PANCE - Endocarditis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Endocarditis tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
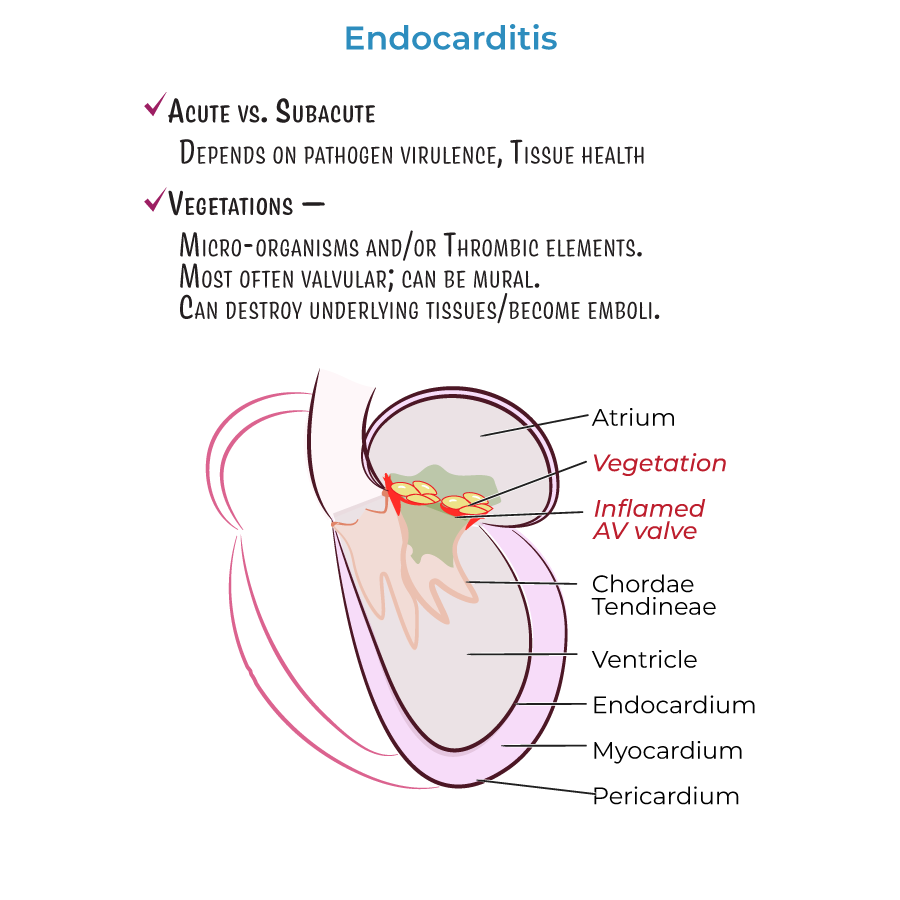
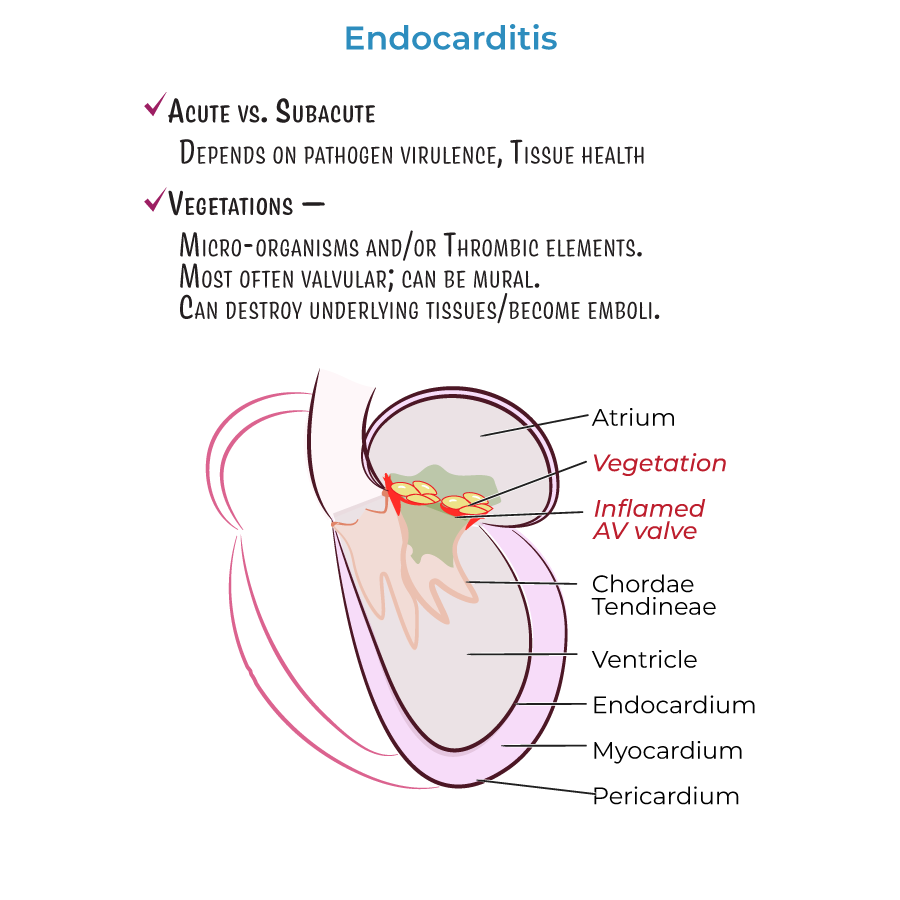 1. Endocarditis = inflammation of the internal lining of the heart (endocardium).
2. Can be acute or subacute, depending on pathogen virulence and cardiac tissue health.
3. Characterized by vegetations comprising microorganisms and/or thrombotic elements.
4. Most vegetations found on valvular ring or leaflets; "mural" vegetations form on heart walls.
5. Complications include tissue invasion/destruction and potential for emboli formation.
1. Endocarditis = inflammation of the internal lining of the heart (endocardium).
2. Can be acute or subacute, depending on pathogen virulence and cardiac tissue health.
3. Characterized by vegetations comprising microorganisms and/or thrombotic elements.
4. Most vegetations found on valvular ring or leaflets; "mural" vegetations form on heart walls.
5. Complications include tissue invasion/destruction and potential for emboli formation.
 Additional information important for PANCE:
Additional information important for PANCE:
- --
VITAL FOR PANCE
Definition and Pathophysiology
 1. Endocarditis = inflammation of the internal lining of the heart (endocardium).
2. Can be acute or subacute, depending on pathogen virulence and cardiac tissue health.
3. Characterized by vegetations comprising microorganisms and/or thrombotic elements.
4. Most vegetations found on valvular ring or leaflets; "mural" vegetations form on heart walls.
5. Complications include tissue invasion/destruction and potential for emboli formation.
1. Endocarditis = inflammation of the internal lining of the heart (endocardium).
2. Can be acute or subacute, depending on pathogen virulence and cardiac tissue health.
3. Characterized by vegetations comprising microorganisms and/or thrombotic elements.
4. Most vegetations found on valvular ring or leaflets; "mural" vegetations form on heart walls.
5. Complications include tissue invasion/destruction and potential for emboli formation.
Classification
1. Infective endocarditis: Contains pathogens in vegetations (also called bacterial endocarditis).
2. Non-infective endocarditis: Contains sterile vegetations (also called marantic or non-bacterial thrombotic endocarditis).
