NCLEX Focus - Hypertension Pathophysiology
Start your One-Week Free Trial
Already subscribed? Log in »
The following are high yield points from the Hypertension Pathophysiology tutorial to help you prepare for the NCLEX.
Review this Hypertension Pathophysiology flashcard for further details.
NCLEX Focus
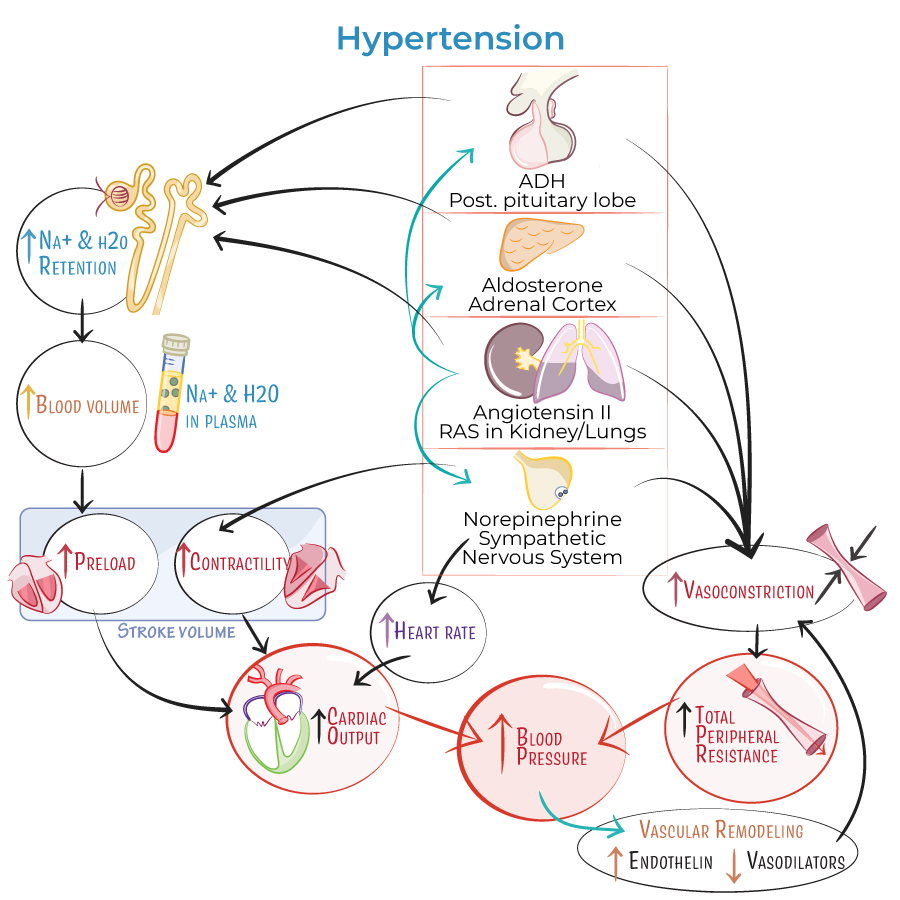
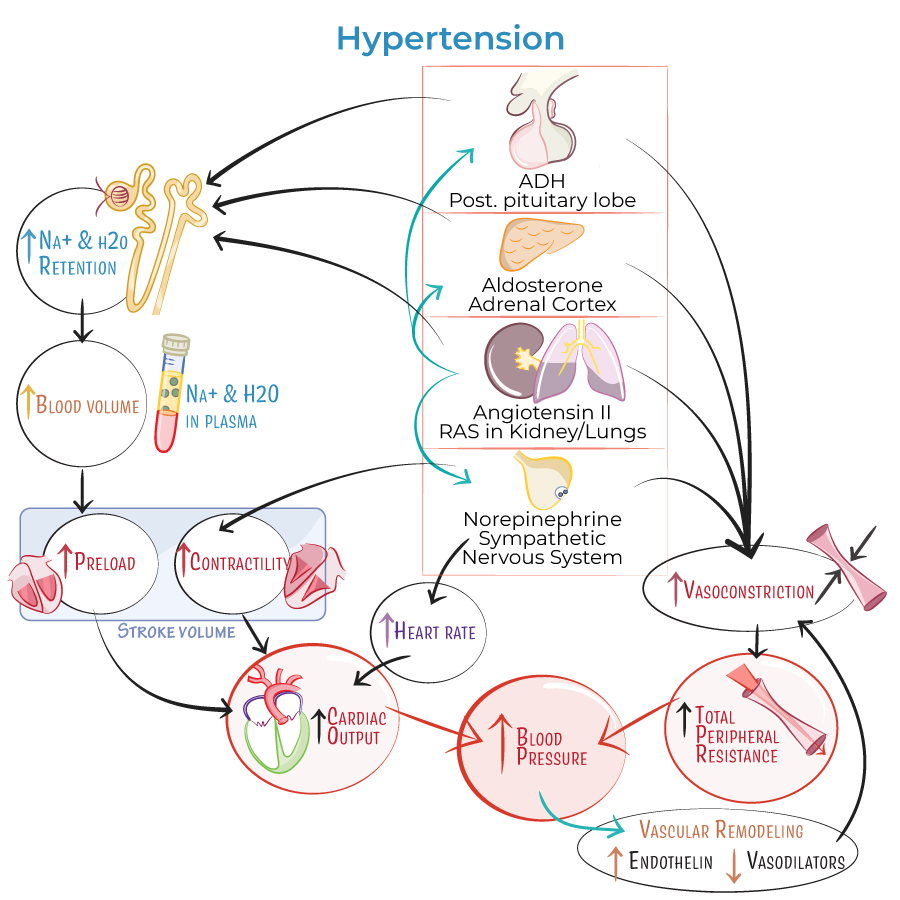
Determinants of Mean Arterial Pressure (MAP)
- Mean arterial pressure is regulated by cardiac output and total peripheral resistance.
- Cardiac output is the product of heart rate and stroke volume.
- Stroke volume depends on preload and contractility.
- Preload is influenced by venous return, which is largely determined by blood volume.
- Blood volume is affected by sodium and water retention, primarily controlled by renal function.
- --
Total Peripheral Resistance (TPR)
- TPR is regulated by the degree of vasoconstriction, especially in small arteries and arterioles.
- Increased vasoconstriction raises TPR, thereby increasing blood pressure.
- --
Hormonal Regulators of Blood Pressure
Several hormones contribute to hypertension by increasing cardiac output and/or TPR:
- Antidiuretic hormone (vasopressin)
- Released by the posterior pituitary
- Causes vasoconstriction and water reabsorption in kidneys
- Increases blood volume and cardiac output
- Aldosterone
- Secreted by the adrenal cortex
- Promotes sodium and water retention
- Raises blood volume and pressure
