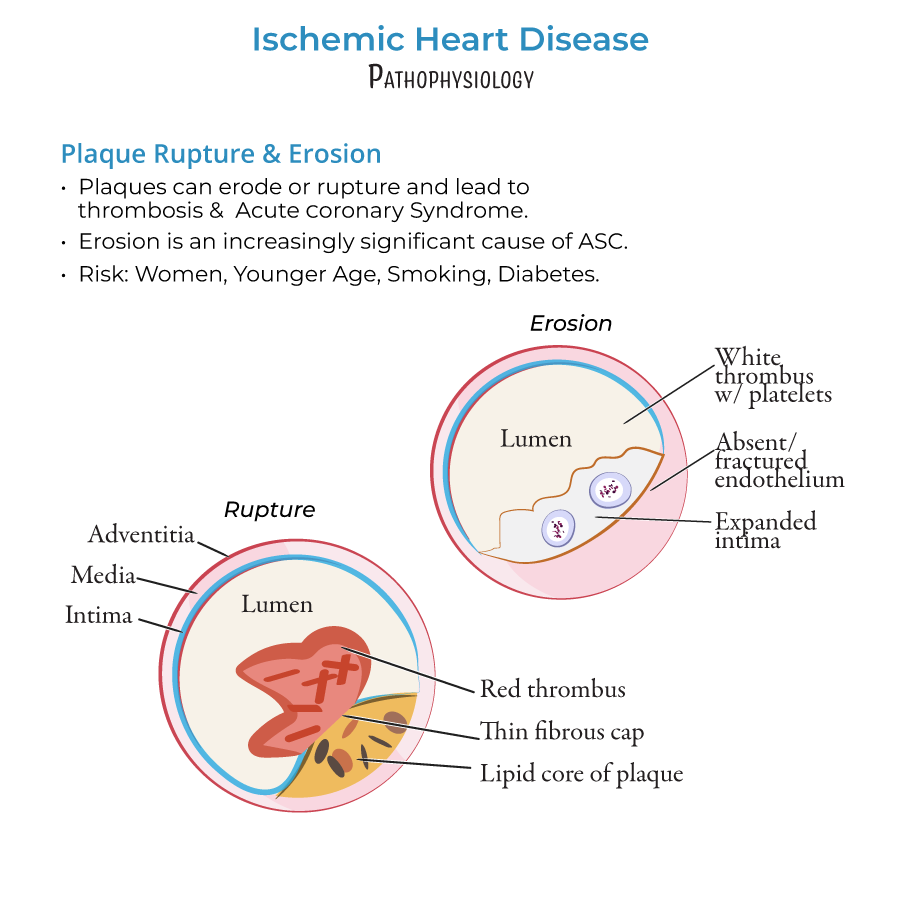
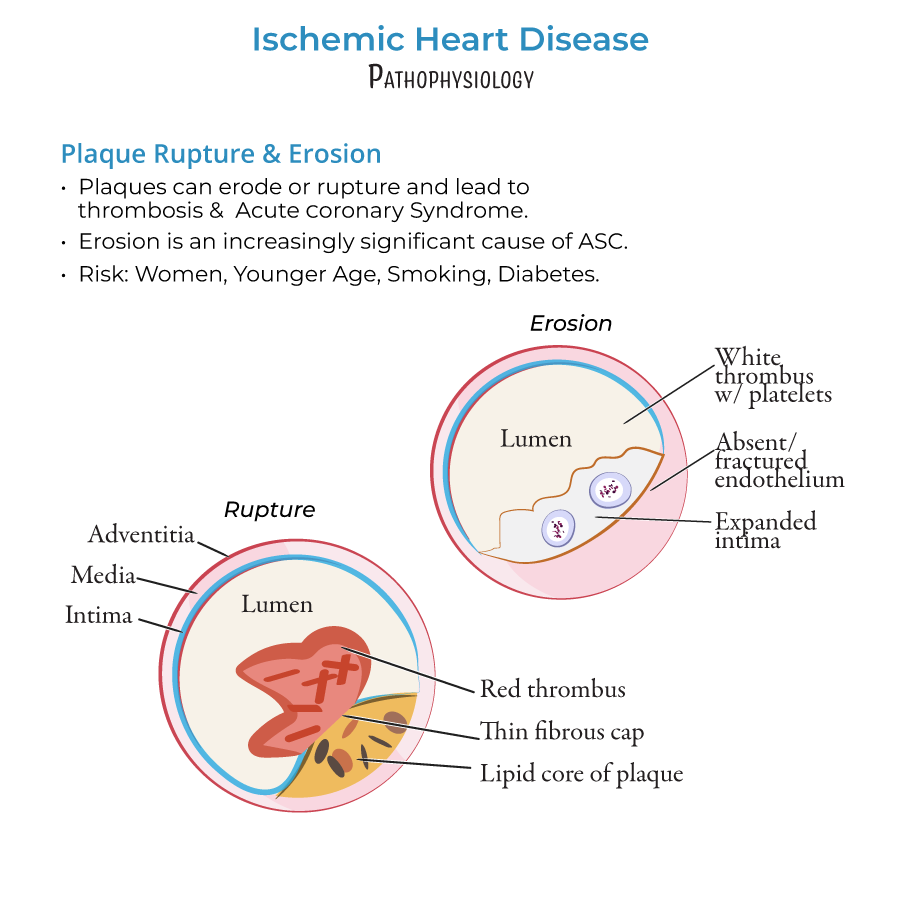
Plaque Complications: Clinical Differentiation
1. Plaque rupture:
- Characteristics: Lipid cores, thin caps, tears in fibrous caps
- Thrombogenic profile: Forms fibrin-rich "red thrombi"
- Therapeutic note: Decreasing in frequency due to statin therapy
- Patient demographics: More common in women, young patients, smokers, diabetics
- Pathophysiology: Thick cap plaques with endothelial dysfunction/absence
- Thrombogenic profile: Produces platelet-rich "white thrombi"
- Therapeutic challenge: Not prevented by lipid-lowering therapy alone
Coronary Microvascular Dysfunction
1. Epidemiology: Affects both sexes nearly equally (contrary to earlier beliefs).
2. Clinical relevance: Significant cause of INOCA, can coexist with obstructive CAD.
3. Pathophysiologic mechanisms:
- Structural: Arteriole remodeling (thicker walls, reduced wall:lumen ratio)
- Functional: Impaired vasodilation, endothelial dysfunction
- Pattern: Diffuse, patchy ischemia (vs. localized epicardial lesions)
