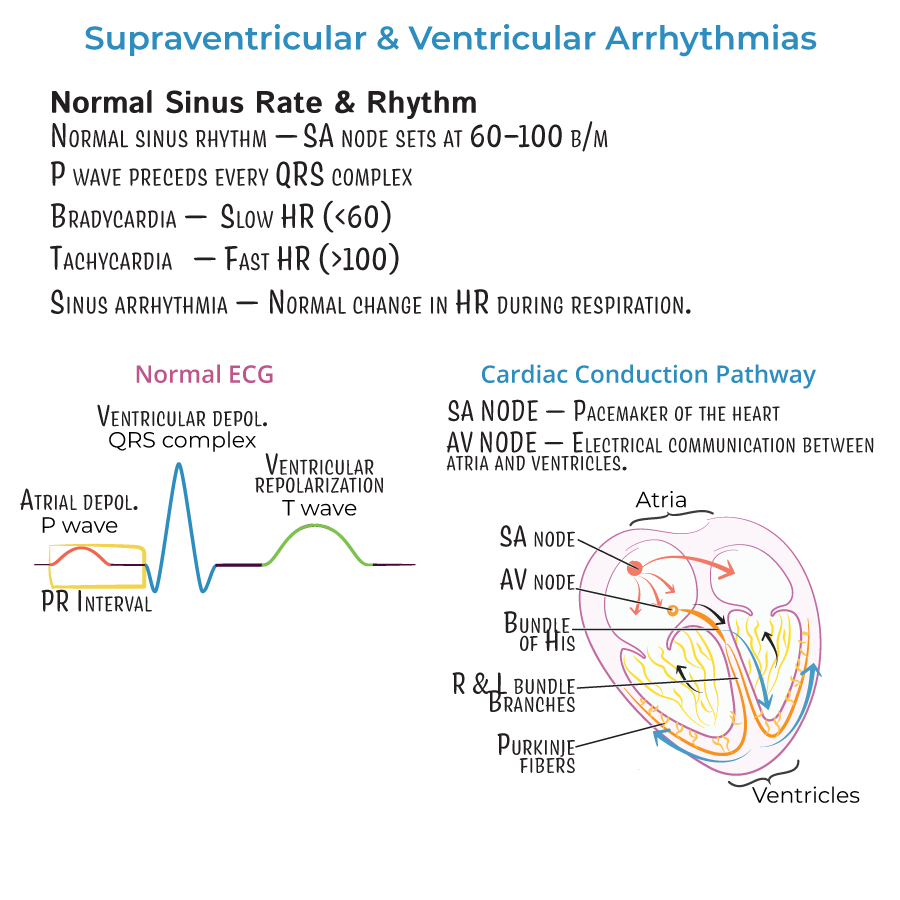
NCLEX Focus - Supraventricular & Ventricular Arrhythmias
Start your One-Week Free Trial
Already subscribed? Log in »
The following are high yield points from the Supraventricular & Ventricular Arrhythmias tutorial to help you prepare for the NCLEX.
Review Supraventricular Arrhythmias and Ventricular Arrhythmias for further details.
 A 61-year-old woman presents after a syncopal episode at home. She was recently prescribed levofloxacin for a urinary tract infection. Her EKG reveals prolonged QT interval. What is the most likely cause of her syncope?
A 58-year-old male with ST-elevation myocardial infarction suddenly becomes unresponsive and pulseless. Cardiac monitoring shows chaotic, irregular electrical activity without identifiable P, QRS, or T waves. What is the nurse’s next best action?
A 19-year-old patient with Wolff-Parkinson-White (WPW) syndrome is experiencing supraventricular tachycardia. Which of the following medications should be avoided due to risk of triggering ventricular fibrillation?
A 76-year-old male presents with fatigue and palpitations. ECG shows irregularly irregular rhythm with no distinct P waves. What is the most likely diagnosis?
A code is called for a 70-year-old patient who is unresponsive and pulseless. The cardiac monitor shows organized electrical activity without a palpable pulse. What is the nurse’s next best step?
A nurse is assessing a patient admitted with new-onset atrial fibrillation. Which of the following findings is most concerning for decreased cardiac output?
