PANCE - Atherosclerosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Atherosclerosis Tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR PANCE
Disease Basics and Pathophysiology
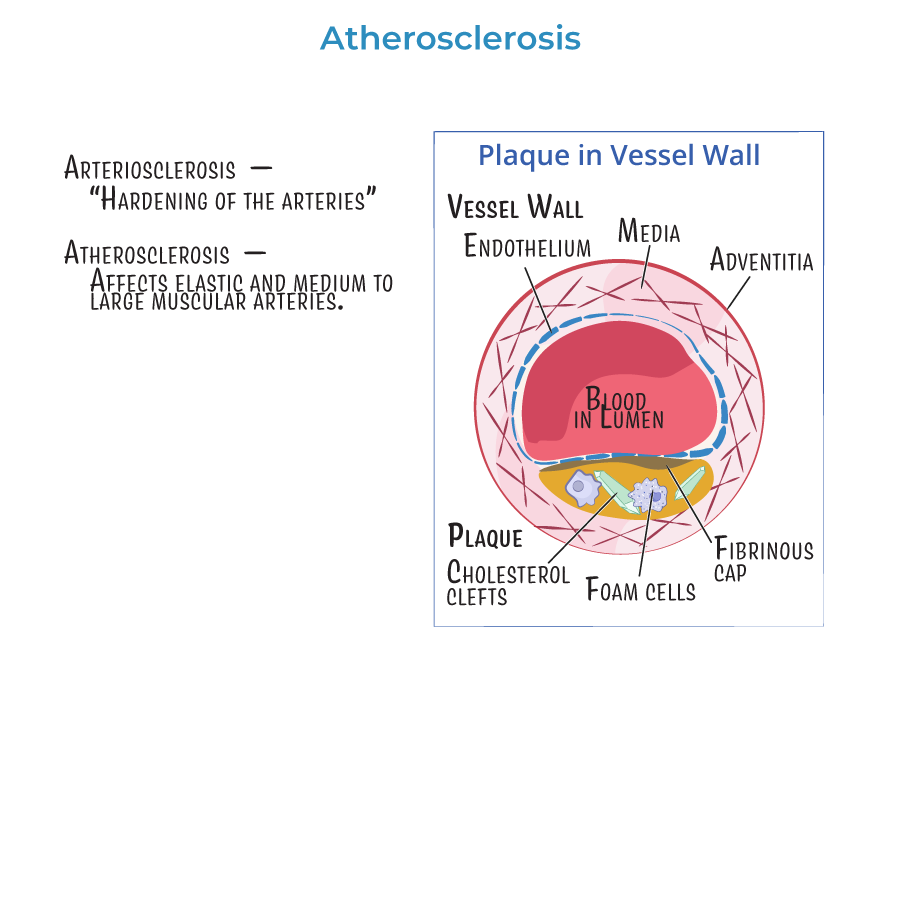
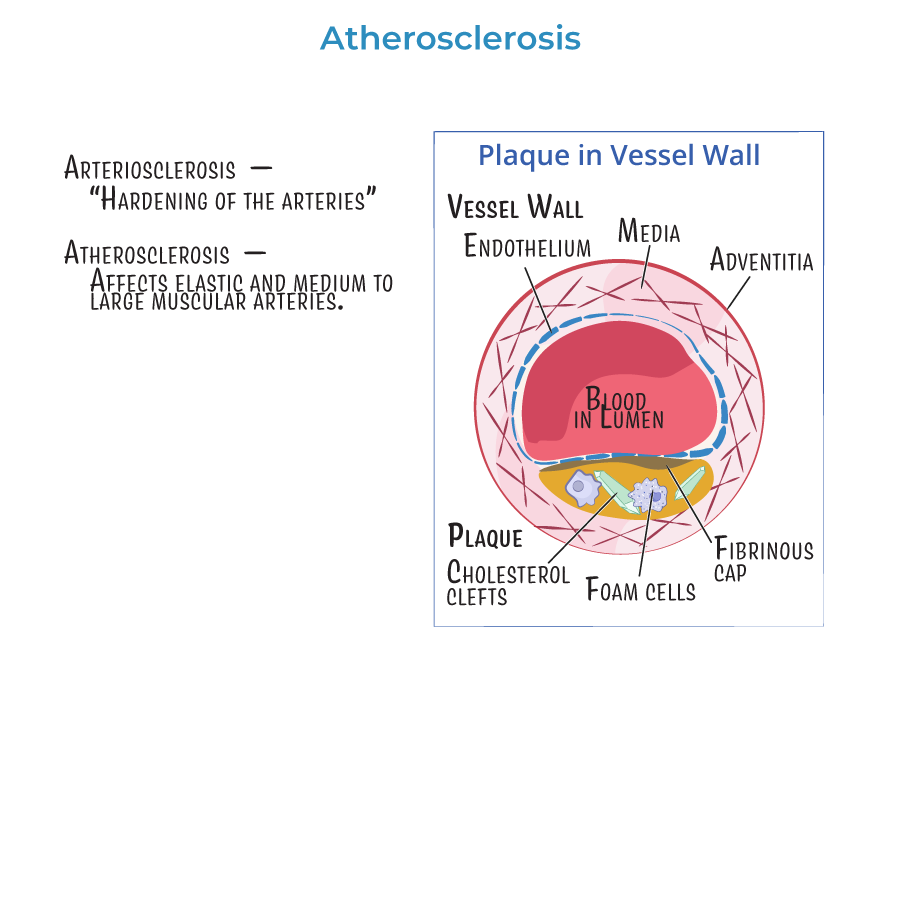
1. Atherosclerosis is the buildup of cholesterol-laden plaques within the walls of medium and large arteries, leading to reduced blood flow and vascular events.