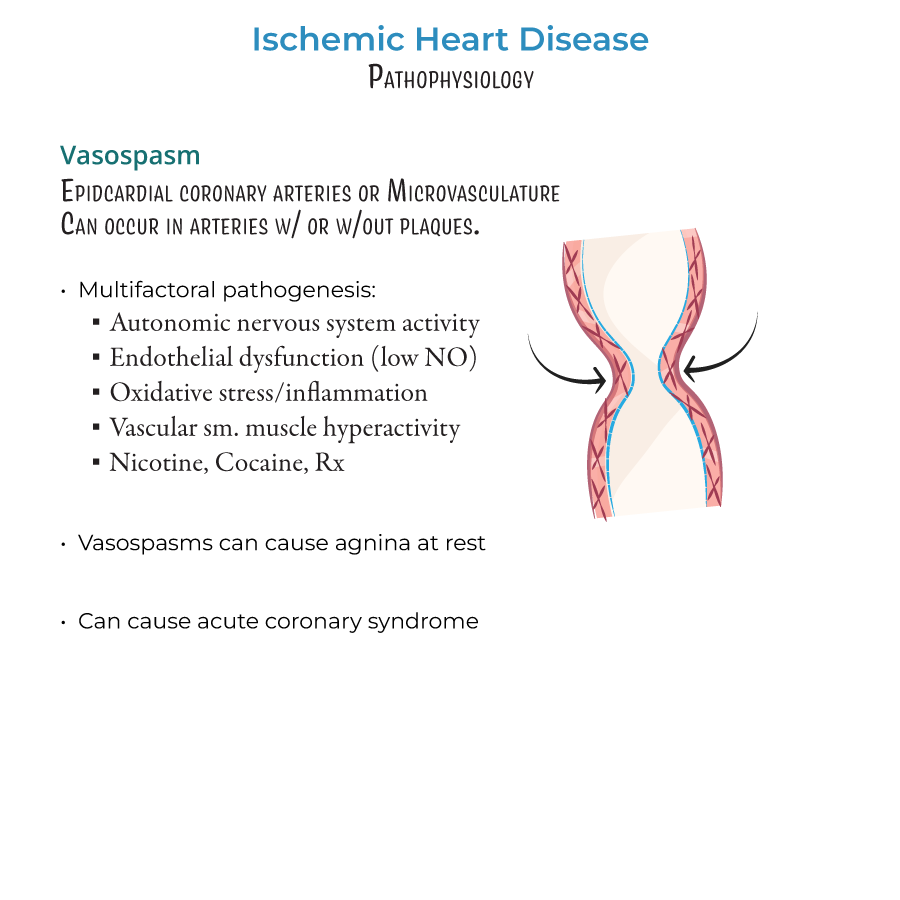
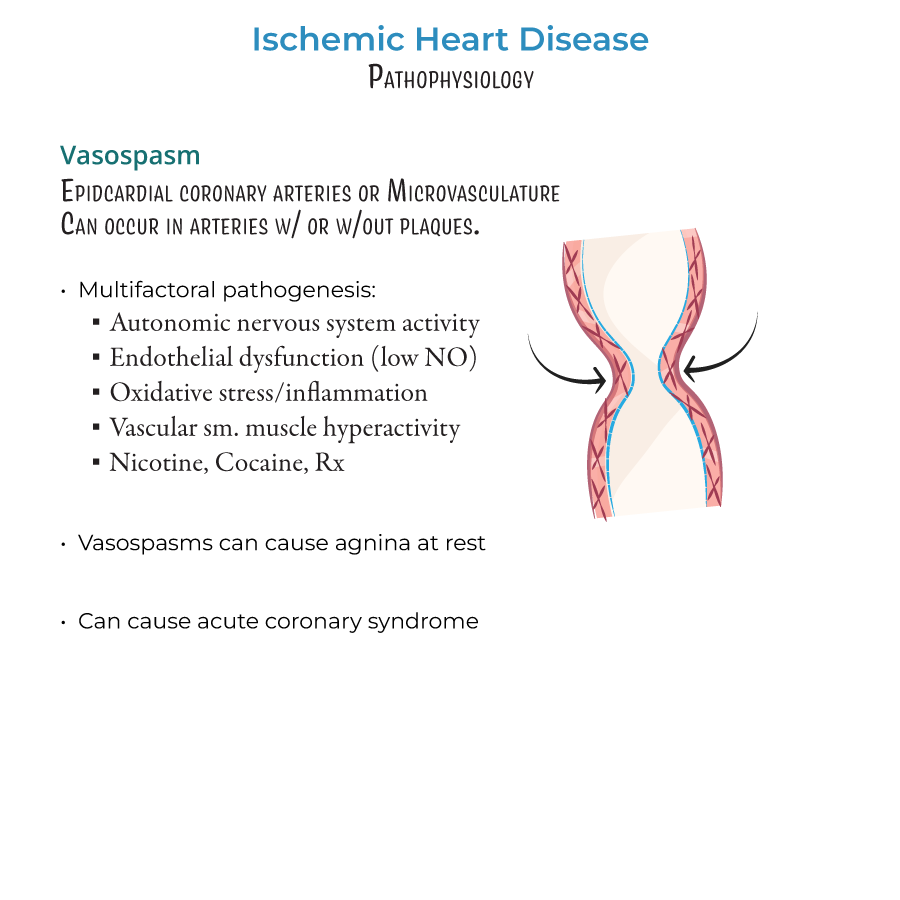
Vasospasm: Diagnostic Considerations
1. Location: Can occur in epicardial coronary arteries and microvasculature.
2. Context: Can happen with or without underlying stenosis.
3. Precipitating factors:
- Enhanced autonomic nervous system activity
- Endothelial dysfunction (especially reduced nitric oxide)
- Oxidative stress and inflammation
- Vascular smooth muscle hyperactivity
- Exogenous triggers: nicotine, cocaine, vasoconstricting medications
Clinical Assessment Pearls
1. Sex-based differences:
- Women: Higher prevalence of INOCA and plaque erosion
- Men: Higher prevalence of obstructive CAD
- Both: Similar rates of microvascular dysfunction
- Exertional symptoms: Consider obstructive CAD
- Rest symptoms: Consider vasospasm
- Symptoms with normal angiogram: Consider microvascular dysfunction, INOCA
- --
Beyond the Tutorial
Clinical Presentation and Evaluation
1. History and physical exam:
- Chest pain characteristics (PQRST assessment)
- Associated symptoms (dyspnea, diaphoresis, nausea, radiation to arm/jaw)
- Timing of symptoms (rest vs. exertion)
- Cardiovascular examination (rate, rhythm, murmurs, gallops)
- Signs of heart failure (JVD, edema, crackles)
- ECG patterns:
- ST elevation: Transmural ischemia/infarction
- ST depression: Subendocardial ischemia
- T-wave inversion: Ischemia
- Q waves: Prior infarction
- Cardiac biomarkers: Troponin I/T, CK-MB
- Non-invasive testing: Stress testing (exercise, pharmacologic), stress echo, nuclear imaging
- Invasive testing: Coronary angiography, fractional flow reserve (FFR)