A 61-year-old woman presents after a syncopal episode at home. She was recently prescribed levofloxacin for a urinary tract infection. Her EKG reveals prolonged QT interval. What is the most likely cause of her syncope?
A 58-year-old male with ST-elevation myocardial infarction suddenly becomes unresponsive and pulseless. Cardiac monitoring shows chaotic, irregular electrical activity without identifiable P, QRS, or T waves. What is the nurse’s next best action?
A 19-year-old patient with Wolff-Parkinson-White (WPW) syndrome is experiencing supraventricular tachycardia. Which of the following medications should be avoided due to risk of triggering ventricular fibrillation?
A 76-year-old male presents with fatigue and palpitations. ECG shows irregularly irregular rhythm with no distinct P waves. What is the most likely diagnosis?
A code is called for a 70-year-old patient who is unresponsive and pulseless. The cardiac monitor shows organized electrical activity without a palpable pulse. What is the nurse’s next best step?
A nurse is assessing a patient admitted with new-onset atrial fibrillation. Which of the following findings is most concerning for decreased cardiac output?
NCLEX Focus
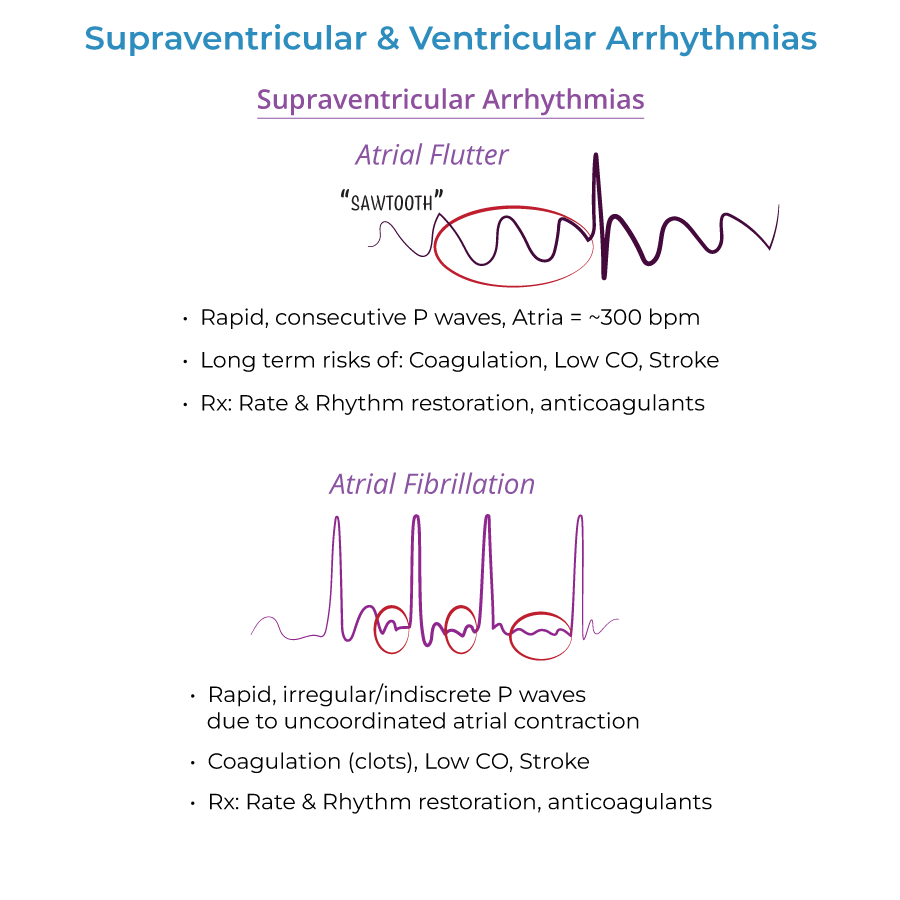
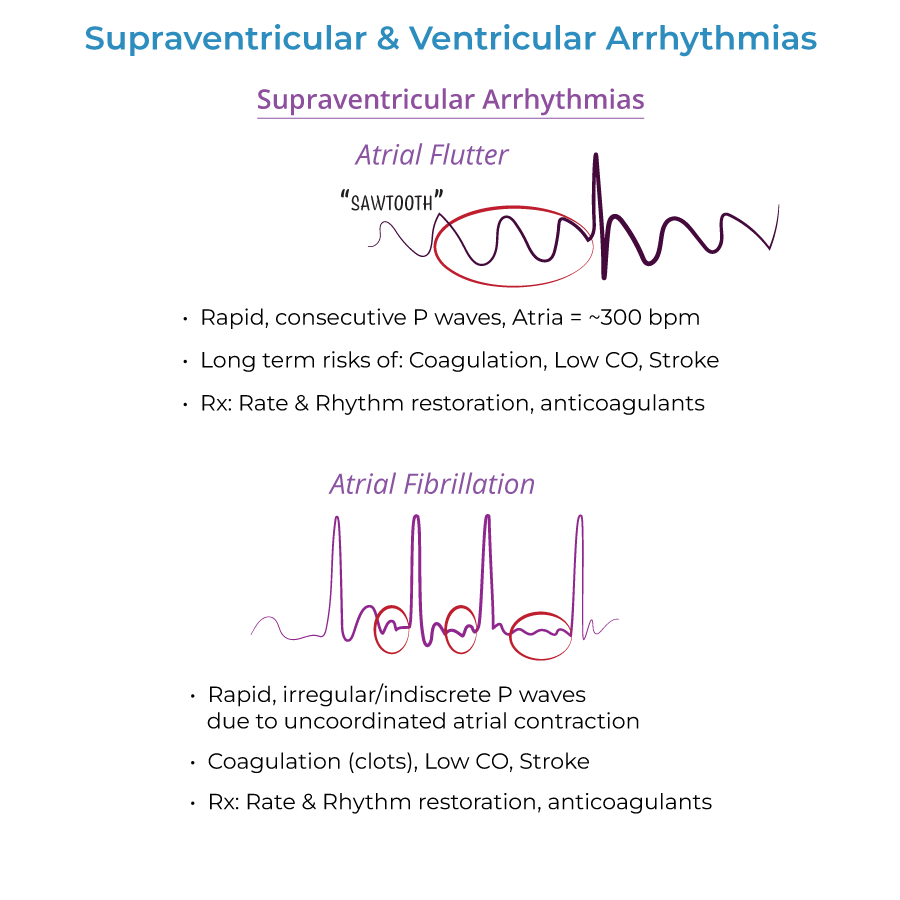
Atrial Flutter
- ECG: Regular, rapid "sawtooth" P waves; atrial rate ~300 bpm, ventricular rate ~150 bpm.
