PANCE - Gastritis & Peptic Ulcer Disease
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Gastritis & Peptic Ulcer Disease tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for PANCE.
Below is information not explicitly contained within the tutorial but important for PANCE.
- --
VITAL FOR PANCE
Disease Definitions & Pathogenesis
1. Gastritis is inflammation of the gastric mucosa; it can be diffuse or multi-focal.
2. Peptic ulcer disease is characterized by ulcers in the stomach and/or duodenum that penetrate the mucosa to reach the deeper layers of the GI tract.
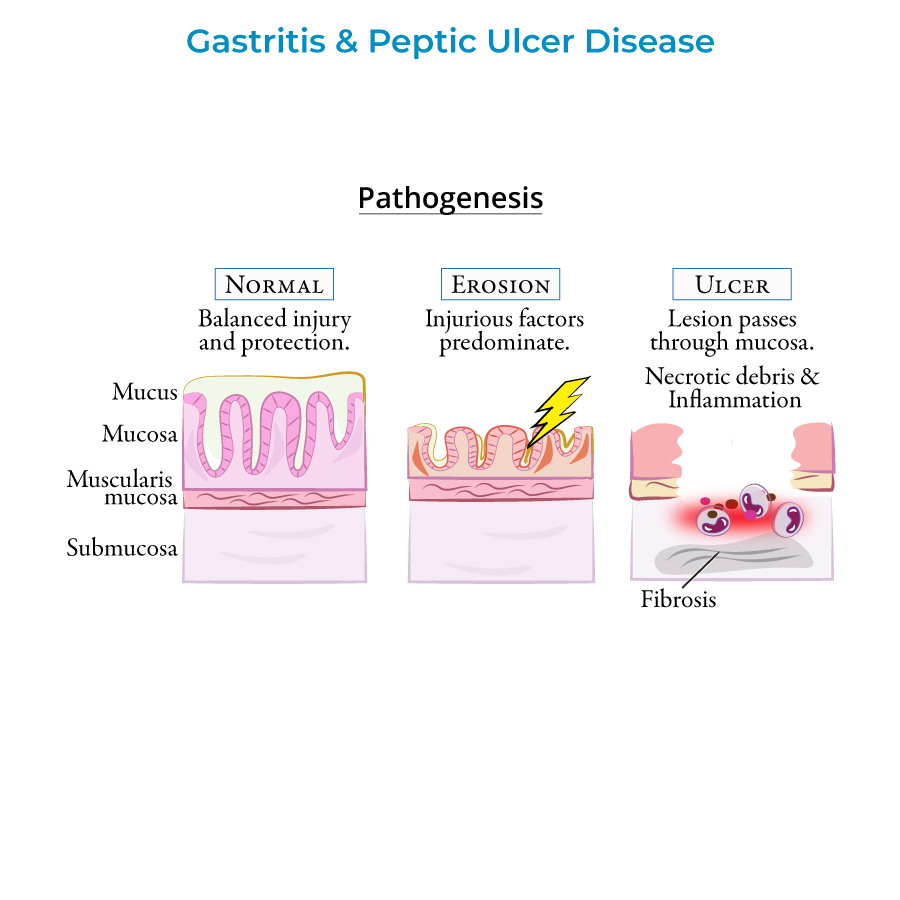
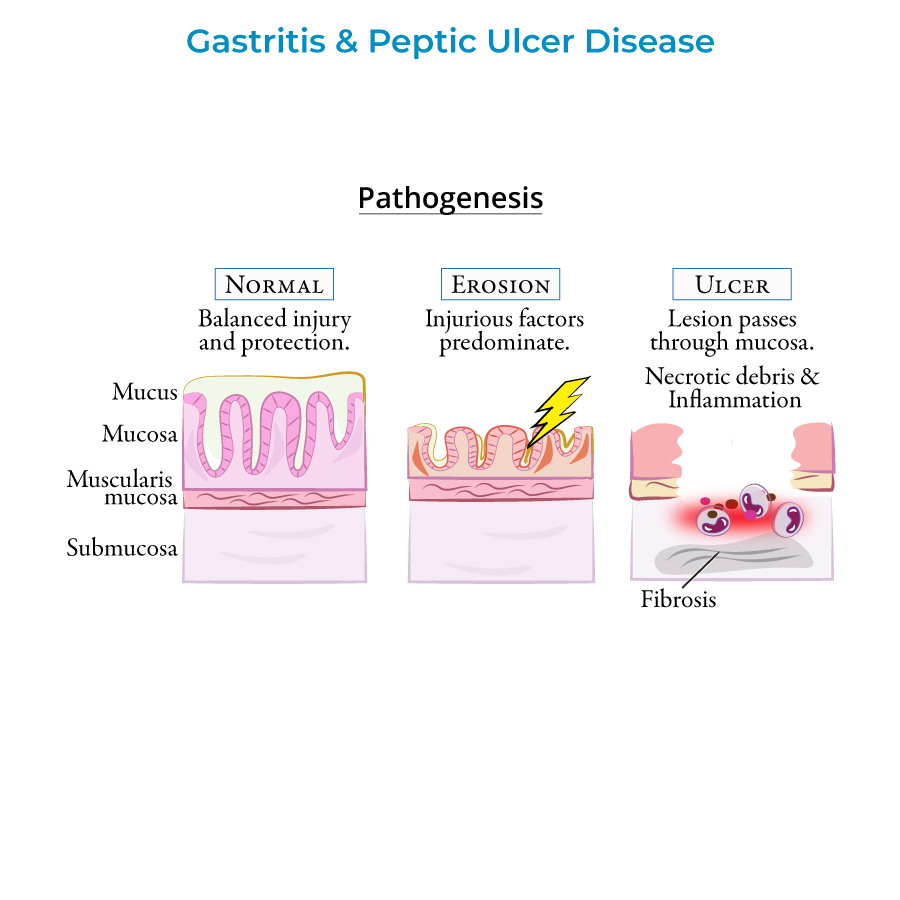
3. Healthy GI tissue layers from deep to superficial: submucosa, muscularis mucosa, mucosa, and the protective mucus layer.