- Angiotensin II
- Stimulates vasoconstriction, sodium/water retention, and release of aldosterone and ADH
- Central to the renin-angiotensin-aldosterone system
- Targeted by multiple antihypertensive medications
- Norepinephrine
- Increases heart rate, contractility, and vasoconstriction
- --
Vascular Remodeling and Local Mediators
- Chronic hypertension causes vascular inflammation and damage, resulting in vascular remodeling.
- Remodeling leads to:
- Increased levels of endothelin (a potent vasoconstrictor)
- Decreased production of vasodilators like nitric oxide
- Vasodilators include:
- Nitric oxide
- Prostaglandins
- Histamine
- Bradykinin (degraded by angiotensin-converting enzyme, ACE)
- ACE inhibitors lower blood pressure by reducing angiotensin II and preserving bradykinin levels.
- --
Clinical Integration
- Salt sensitivity, aldosterone-secreting tumors, and similar conditions raise blood volume, leading to hypertension through increased preload.
- Lifestyle factors, genetics, and environmental variables influence any part of this system and contribute to primary hypertension.
- --
Hypertensive Crisis
- Defined by blood pressure exceeding 180/120 mmHg.
- Two types:
- Hypertensive urgency: No end-organ damage
- Hypertensive emergency: Evidence of end-organ damage
- Symptoms of hypertensive emergency include:
- Severe headache, visual changes, confusion
- Chest pain, shortness of breath
- Nausea, vomiting, anxiety, seizures