- Symptoms: May be asymptomatic or cause palpitations, chest discomfort, syncope, dyspnea.
- Treatment:
- Rate control: Beta blockers, nondihydropyridine calcium channel blockers (verapamil, diltiazem).
- Rhythm control: Cardioversion, antiarrhythmic drugs, or ablation.
- Stroke prevention: Anticoagulation (e.g., warfarin).
- --
Atrial Fibrillation
- ECG: Irregular, rapid P waves; no organized atrial contraction; irregularly irregular rhythm.
- Symptoms: Fatigue, palpitations, dizziness, dyspnea; can be asymptomatic.
- Treatment:
- Rate control: Beta blockers or calcium channel blockers.
- Rhythm control: Anticoagulation before cardioversion.
- Avoid AV node blockers in WPW syndrome — can be fatal.
- Risk Factors: Cardiac disease, hyperthyroidism, lung disease, obesity, alcohol.
- Clinical Concerns:
- High risk of stroke/systemic embolism.
- Evaluate with echocardiography, thyroid function tests.
- Must rule out Wolff-Parkinson-White (WPW) before certain treatments.
- --
Asystole
- ECG: Flatline; no electrical activity.
- Description: Complete cardiac standstill.
- Treatment: CPR and epinephrine (1 mg IV every 3–5 min).
- Clinical Concern: Non-shockable rhythm; fatal without immediate intervention.
- --
Pulseless Electrical Activity (PEA)
- ECG: Normal or abnormal rhythm without a palpable pulse.
- Treatment: CPR + epinephrine, treat underlying cause (H’s and T’s).
- Clinical Concern: One of the most common rhythms in cardiac arrest.