Management Approaches
1. Acute interventions for ACS:
- Initial management: Aspirin, nitroglycerin, oxygen if hypoxemic
- Antiplatelet therapy: DAPT (aspirin + P2Y12 inhibitor)
- Anticoagulation: UFH, LMWH, fondaparinux
- Reperfusion strategies: Primary PCI vs. fibrinolysis
- Adjunctive therapies: Beta-blockers, ACE inhibitors, statins
- Anti-anginal medications:
- First-line: Beta-blockers, CCBs, nitrates
- Second-line: Ranolazine, ivabradine
- Risk factor modification:
- Lipid management: High-intensity statins, ezetimibe, PCSK9 inhibitors
- Hypertension control: Goal BP <130/80 mmHg
- Diabetes management: Target HbA1c <7%
- Antiplatelet therapy: Aspirin 81 mg daily
- Revascularization considerations: PCI vs. CABG based on anatomy
- Vasospastic angina: CCBs and nitrates are first-line; avoid beta-blockers
- Microvascular angina: Beta-blockers, CCBs, ACE inhibitors, ranolazine
- Plaque erosion management: Aggressive antiplatelet therapy
- INOCA: Consider coronary reactivity testing, targeted therapy
PA Clinical Role and Monitoring
1. Patient education:
- Risk factor modification strategies
- Medication adherence
- Warning symptoms requiring immediate medical attention
- Cardiac rehabilitation importance
- Medication efficacy and side effect assessment
- Symptom evaluation
- Risk factor control
- Exercise tolerance monitoring
- Secondary prevention measures
- New or worsening chest pain despite medical therapy
- Syncope or presyncope with exertion
- Symptoms at progressively lower levels of activity
- New heart failure symptoms
- Medication intolerance affecting adherence
