PANCE - GI Bleeding
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the GI Bleeding tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR PANCE
Clinical Presentations of GI Bleeding
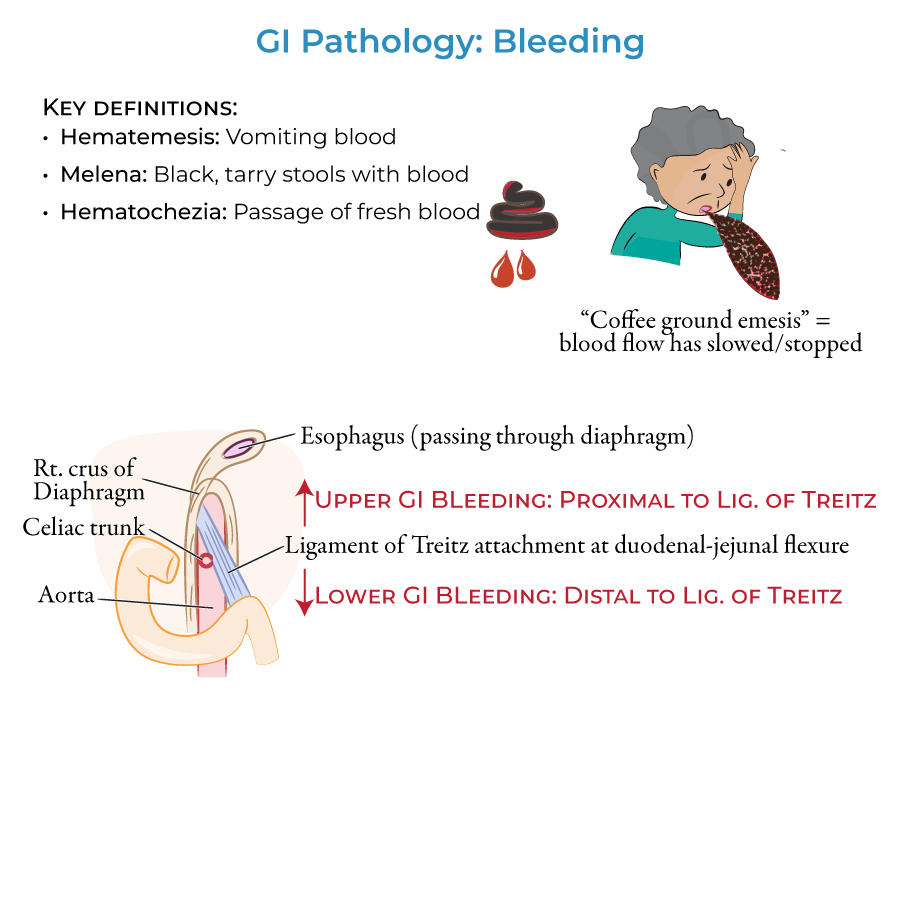
1. Hematemesis means vomiting blood ("heme" = blood; "emesis" = vomit).
2. When bloody vomit has a dark, mottled "coffee ground" appearance, this indicates that blood flow has slowed or stopped.
3. Melena refers to black, tarry stools with blood.
4. Hematochezia refers to the passage of bright red fresh blood.
5. Bleeding in the upper gastrointestinal tract produces hematemesis and/or melena; bleeding in the lower gastrointestinal tract produces melena or hematochezia.
Anatomical Considerations
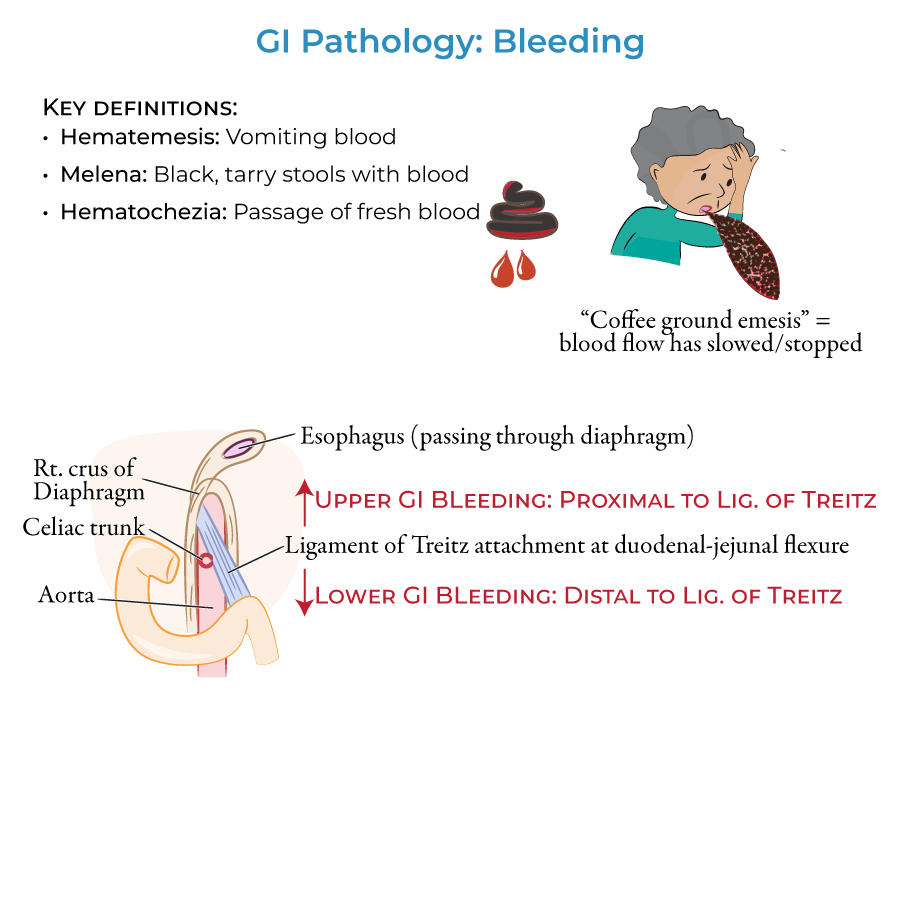
1. The Upper Gastrointestinal tract lies proximal to the duodenal attachment of the ligament of Treitz (suspensory ligament of the duodenum) and the Lower Gastrointestinal tract lies distal to it.