3. Culture-negative endocarditis: Infectious agent present but not identifiable by routine blood cultures.
Clinical Presentation
1. Acute endocarditis presents with fever, chills, and other flu-like symptoms.
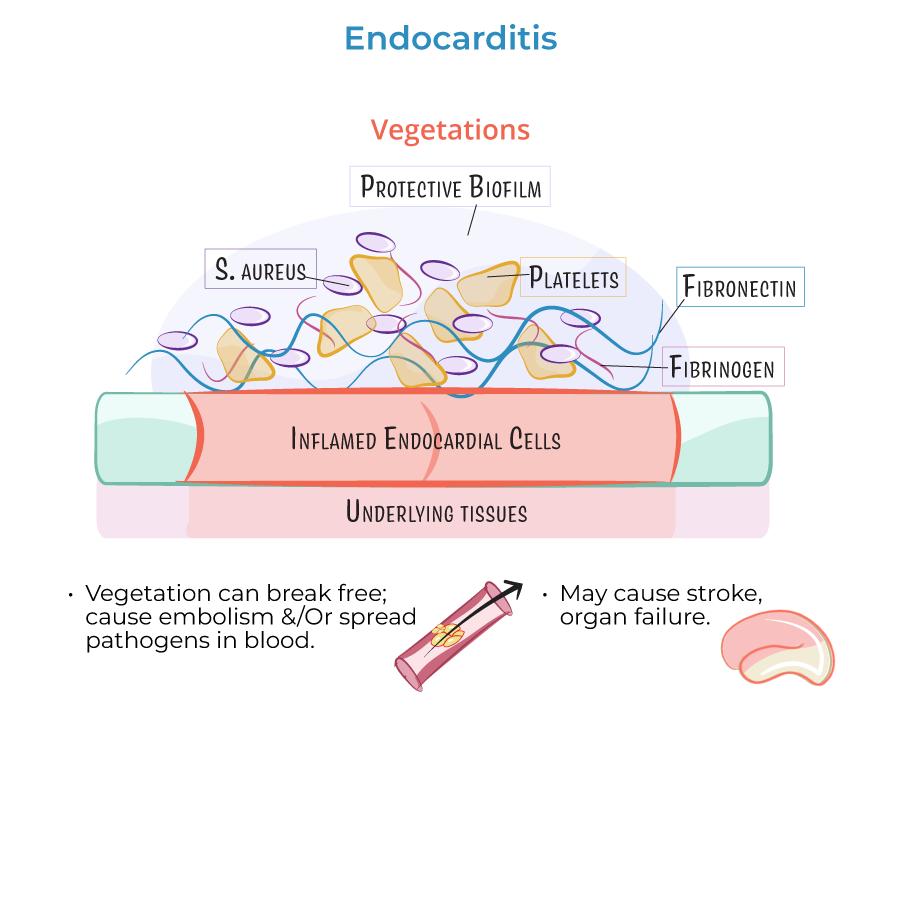
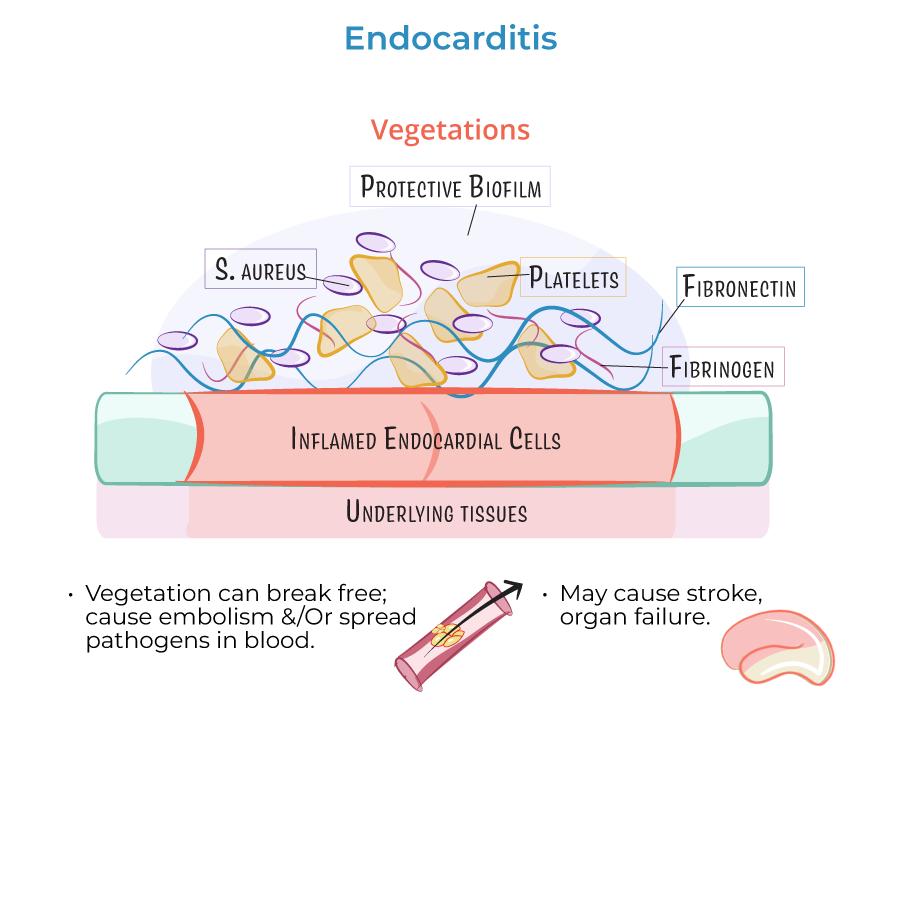
2. Complications include stroke, organ failure, and sepsis due to emboli lodging in blood vessels.
Common Pathogens
1. Gram-positive bacteria most common in infective endocarditis:
- Staphylococcus aureus (most common)
- Viridans group Streptococci
- Enterococci
- Coagulase-negative Staphylococci
- Haemophilus species
- Aggregatibacter species
- Cardiobacterium hominis
- Eikenella corrodens
- Kingella kingae
- --
HIGH YIELD
Pathophysiology and Vegetation Formation
1. Vegetations more likely to form where valvular damage already exists.
2. Initial inflammation often caused by catheter-induced abrasion or prosthetic devices.
3. Endothelial damage promotes fibronectin deposition and vegetation formation.
4. Fibronectin adheres to circulating fibrin, platelets, white blood cells, and pathogens.
5. Vegetations can break free causing embolism or pathogen spread in bloodstream.
Risk Factors and Patterns
1. Valvular patterns:
- Mitral valve regurgitation: Produces lesions on atrial leaflet surface
- Aortic insufficiency: Produces vegetations on ventricular side
- Ventricular septal defects: Right-sided vegetations near the orifice
- Intravenous drug users: Right-sided valvular endocarditis; introduction of particulate matter, skin pathogens, or oral flora
- Prosthetic valve patients: Higher infection susceptibility; commonly S. aureus and Coagulase-negative Staphylococci
- Rheumatic heart disease: Small vegetations near edge of leaflet
- Libman-Sacks endocarditis (associated with SLE): Small/medium vegetations on both sides of leaflets; loosely attached with increased embolism risk
