PANCE - Adrenal Insufficiency
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for PANCE from the Adrenal Insufficiency tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR PANCE
Classification and Overview
1. Adrenal insufficiency is associated with high morbidity and mortality, which increase when diagnosis is delayed.
2. Primary adrenal insufficiency (PAI), also called Addison's disease, is caused by adrenal gland dysfunction.
3. Central adrenal insufficiency is caused by a deficiency in CRH and/or ACTH.
4. In chronic AI, adrenal reserves may initially maintain basal hormone levels, but with impaired ACTH stress response.
Clinical Presentation
1. Primary AI affects all adrenal cortex hormones (cortisol, aldosterone, and androgens).
2. Primary AI patients present with hyperpigmentation of skin and mucosa, hypotension, hyponatremia, hyperkalemia, and metabolic acidosis.
3. Chronic Primary AI symptoms include weakness, fatigue, weight loss, gastrointestinal problems, and salt cravings.
4. Central AI primarily affects cortisol and androgen secretion (aldosterone secretion is maintained).
5. Central AI shows no hyperpigmentation and less hypovolemia/hypotension than primary AI.
Adrenal Crisis
1. Be suspicious of adrenal crisis in patients with acute shock refractory to vasopressors and fluid replacement.
2. Acute adrenal crisis occurs when AI patients face additional stressors (infections, trauma, surgery, dehydration).
3. Presents with shock, fever, dehydration, nausea, vomiting, hypoglycemia, apathy, and weakness.
4. Adrenal crisis is life-threatening and requires immediate intervention.
Diagnosis
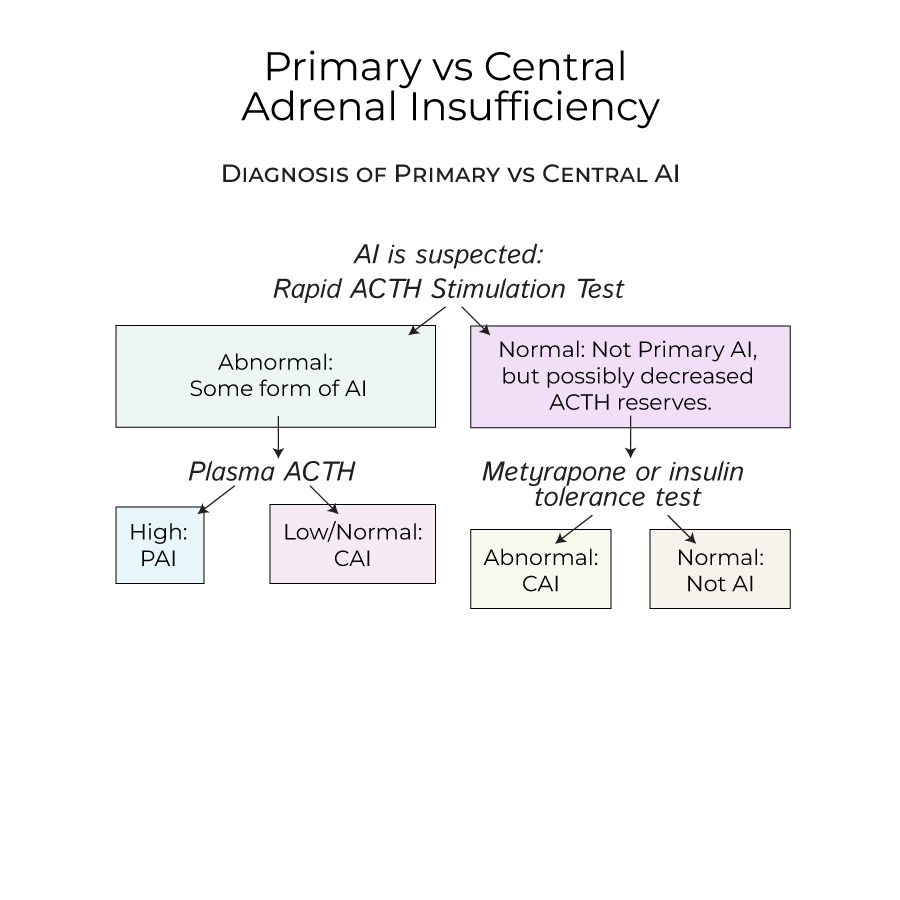
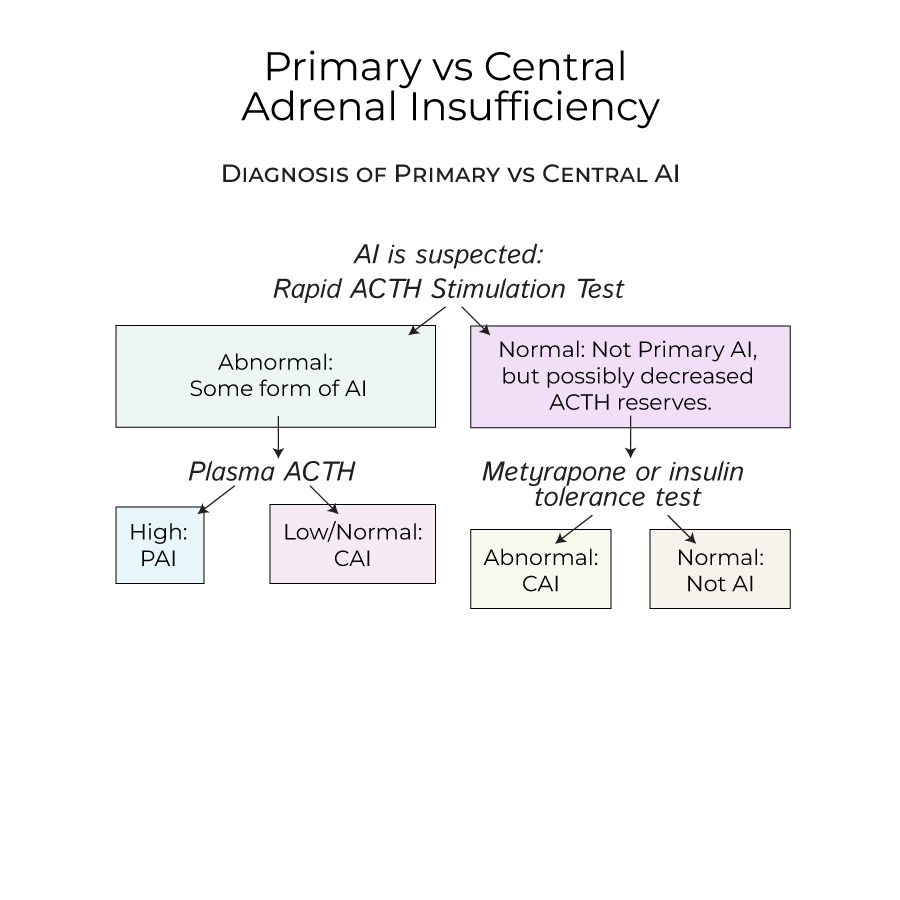
1. When AI is suspected, perform a rapid ACTH stimulation test.
2. If cortisol levels are abnormal after ACTH stimulation, high plasma ACTH indicates Primary AI; low/normal ACTH indicates Central AI.
- --
HIGH YIELD
Causes of Primary AI
1. Autoimmune diseases are the most common causes of primary AI in the United States.
2. Autoimmune Polyendocrine Syndrome Type 1 (APS-1) presents with adrenal insufficiency, hypoparathyroidism, and mucocutaneous candidiasis.
3. Autoimmune Polyendocrine Syndrome Type 2 (APS-2) is associated with adrenal insufficiency, Hashimoto's thyroiditis, and Type I diabetes mellitus.
4. Infections (TB, HIV) are important causes in endemic countries.
5. Bilateral adrenal hemorrhage risk factors include anti-coagulation therapy and disorders like antiphospholipid antibody syndrome and SLE.
