Hemophilia for NP
Start your One-Week Free Trial
Already subscribed? Log in »
Hemophilia for the Nurse Practitioner Licensing Exam
- Definition:
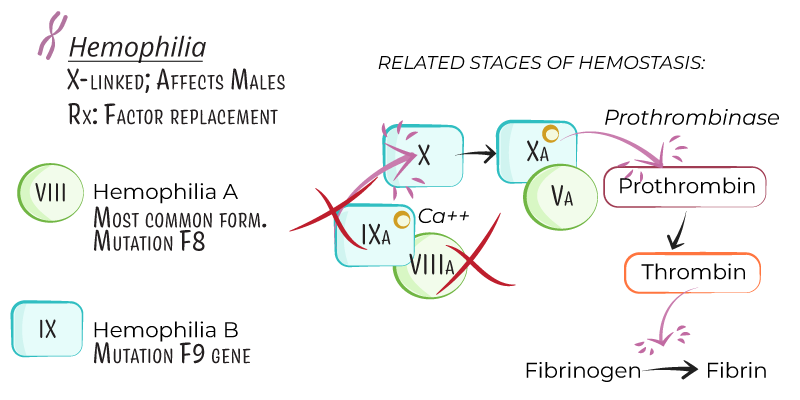
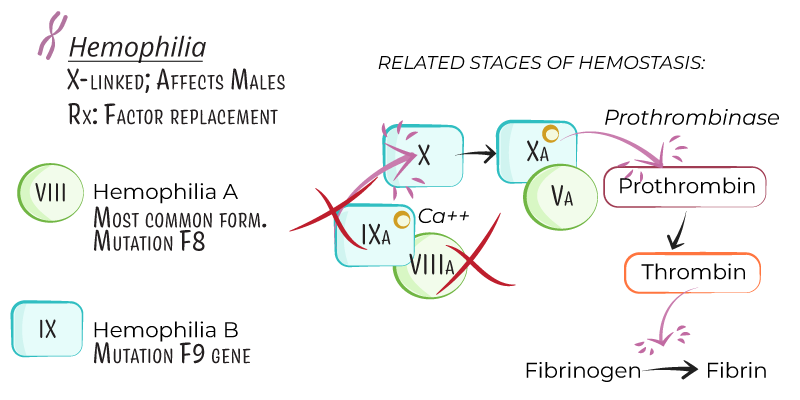
- Hemophilia is an X-linked recessive bleeding disorder caused by deficiencies in specific clotting factors, leading to prolonged bleeding and impaired clot formation.
- Primarily affects males, as the defective gene is located on the X chromosome, though some female carriers may have mild symptoms.
- Types:
- Hemophilia A: Factor VIII deficiency, more common, comprising ~80% of cases.
- Hemophilia B (Christmas Disease): Factor IX deficiency, accounting for ~20% of cases.
Pathophysiology and Severity
- Factor Deficiency:
- Factor VIII and factor IX are intrinsic pathway proteins essential for the activation of factor X and stable clot formation.
- Deficiencies result in delayed thrombin formation, leading to prolonged bleeding.
- Severity:
- Severe: Factor activity <1% of normal, with spontaneous bleeding.
- Moderate: Factor activity 1–5%, with bleeding after mild trauma.
- Mild: Factor activity 5–40%, with bleeding only after significant trauma or surgery.
Clinical Presentation
- Bleeding Sites:
- Hemarthrosis: Recurrent bleeding in joints (knees, elbows, ankles), leading to joint damage if untreated.
- Muscle Bleeding: Deep muscle bleeding, particularly in the thigh or iliopsoas.
- Mucocutaneous Bleeding: Uncommon but may occur with minor injuries.
- Intracranial Hemorrhage: Life-threatening and often trauma-induced.
- Post-Traumatic Bleeding:
- Prolonged bleeding after minor surgeries or injuries, especially in mild or moderate hemophilia.
Diagnosis
- Laboratory Findings:
- Prothrombin Time (PT): Normal.
- Activated Partial Thromboplastin Time (aPTT): Prolonged due to intrinsic pathway defect.
- Factor Assays: Low levels of factor VIII (hemophilia A) or factor IX (hemophilia B) confirm the diagnosis.
Treatment
- Factor Replacement Therapy:
- On-Demand: For active bleeding.
- Prophylactic: Regular infusions in severe cases to prevent spontaneous bleeding.
- Bypassing Agents: Recombinant factor VIIa or activated prothrombin complex concentrate (aPCC) for patients with inhibitors.
- Emicizumab:
- A bispecific antibody used for prophylaxis in hemophilia A, effective even in patients with inhibitors.
- Adjunctive Therapies:
- Antifibrinolytics: Tranexamic acid for mucosal bleeding or dental procedures.
- Pain Management: Acetaminophen preferred to avoid platelet inhibition by NSAIDs.
Key Points
- Hemophilia is an X-linked recessive disorder due to factor VIII or IX deficiency, primarily affecting males.
- Severity depends on factor levels, with spontaneous bleeding in severe cases.
- Diagnosis involves prolonged aPTT and specific factor assays.
- Management includes factor replacement, emicizumab for hemophilia A, and antifibrinolytics for mucosal bleeding.
