PANCE - Inflammatory Bowel Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Inflammatory Bowel Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR PANCE
Inflammatory Bowel Disease (IBD) Overview
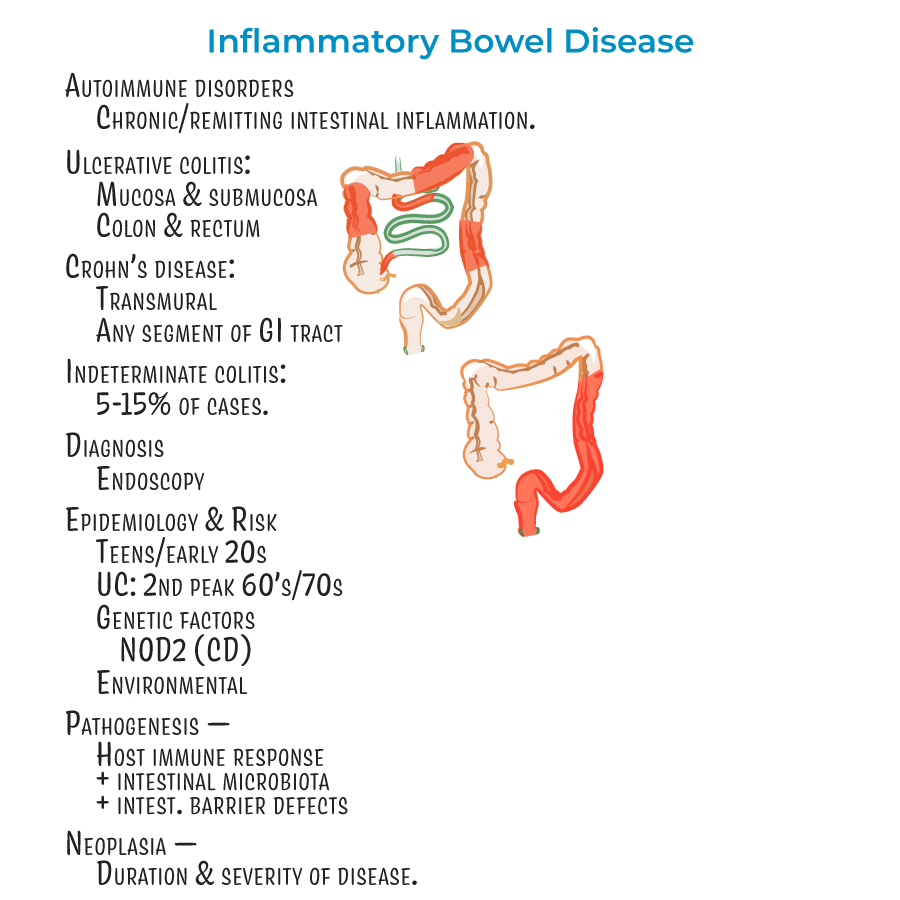
1. Autoimmune disorders characterized by chronic or remitting intestinal inflammation.
2. Diagnosis relies on endoscopy.
3. Most patients diagnosed in teens/early 20s; ulcerative colitis has a second "peak" in patients in their 60's or 70's.
4. Genetic factors play a role (e.g., mutations in NOD2 associated with Crohn's disease).
5. Result of detrimental interactions between host immune response, intestinal microbiota, and intestinal barrier defects.
6. Associated with neoplasia, influenced by duration and severity of disease.
Crohn's Disease - Clinical Features
1. Transmural inflammation can reach all layers of GI tract.
2. Can affect any segment of GI tract, but most commonly involves ileum and colon.
3. "Skip lesions" - discontinuous pattern with normal areas between affected segments.
4. Rectum usually spared (unlike ulcerative colitis).
5. Clinical presentation: Abdominal cramping (often on the right side, where the ileum meets the large intestine), diarrhea (potentially bloody), fever and malaise, weight loss (due to malabsorption), perianal lesions (25% of patients).
6. Complications: Problems related to fistulas, fissures, and obstructive strictures; dysplasia and adenocarcinoma; and anemia from chronic blood loss.
