NCLEX Atherosclerosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Atherosclerosis Tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR NCELX
Clinical Understanding
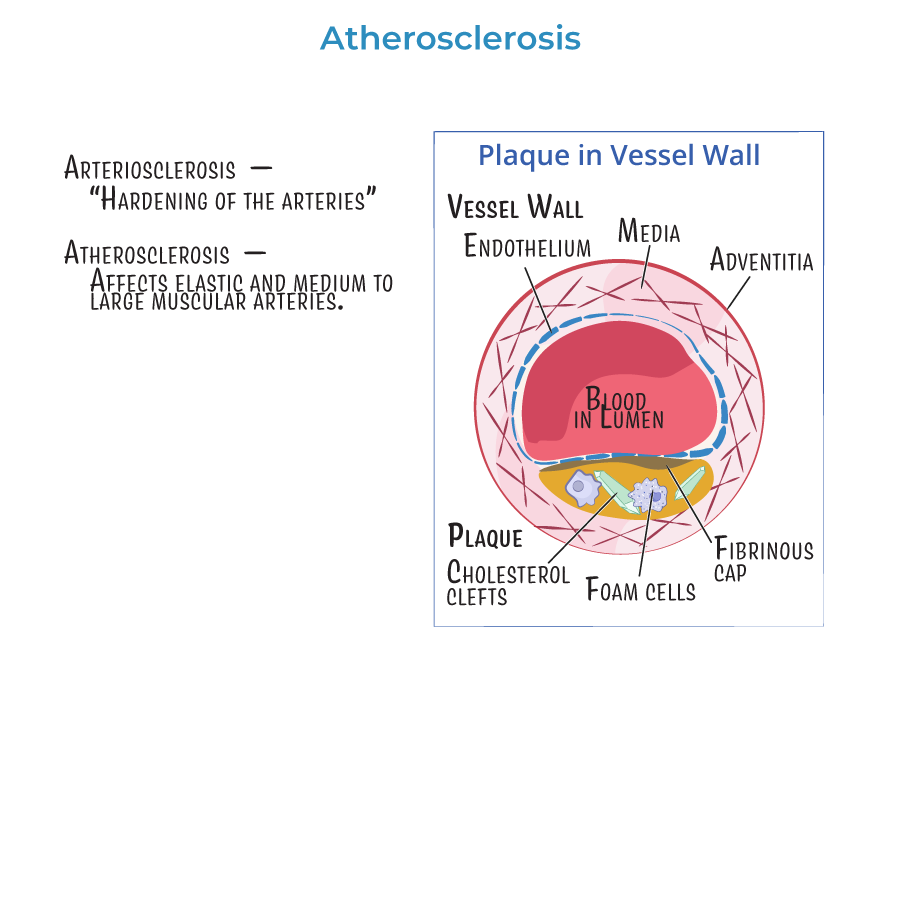
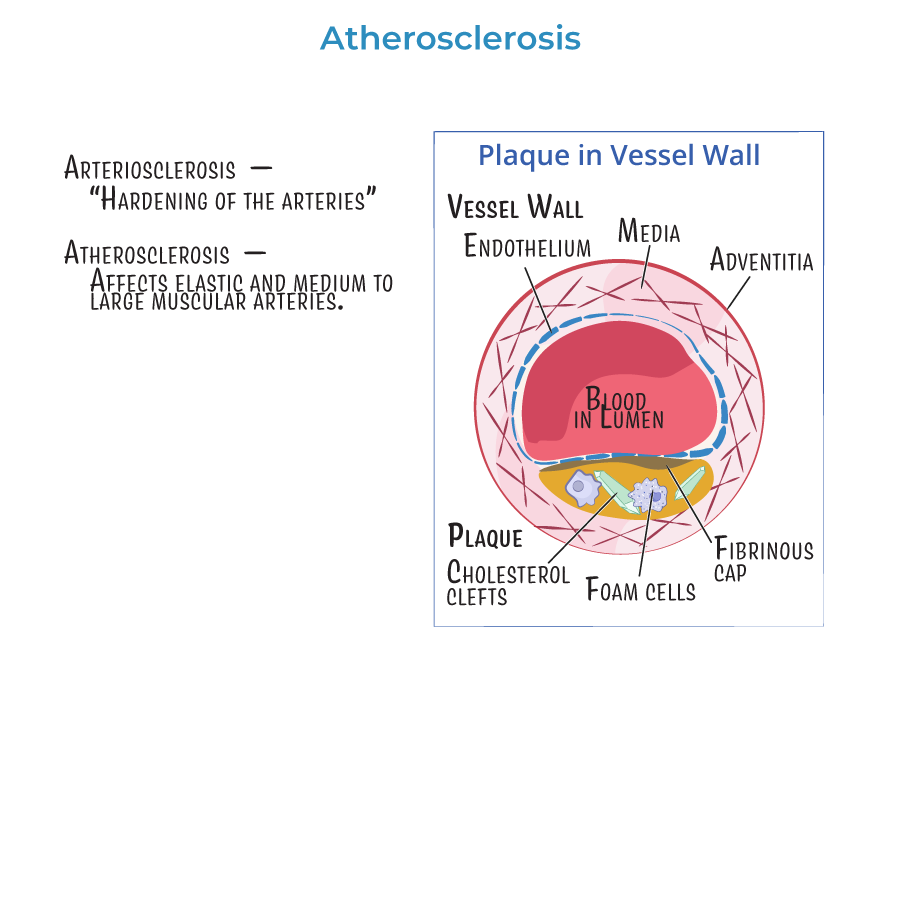
1. Atherosclerosis is a type of arteriosclerosis involving fat and cholesterol buildup (plaque) in medium and large arteries.