2. It is the pathophysiological basis for coronary artery disease (CAD), peripheral artery disease (PAD), cerebrovascular disease (stroke/TIA), and aortic aneurysms.
3. Plaques may rupture and cause acute thrombosis, leading to MI or ischemic stroke.
4. Atherosclerosis begins with endothelial injury, followed by lipid accumulation, macrophage infiltration, foam cell formation, and fibrous cap development.
5. Plaque stability is a major determinant of whether the lesion leads to chronic symptoms or an acute event.
Clinical Presentations
6. CAD: exertional chest pain relieved by rest (stable angina), or sudden worsening (unstable angina/MI).
7. PAD: intermittent claudication, diminished pulses, non-healing ulcers.
8. CVA/TIA: sudden-onset neurologic deficits or brief ischemic episodes.
9. Aneurysm/Dissection: back or chest pain, pulsatile mass, or hypotension in ruptured cases.
Risk Factors and Screening
10. Modifiable risk factors: hyperlipidemia (esp. high LDL), hypertension, smoking, diabetes, obesity, sedentary lifestyle.
11. Non-modifiable risk factors: age, male sex, family history of early ASCVD.
12. Screening tools:
- Lipid panel (at baseline and routinely every 4–6 years)
- Ankle-Brachial Index (ABI) for PAD
- Coronary Artery Calcium (CAC) score in intermediate-risk patients
- --
HIGH YIELD
Diagnostics
1. Fasting lipid profile is the main tool to assess cardiovascular risk.
2. ABI < 0.90 is diagnostic for PAD; lower values indicate greater severity.
3. Carotid Doppler ultrasound assesses for stenosis in TIA or asymptomatic bruits.
4. CT angiography or MRA can evaluate aortic aneurysm/dissection and PAD when interventions are planned.
5. Coronary calcium scoring helps refine ASCVD risk in intermediate-risk adults.
Treatment and Pharmacology
6. Statins are the first-line therapy for both primary and secondary prevention:
- High-intensity statins (e.g., atorvastatin 40–80 mg) reduce LDL by ≥50%.
Lifestyle Modification
10. Non-pharmacologic interventions are foundational:
- Smoking cessation
- DASH or Mediterranean diet
- Regular aerobic exercise
- Weight reduction if overweight/obese
- --
Beyond the Tutorial
Case-Based Integration
1. A 62-year-old man with HTN, DM, and LDL of 160 should be started on a high-intensity statin, even in the absence of symptoms.
2. A 55-year-old female with intermittent leg pain relieved by rest and ABI of 0.8 has PAD and requires statin, antiplatelet, and risk factor control.
3. A patient with new-onset erectile dysfunction may need cardiovascular workup for underlying atherosclerosis.
4. In a patient with carotid bruit, order a Doppler ultrasound to evaluate for significant stenosis.
5. Sudden tearing chest pain and hypotension may suggest aortic dissection—immediate CT angiography and surgical consult are needed.
Monitoring and Follow-Up
6. Recheck lipids 4–12 weeks after initiating therapy, then every 6–12 months.
7. Monitor for statin side effects: myalgia, elevated transaminases, or rare rhabdomyolysis.
8. Educate patients to report muscle pain, dark urine, or fatigue.
9. Long-term monitoring includes routine BP, HbA1c, and lifestyle follow-up.
10. Lifelong management may include combination therapy, particularly in high-risk or refractory cases.