Ulcerative Colitis - Clinical Features
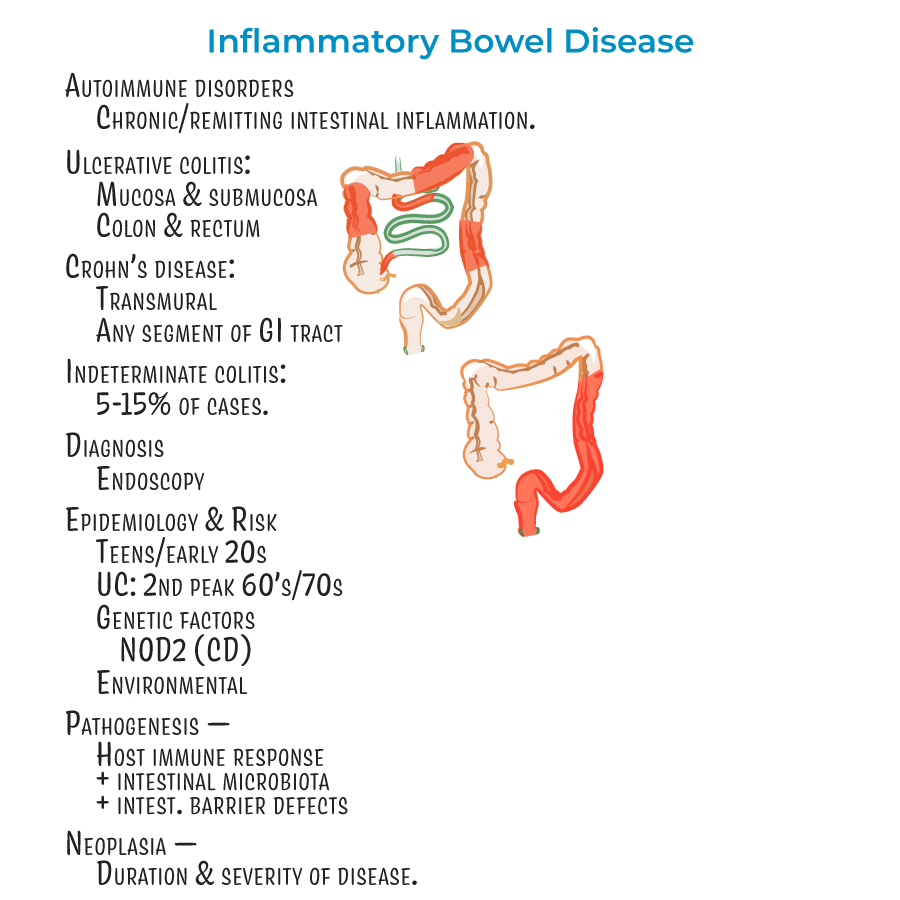
1. Mucosal and submucosal inflammation only.
2. Restricted to the colon and rectum.
3. Characterized by continuous lesions (unlike Crohn's disease).
4. Clinical presentation: Bloody diarrhea with rectal bleeding, abdominal pain, fever, and weight loss.
5. Complications: Toxic ulceritis, toxic megacolon, intestinal perforation. Dysplasia and adenocarcinoma more likely when entire colon is involved (pancolitis).
- --
HIGH YIELD
Inflammatory Bowel Disease - Management
1. Environmental factors are important (diet, cigarette smoking, medications).
2. About 5-15% of cases are considered "indeterminant" colitis when distinction between UC and CD is difficult.
3. Extraintestinal manifestations: Most common are skin lesions (in up to 40% of patients), uveitis, and arthritis.
4. Less common but potentially deadly complications: involvement of liver/gallbladder, lung, pancreas, and kidneys.
Crohn's Disease - Diagnostic Features
1. Many studies suggest a female predominance.
2. Transmural inflammation with wall thickening and "creeping fat" that wraps around the GI tract.
3. Lesion progression:
- Aphthous erosions (early shallow whitish sores)
- Longitudinal "bear claw" ulcers (look like rake dragged down GI lining)
- Cobblestone appearance (as tissue becomes crowded with ulcers)
- Fissures form and progress to fistulas (connecting to abdominal/pelvic cavity or other organs)