- Culture-negative endocarditis: Consider Coxiella burnetii, Brucella species, Tropheryma whipplei
Clinical Correlations
1. Prosthetic valve endocarditis:
- Invasive vegetations form where prosthetic annular ring meets tissue
- Can deform valvular leaflets
- Often requires surgical valve replacement
- --
Beyond the Tutorial
Diagnostic Approach
1. Modified Duke criteria: Primary diagnostic framework
- Major criteria: Positive blood cultures, echocardiographic evidence
- Minor criteria: Predisposing conditions, fever, vascular/immunologic phenomena
- Blood cultures (3 sets from different sites before antibiotics)
- CBC (anemia, leukocytosis)
- Inflammatory markers (ESR, CRP)
- Urinalysis (hematuria, proteinuria)
- Transthoracic echocardiography (TTE): Initial screening
- Transesophageal echocardiography (TEE): Higher sensitivity, especially for prosthetic valves
Treatment Principles
1. Antimicrobial therapy:
- Empiric coverage based on likely pathogens
- Targeted therapy after culture results
- Extended duration (4-6 weeks for native valves, 6+ weeks for prosthetic)
- Heart failure from valvular dysfunction
- Uncontrolled infection (persistent bacteremia, abscess)
- Prevention of embolic events (large/mobile vegetations)
- Fungal endocarditis
- Limited to highest-risk patients (prosthetic valves, previous endocarditis)
- For dental procedures involving gingival manipulation
Clinical Pearls
1. Classic peripheral findings:
- Janeway lesions: Painless, erythematous macules
- Osler nodes: Painful, tender nodules
- Splinter hemorrhages: Linear subungual lesions
- Roth spots: Retinal hemorrhages with pale centers
- Infectious disease consultation for all cases
- Early cardiothoracic surgery evaluation when indicated
- Serial echocardiography to monitor treatment response
- Long-term follow-up for recurrence prevention