2. This condition leads to narrowing of blood vessels, reducing blood flow and oxygen delivery to tissues.
3. It is the primary cause of coronary artery disease, heart attack, stroke, peripheral artery disease (PAD), and aortic aneurysm/dissection.
4. Common symptoms include:
- Chest pain (angina) in coronary artery disease
- Claudication (leg pain with walking) in PAD
- Numbness or weakness in stroke or TIA
Nursing Priorities
6. Monitor vital signs, especially blood pressure and heart rate, to reduce vascular strain.
7. Educate patients on lifestyle changes: low-fat diet, exercise, smoking cessation.
8. Administer prescribed statins, and monitor for side effects like muscle pain or elevated liver enzymes.
9. Encourage adherence to medications for blood pressure, cholesterol, and diabetes.
10. Report any signs of sudden chest pain, vision changes, confusion, or limb pain immediately — these could indicate ischemia or infarction.
- --
HIGH YIELD
Risk Factors and Prevention
1. Major modifiable risk factors:
- High LDL cholesterol
- Hypertension
- Smoking
- Diabetes
- Obesity
- Sedentary lifestyle
- Age
- Male sex
- Family history of cardiovascular disease
- Lipid panel: measures cholesterol and triglycerides
- Blood glucose and A1c for diabetes
- Blood pressure readings
- Low-sodium, low-fat diet (DASH or heart-healthy)
- Physical activity (30 minutes/day, 5 days/week)
- Avoidance of tobacco and excessive alcohol
Medications and Safety
5. Statins are used to lower LDL and stabilize plaques.
6. Teach patients to report muscle pain or weakness, a sign of rhabdomyolysis, a rare but serious side effect.
7. Antiplatelet medications like aspirin may be prescribed for secondary prevention.
8. Blood pressure medications like ACE inhibitors and beta-blockers reduce strain on arteries and lower stroke/MI risk.
Complications to Monitor
9. Myocardial infarction: chest pain, shortness of breath, sweating, nausea.
10. Stroke/TIA: facial droop, arm weakness, slurred speech.
11. PAD: cold extremities, diminished pulses, poor wound healing.
12. Aneurysm/dissection: severe back pain, hypotension, pulseless extremities — report immediately.
- --
Beyond the Tutorial
Patient Teaching and Community Health
1. Encourage routine checkups and cholesterol screening beginning at age 20 and earlier if family history is positive.
2. Help patients develop realistic goals: e.g., 5–10% weight loss improves cardiovascular health.
3. Teach importance of medication adherence, even if symptoms are absent.
4. Instruct patients recovering from MI or stroke to attend cardiac rehab and follow up with primary care.
5. Nurses play a key role in prevention by providing education in community and clinic settings.
NCLEX Nursing Strategies
6. Prioritize unstable patients with signs of stroke, MI, or aortic rupture.
7. Use the SBAR format when reporting deterioration to providers.
8. Recognize statin adverse effects early: monitor CK, AST/ALT, and renal function if muscle symptoms arise.
9. Provide emotional support to patients with chronic vascular disease, who may experience anxiety or depression.
10. Collaborate with dietitians, pharmacists, and case managers to promote safe, coordinated care.