Ulcerative Colitis - Diagnostic Features
1. Sunken, red/bloody ulcers with friable appearance.
2. Inflammation destroys submucosal vascular network.
3. Mucosa is bloody during active inflammation.
4. Remaining mucosa creates "pseudopolyps".
5. Histology: Branching and distension of intestinal crypts, crypt abscesses with neutrophils.
6. Inflammation is Th2 cell-mediated.
Treatment Approaches
1. Crohn's disease: Patients advised to avoid cigarette smoking (exacerbates inflammation), anti-inflammatories, immune suppressors, surgery to remove parts of the colon.
2. Ulcerative colitis: Anti-inflammatories, immune suppressors, and colectomy. Patients who smoke cigarettes more likely to experience bouts upon quitting.
Differential Diagnosis
1. Key differences:
- CD = transmural inflammation, skip lesions, any GI segment, rectum usually spared
- UC = mucosal/submucosal inflammation, continuous lesions, colon/rectum only
- --
Beyond the Tutorial
Initial Evaluation and Workup
1. History taking:
- Detailed symptom characterization (onset, duration, frequency)
- Family history of IBD or colorectal cancer
- Medication history (NSAIDs, antibiotics)
- Travel history (infectious differential)
- Smoking status
- Diet and recent dietary changes
- Comprehensive abdominal exam (tenderness, masses, distention)
- Digital rectal examination
- Perianal inspection
- Oral cavity assessment for ulcers
- Skin, joint, and eye examination for extraintestinal manifestations
- Nutritional status evaluation
- CBC with differential
- CMP with liver function
- ESR and CRP
- Fecal calprotectin
- Stool studies (culture, ova and parasites, C. difficile)
- Iron studies
- Vitamin B12, folate, and vitamin D levels
- Abdominal radiography (for obstruction, toxic megacolon)
- CT enterography
- MR enterography (preferred for young patients)
- Small bowel follow-through
- Capsule endoscopy (contraindicated with strictures)
Management in Primary Care Setting
1. Medication management:
- 5-ASA compounds (mesalamine, sulfasalazine): indications, dosing, adverse effects
- Corticosteroids: appropriate duration, tapering schedules, monitoring
- Immunomodulators: required laboratory monitoring, vaccination considerations
- Biologics: screening requirements, timing of laboratory monitoring
- Antibiotics: specific indications in IBD
- Laboratory monitoring based on medication regimen
- Nutritional status assessment
- Growth and development in pediatric patients
- Bone health with long-term steroid use
- Cancer surveillance protocols
- Vaccination guidelines for immunosuppressed patients
- Pneumococcal, influenza, hepatitis B, HPV vaccinations
- TB screening before biologic therapy
- Bone density testing
- Depression and anxiety screening
- Criteria for hospital admission
- Recognition of toxic megacolon
- Management of acute severe flares
- Dehydration assessment and management
- Pain management approaches
Patient Education and Counseling
1. Disease education:
- Chronic nature of IBD
- Importance of medication adherence even during remission
- Warning signs requiring urgent medical attention
- Proper use of symptom diary
- Smoking cessation strategies (with UC vs. CD considerations)
- Stress management techniques
- Exercise recommendations
- Travel planning with IBD
- Occupational considerations
- Common food triggers
- Appropriate diet during flares vs. remission
- Importance of adequate hydration
- Supplement recommendations
- When to consult dietitian
- Fertility implications
- Medication safety during pregnancy and breastfeeding
- Disease management during pregnancy
- Genetic counseling considerations
Interprofessional Collaboration
1. Referral guidelines:
- When to refer to gastroenterology
- Surgical consultation criteria
- Nutritional support team involvement
- Pain management specialist referral
- Mental health referrals
- Communication with specialists
- Documentation requirements
- Insurance authorization for biologics
- Home health services when appropriate
- Support group resources
- Creating emergency care plans
- Patient education on emergency department visits
- Documentation of treatment history for emergency providers
- Steroid dosing during acute illness
- Pediatric to adult care transition
- Hospital to home coordination
- Post-surgical follow-up protocols
- Communication across healthcare settings