6. Waterhouse-Friderichsen Syndrome in children presents with adrenal bleeding caused by septicemia, often with meningococcal or pseudomonas infections.
Causes of Central AI
1. Most commonly caused by long-term exogenous steroid use or sudden cessation.
2. May be caused by pituitary/hypothalamic dysfunction (tumors, infections, drugs).
3. Drugs that interrupt ACTH production include immune checkpoint inhibitors, high-dose progestins, and opioids.
4. Often associated with deficiencies of other pituitary hormones.
Treatment Principles
1. Treatment includes glucocorticoid replacement for all forms of AI.
2. Mineralocorticoid replacement is needed only for primary AI.
3. To avoid adrenal crisis, provide additional glucocorticoid doses during stressors like surgery.
4. Beware of overtreatment with glucocorticoids, which can produce Cushing's syndrome.
5. Patients should carry medical cards warning of their condition.
Special Considerations
1. Primary AI affects slightly more women than men, typically diagnosed at 30-50 years.
2. The adrenal gland blood supply (three arteries, one vein) makes it vulnerable to hemorrhage.
3. Advanced testing for early central AI includes metyrapone administration or insulin tolerance tests.
4. Patients with APS are likely to have additional endocrine-related disorders.
- --
Beyond the Tutorial
Clinical Approach for PAs
1. Maintain a low threshold for suspicion in patients with unexplained hypotension, fatigue, and electrolyte abnormalities.
2. Consider adrenal insufficiency in all patients on chronic steroid therapy presenting with acute illness.
3. Remember that hyperpigmentation is a key differentiator between primary and central AI.
4. Establish a clear protocol for stress-dose steroids in your practice for AI patients undergoing procedures.
Patient Education
1. Educate patients about the importance of medication adherence and danger signs of adrenal crisis.
2. Provide clear instructions for dose adjustments during illness, including when to seek medical attention.
3. Ensure patients have emergency injectable steroids and know how to use them.
4. Emphasize the importance of medical alert identification and emergency plan documentation.
Monitoring and Follow-up
1. Schedule regular follow-ups to assess treatment adequacy and adjust doses as needed.
2. Monitor for complications of chronic glucocorticoid therapy (osteoporosis, diabetes, hypertension).
3. Screen for associated conditions in autoimmune primary AI.
4. Coordinate care with endocrinology specialists, especially for complex cases or during pregnancy.