4. As injurious factors predominate, the mucosa becomes inflamed and erosive lesions form.
5. Ulcers develop when lesions erode through the mucosa and deeper layers, showing necrotic debris with leukocyte infiltration, inflammation, and fibrosis in chronic cases.
Clinical Approach & Diagnosis
1. Signs and symptoms include epigastric pain, GI bleeding, nausea or vomiting; many patients are asymptomatic, especially in early phases.
2. Diagnosis relies on upper endoscopy to visualize lesions and biopsies to look for inflammation, H. pylori infection, and malignancy.
3. Urea breath test and stool antigen tests can also be used to look for H. pylori infection.
4. For patients younger than 60 years without alarming symptoms, focus on non-invasive H. pylori testing and PPI response.
5. For patients older than 60 years or with alarming symptoms (weight loss, anemia, bloody stools, dysphagia), upper endoscopy should be performed.
Treatment & Management
1. Treatment involves proton pump inhibitors, NSAID discontinuation, and H. pylori eradication with antibiotics when present.
2. Follow-up testing is necessary to confirm H. pylori eradication and prevent relapse.
3. Non-ulcer dyspepsia is treated with proton pump inhibitors after ruling out cancer in those over 55 years old.
4. Hemorrhage complications can be treated with endoscopic hemostasis therapies and proton pump inhibitors.
5. For gastric outlet obstruction, try treatment of the underlying peptic ulcer disease before attempting surgical solutions.
- --
HIGH YIELD
Etiology & Risk Factors
1. Key insults to the GI tract include H. pylori infection, NSAIDs, cigarette smoking, alcohol, and ischemia.
2. H. pylori is present in approximately 70% of gastric ulcer cases and 90% of duodenal ulcer cases.
3. NSAIDs block prostaglandin synthesis necessary for mucous production, while alcohol causes direct damage to the mucosal lining.
4. H. pylori is a gram-negative spirochete bacterium that raises stomach pH via urease and is classified as a class I carcinogen.
5. Contrary to popular belief, psychological stress and spicy foods do not cause peptic ulcers.
Clinical Presentations & Patterns
1. Acute gastritis occurs with sudden insult to the gastric mucosa, commonly from NSAIDs, aspirin, and alcohol.
2. Stress ulcers form secondary to acute, severe illness: Curling ulcers (systemic burns, hypovolemia) and Cushing ulcers (brain injury, increased vagal stimulation).
3. Chronic gastritis often leads to atrophy with loss of gastric glands and folds, increasing malignancy risk.
4. Gastric ulcer pain increases upon eating (leading to weight loss), while duodenal ulcer pain relieves with eating (possibly causing weight gain).
5. Perforation presents with sudden abdominal pain, tachycardia, abdominal rigidity, and pneumoperitoneum (free air under diaphragm) on imaging.
Complications & Special Considerations
1. Gastric ulcers have a higher risk of malignancy (5-10%) compared to duodenal ulcers, which are typically benign.
2. Peptic ulcers are the most common cause of upper GI bleeding, though most ulcers do not bleed.
3. Perforation has a high mortality rate (up to 30%) and requires emergency intervention.
4. Gastric outlet obstruction occurs due to inflammation and edema in acute cases; fibrosis and scarring in chronic cases.
5. H. pylori increases the risk of peptic ulcer disease, gastric cancer, and primary gastric MALT lymphomas.
- --
Beyond the Tutorial
Clinical Pearls
1. ROME IV criteria for functional dyspepsia: Bothersome postprandial fullness, early satiation, epigastric pain or burning, and no evidence of structural disease.
2. The "test and treat" strategy for H. pylori is cost-effective in high-prevalence populations; empiric PPI trial is preferred in low-prevalence regions.
3. Consider drug-induced causes of gastritis beyond NSAIDs: bisphosphonates, potassium supplements, iron, chemotherapeutic agents, and cocaine.
4. The Sydney System provides standardized gastritis classification based on topography, morphology, and etiology for consistent diagnosis and reporting.
5. Prostaglandin analogs (misoprostol) may be used prophylactically in high-risk patients who require continued NSAID therapy.
Treatment Protocols
1. First-line H. pylori treatment: 14-day triple therapy with PPI + clarithromycin + amoxicillin or metronidazole.
2. Bismuth quadruple therapy (PPI + bismuth + tetracycline + metronidazole) for clarithromycin-resistant regions or treatment failures.
3. Sequential therapy: 5 days of PPI + amoxicillin followed by 5 days of PPI + clarithromycin + metronidazole for improved eradication rates.
4. NSAID-associated ulcer prevention: PPI, H2RA, or misoprostol; consider COX-2 selective agents in high-risk patients.
5. Management of acute upper GI bleeding: Risk stratification using Glasgow-Blatchford or AIMS65 scores to determine level of care and timing of endoscopy.
