PANCE - Hypertension Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE (Physician Assistant National Certifying Examination) & PANRE from the Blood Pressure Regulation and Hypertension tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 4. Determinants of peripheral resistance:
Below is information not explicitly contained within the tutorial but important for PANCE & PANRE.
4. Determinants of peripheral resistance:
Below is information not explicitly contained within the tutorial but important for PANCE & PANRE.
- --
VITAL FOR PANCE/PANRE
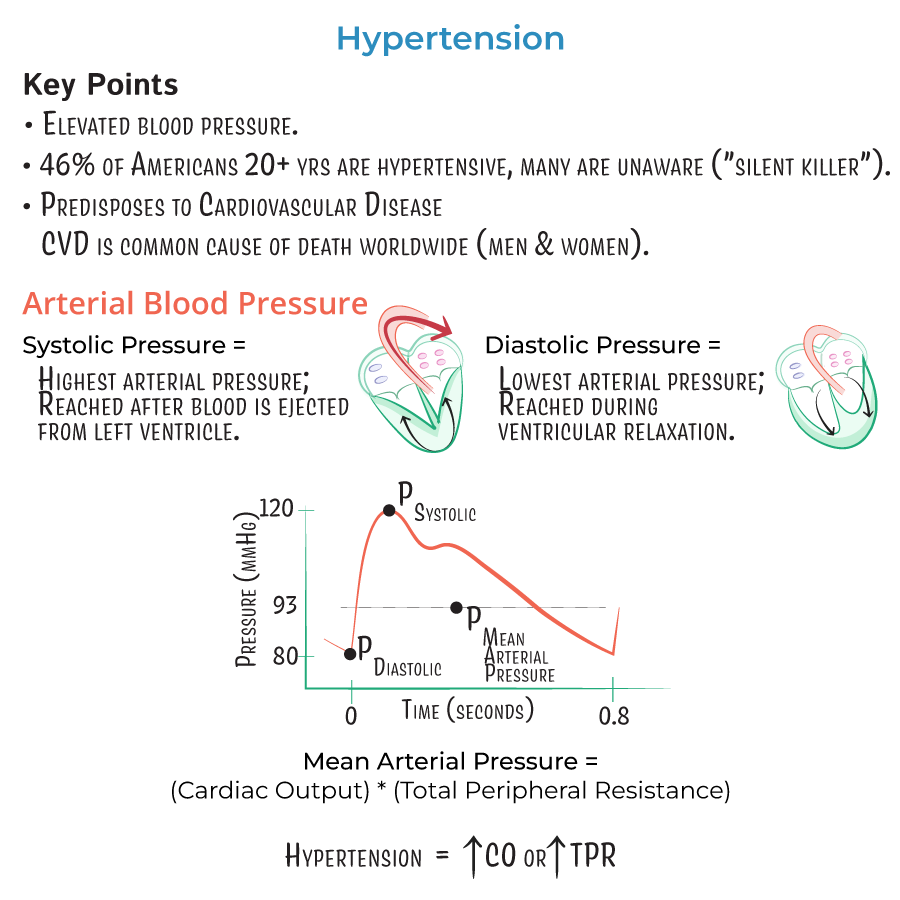
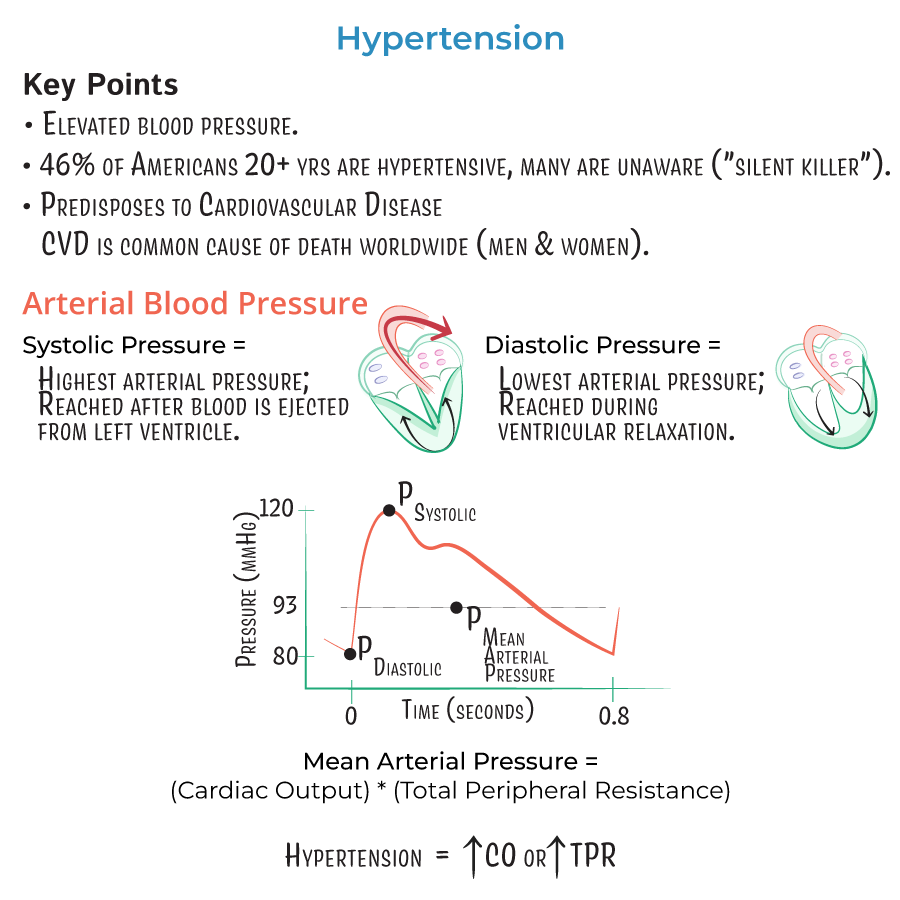
Blood Pressure Fundamentals
1. Determinants of mean arterial pressure:
- Cardiac output (CO)
- Total peripheral resistance (TPR)
- Formula: MAP = CO × TPR
- Heart rate
- Stroke volume
- Formula: CO = HR × SV
- Preload: affected by blood volume and venous return
- Contractility: intrinsic force of contraction
- Afterload: resistance against which heart pumps
 4. Determinants of peripheral resistance:
4. Determinants of peripheral resistance:
- Vasoconstriction of small arteries and arterioles
- Anatomic changes in vessel walls (remodeling)
- Blood viscosity (minor component)
Physiologic Mediators of Blood Pressure
1. Renin-Angiotensin-Aldosterone System:
- Angiotensin II: potent vasoconstrictor
- Increases sodium and water retention
- Stimulates release of norepinephrine, ADH, and aldosterone
- Target for multiple antihypertensive medications
- Antidiuretic hormone (vasopressin)
- Functions as vasoconstrictor
- Increases water reabsorption in collecting ducts
- Aldosterone
- Increases sodium and water retention
- Effects similar to ADH on blood volume
- Norepinephrine
- Increases heart rate and contractility
- Causes vasoconstriction
Hypertensive Crisis Evaluation
1. Classification:
- Hypertensive urgency: BP >180/120 mmHg without end-organ damage
- Hypertensive emergency: BP >180/120 mmHg with end-organ damage
- Severe headache with confusion
- Impaired vision
- Chest pain, shortness of breath
- Nausea/vomiting
- Anxiety
- Seizures
- --
HIGH YIELD
Clinical Understanding of BP Regulation
1. Vasoactive balance:
- Vasodilators: nitric oxide, prostaglandins, histamine, bradykinin
- Vasoconstrictors: angiotensin II, norepinephrine, endothelin
- Clinical relevance: medications target this balance