- --
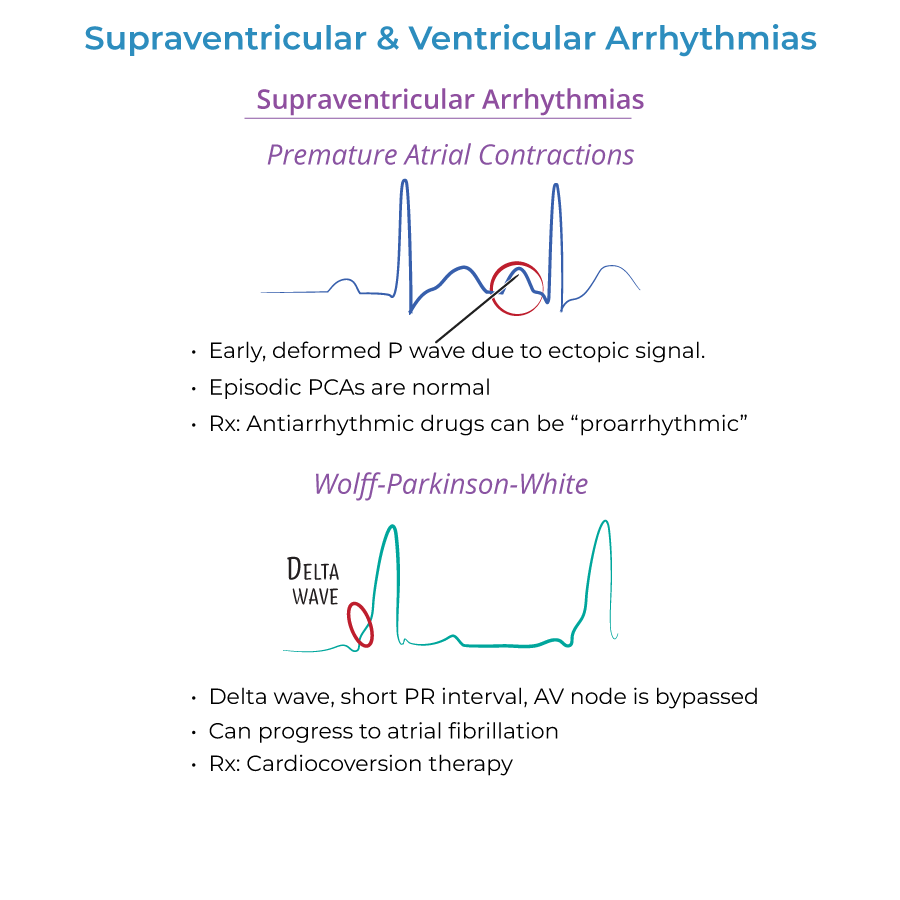
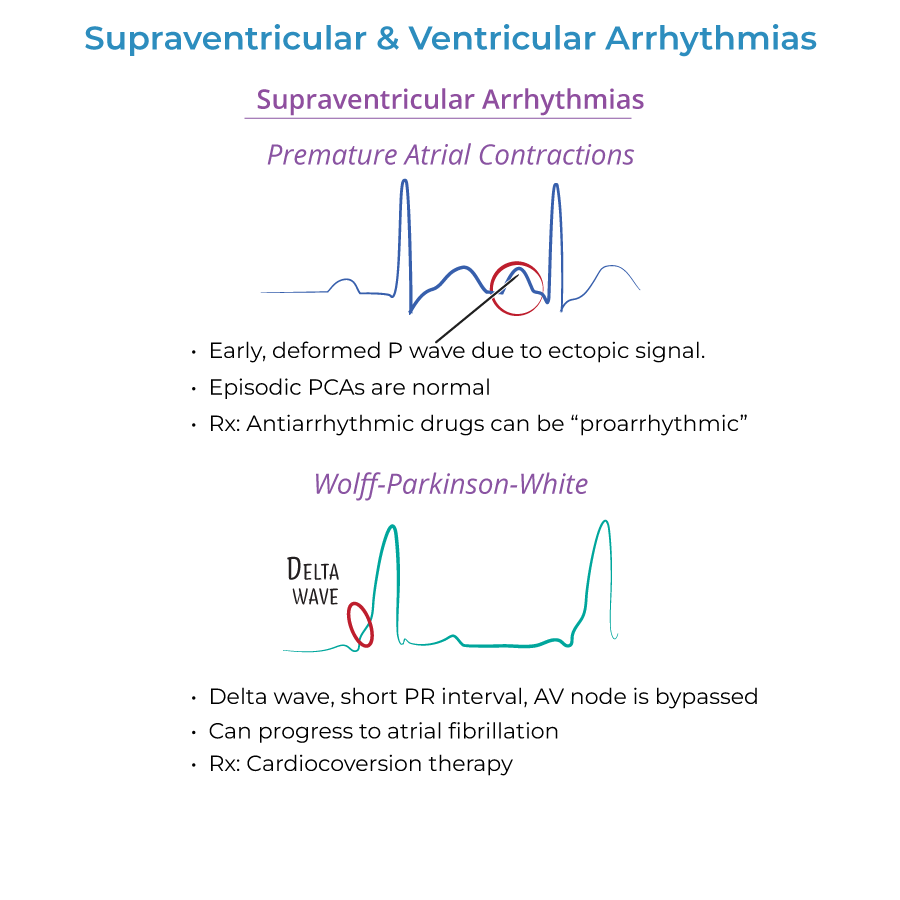
Premature Beats (PACs/PVCs)
- ECG: Early atrial or ventricular beats from ectopic focus.
- Symptoms: “Skipped beats,” palpitations.
- Treatment: Usually none if asymptomatic; avoid unnecessary antiarrhythmics.
- Risk Factors: Caffeine, stress, alcohol, hypoxia, electrolyte disturbances.
- Clinical Concern: May progress to atrial flutter/fibrillation.
- --
Wolff-Parkinson-White (WPW) Syndrome
- ECG: Short PR interval, delta wave, broad QRS.
- Cause: Accessory pathway (Bundle of Kent) bypassing AV node.
- Symptoms: Palpitations, dizziness, tachycardia; can be asymptomatic.
- Treatment: Cardioversion; definitive = catheter ablation.
- Avoid AV node blockers (e.g., digoxin, CCBs) — may induce ventricular fibrillation.
- Risk Factors: Congenital, linked to Ebstein anomaly.
- Clinical Concern: Can lead to fatal arrhythmias if mismanaged.
- --
Ventricular Tachycardia (VT)
- ECG: 3+ consecutive ventricular beats >120 bpm; wide QRS.
- Symptoms: Palpitations, dizziness, fainting, dyspnea; may be asymptomatic if short (paroxysmal).
- Treatment: Cardioversion, antiarrhythmics, or defibrillator implant.
- Risk Factors: Heart disease, medications, electrolyte imbalances.