Upper GI Bleeding Etiologies
1. Duodenal and gastric ulcers & erosion are most common cause of upper GI bleeding, resulting from H. pylori infection, drugs, stress, or autoimmune disorders.
2. Esophagitis leads to erosion of the esophageal lining and bleeding, associated with severe acid reflux and alcohol consumption.
3. Varices in the esophagus and proximal stomach can rupture and cause potentially life-threatening hemorrhages, associated with cirrhosis and portal hypertension.
4. Mallory-Weiss tears occur in the distal esophagus from fits of violent vomiting or coughing.
Lower GI Bleeding Etiologies
1. Infectious colitis, particularly bacterial, produces fever, tenesmus, abdominal pain, and purulent, loose bloody stools.
2. C. difficile infection following antibiotic use is an example of bacterial colitis.
3. Inflammatory bowel disease, particularly ulcerative colitis, causes bloody diarrhea when active.
4. Acute and chronic intestinal ischemia causes lower GI bleeding along with nausea, vomiting, and abdominal pain.
5. Diverticular hemorrhage is a top cause of lower GI bleeding characterized by brisk hematochezia with possibility of massive bleeding.
6. Anal fissures are tears in the anal sphincter that produce bright, fresh blood and cause pain during and after bowel movements.
7. Hemorrhoids are swollen veins in rectum and perianal region that can rupture and produce hematochezia.
- --
HIGH YIELD
Clinical Distinctions
1. Viral colitis is associated with watery diarrhea and is more common in infants and children.
2. Amoebic colitis is associated with diarrhea and mucoid discharge.
3. Ulcerative colitis is characterized by mucosal and submucosal inflammation with sunken ulcers that create a friable or crumbly appearance.
4. Diverticula are not necessarily inflamed when bleeding occurs in diverticular hemorrhage.
5. Mallory-Weiss tears are rare compared to other causes of upper GI bleeding.
Important Distinguishing Features
1. Esophagitis erosion is most often associated with severe acid reflux and alcohol consumption.
2. Varices can cause potentially life-threatening hemorrhages.
3. Neoplasms can occur anywhere along the GI tract and are often the presenting sign.
4. Arteriovenous malformations are atypical arrangements of blood vessels that divert blood from their proper targets; the tangled vessels can rupture and cause bleeding. These are rare.
- --
Beyond the Tutorial
Diagnostic Approach
1. History and physical exam should focus on hemodynamic stability, comorbidities, and medication history.
2. Laboratory evaluation includes CBC, coagulation studies, liver function tests, and BUN/creatinine ratio.
3. Nasogastric lavage may help localize bleeding to upper versus lower GI tract.
4. Upper endoscopy is first-line for suspected upper GI bleeding.
5. Colonoscopy is preferred for evaluation of lower GI bleeding after bowel preparation.
Treatment Principles
1. Initial resuscitation with IV fluids and blood products based on hemodynamic status and hemoglobin levels.
2. Proton pump inhibitors for non-variceal upper GI bleeding.
3. Octreotide and antibiotics for variceal bleeding.
4. Endoscopic interventions including injection therapy, thermal coagulation, and mechanical methods.
5. Interventional radiology with embolization for refractory bleeding.
Special Considerations
1. Management of anticoagulation and antiplatelet therapy in patients with GI bleeding.
2. Approach to obscure GI bleeding with video capsule endoscopy.
3. Recognition of rare causes including Dieulafoy's lesion, hemosuccus pancreaticus, and aortoenteric fistula.
4. Meckel's diverticulum is the most common cause of significant lower GI bleeding in children.
5. Risk stratification using Glasgow-Blatchford or Rockall scores to guide management and disposition.
PA Clinical Pearls
1. Serial hemoglobin measurements rather than single values provide better assessment of ongoing blood loss.
2. Bright red blood per rectum with hemodynamic instability suggests upper, not lower, GI source.
3. Consider medication-induced causes including NSAIDs, anticoagulants, SSRIs, and bisphosphonates.
4. Transient ischemic colitis commonly affects the "watershed" area near splenic flexure.
5. Gastric antral vascular ectasia ("watermelon stomach") is associated with cirrhosis and autoimmune disorders.