- Angiotensin II breaks down bradykinin (vasodilator)
- ACE inhibitors both reduce angiotensin II and increase bradykinin
- Explains therapeutic effects and side effect profile
- Hypertension produces vessel damage and inflammation
- Results in elevated endothelin (vasoconstrictor)
- Reduces nitric oxide (vasodilator)
- Impact: chronic hypertension becomes more resistant to treatment
Pathophysiologic Assessment
1. Volume-dependent hypertension:
- Salt-sensitive patients develop hypertension with high sodium intake
- Clinical clues: edema, response to diuretics
- Therapeutic approach: sodium restriction, diuretics
- Aldosterone-secreting tumors increase blood volume and preload
- Clinical clues: hypokalemia, metabolic alkalosis
- Diagnostic approach: aldosterone/renin ratio
- Genetic and epigenetic factors
- Diet (especially sodium)
- Physical activity levels
- Environmental factors
- --
Beyond the Tutorial
Diagnosis and Classification
1. BP measurement technique:
- Proper cuff size and positioning
- Patient positioning and preparation
- Multiple readings on separate occasions
- Ambulatory and home BP monitoring
- Normal: <120/<80 mmHg
- Elevated: 120-129/<80 mmHg
- Stage 1: 130-139/80-89 mmHg
- Stage 2: ≥140/≥90 mmHg
- Hypertensive crisis: >180/>120 mmHg
- Clinical clues suggesting secondary causes
- Initial diagnostic workup
- When to refer for specialist evaluation
Management Approach
1. Non-pharmacologic interventions:
- DASH diet
- Sodium restriction (<2.3g/day)
- Regular physical activity
- Weight loss
- Alcohol limitation
- Smoking cessation
- First-line agents: thiazides, ACEIs, ARBs, CCBs
- Second-line agents: beta-blockers, alpha-blockers, aldosterone antagonists
- Combination therapy principles
- Monitoring parameters
- Elderly
- Pregnancy
- Diabetes
- CKD
- CVD
- African American patients
Complications and Follow-up
1. Target organ damage:
- Heart: LVH, heart failure, CAD
- Brain: stroke, TIA, vascular dementia
- Kidneys: CKD, proteinuria
- Vessels: aortic aneurysm, PAD
- Eyes: retinopathy
- Medication adherence strategies
- Self-monitoring guidance
- Warning signs requiring medical attention
- Lifestyle modification counseling
- Monitoring frequency based on control and risk
- Laboratory monitoring
- Reassessment of cardiovascular risk
- Medication adjustment approach