- Clinical Concern: Can cause sudden death, heart failure, or loss of consciousness.
- --
Torsades de Pointes
- ECG: Twisting, spiral-shaped QRS pattern on a fluctuating baseline.
- Subtype: Polymorphic VT associated with prolonged QT.
- Symptoms: Palpitations, dizziness, fainting, dyspnea.
- Treatment: IV magnesium is first-line.
- Risk Factors: Hypokalemia, hypocalcemia, QT-prolonging drugs (e.g., levofloxacin, erythromycin).
- Clinical Concern: Can lead to ventricular fibrillation and death.
- --
Long QT Syndrome
- ECG: Prolonged QT interval due to defective repolarization (ion channel issues).
- Inherited Forms:
- Romano-Ward Syndrome (Types 1–3)
- Jervell and Lange-Nielsen Syndrome (with congenital deafness)
- Acquired Causes:
- Medications (e.g., antiarrhythmics, antidepressants, antihistamines, diuretics)
- Electrolyte imbalances (hypokalemia, hypocalcemia)
- Clinical Concern: Leads to Torsades de Pointes, syncope, sudden death.
- --
Ventricular Fibrillation (VF)
- ECG: Chaotic, disorganized electrical activity; no identifiable waves.
- Symptoms: Unresponsiveness, cardiac arrest.
- Treatment: Immediate defibrillation + CPR.
- Risk Factors: Ischemic heart disease, cardiomyopathies, Brugada syndrome.
- Clinical Concern: Always fatal without prompt defibrillation.
NCLEX Questions
