NCLEX - Aortic Aneurysm & Dissection
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Aortic Aneurysm & Dissection, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.

- --
VITAL FOR NCLEX
Aortic Aneurysm
1. Abdominal Aortic Aneurysm (AAA) often affects older men with history of smoking, hypertension, and atherosclerosis.
2. Key signs of AAA include abdominal or back pain, a pulsatile abdominal mass, and sometimes hypotension if rupturing.
3. If AAA ruptures, the patient may present with hypovolemic shock (low blood pressure, tachycardia, cold clammy skin).
4. Ultrasound is used for screening and diagnosis of AAA.
5. Monitor patients with small AAAs with regular ultrasound and promote smoking cessation.
6. Emergency surgery is needed for ruptured or symptomatic AAAs.
7. Postoperative care includes monitoring for bleeding, renal function (urine output), and blood pressure control.

Thoracic Aortic Aneurysm
8. Symptoms include chest pain, back pain, hoarseness, cough, and dysphagia due to pressure on nearby structures.
9. CT angiography is the preferred imaging study.
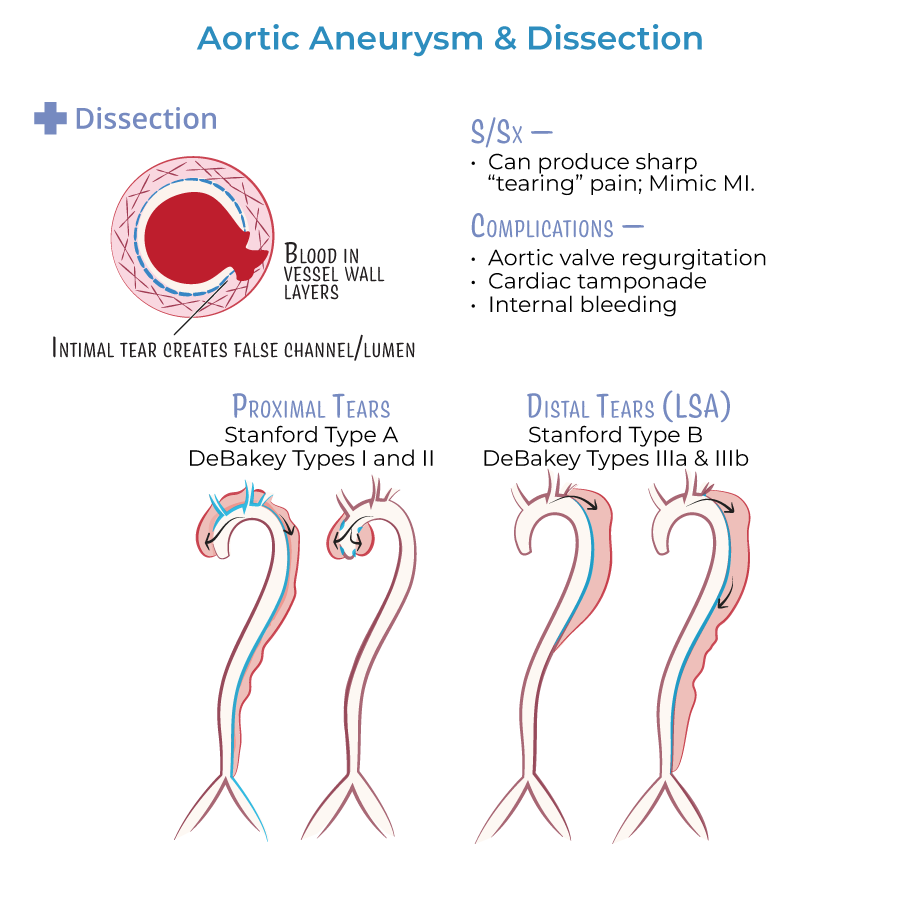
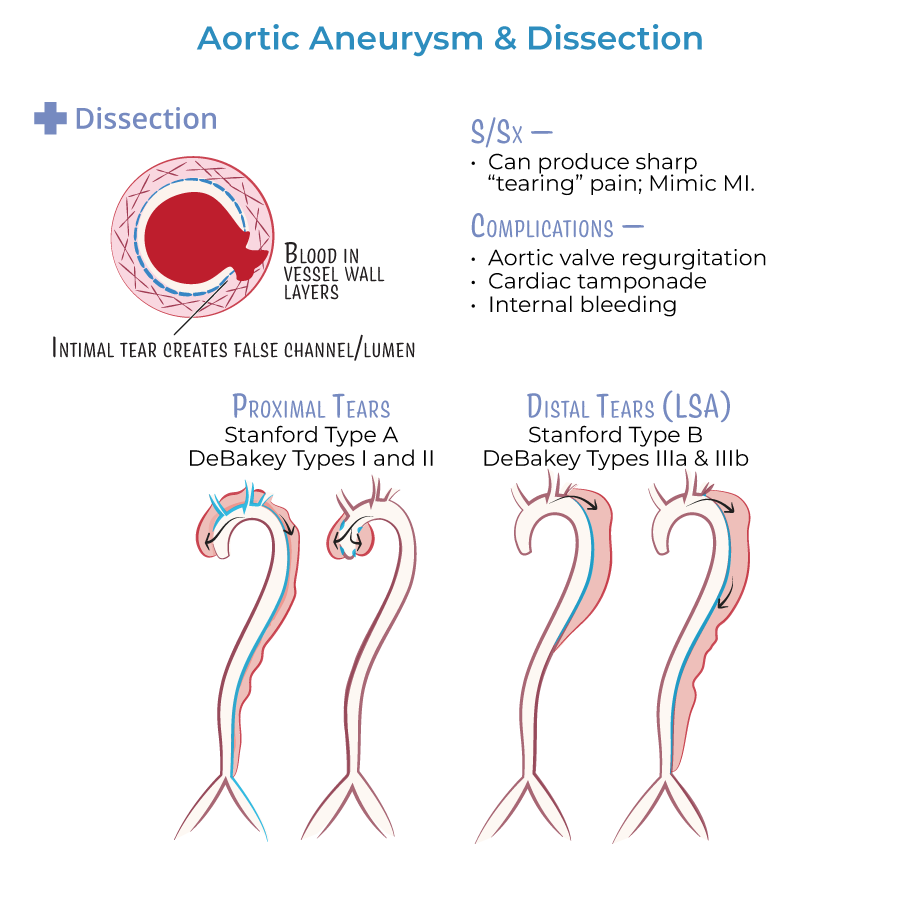
Aortic Dissection
10. Aortic dissection presents with sudden, severe "tearing" chest or back pain.
11. Look for differences in blood pressure between arms or pulse deficits.
12. Stanford Type A dissections (ascending aorta) require emergency surgery.
13. Stanford Type B dissections (descending aorta) are usually treated with medication first unless complications occur.
14. Immediate nursing priority: administer IV beta-blocker to lower heart rate and blood pressure and prevent further tearing.
15. Monitor for complications like stroke symptoms, cardiac tamponade (low BP, JVD, muffled heart sounds), and renal failure.
- --
HIGH YIELD
Risk Factors and Causes
1. Hypertension is the leading cause of aortic dissection.
2. Smoking and atherosclerosis are major risk factors for AAA development.
3. Marfan syndrome and Ehlers-Danlos syndrome increase the risk of thoracic aneurysms and dissections.
Signs and Symptoms
4. Thoracic aneurysm rupture may cause sudden chest or back pain, hoarseness, dysphagia, and shock.
5. AAA rupture causes hypotension, flank pain, and signs of shock.
6. New diastolic murmur can indicate aortic valve regurgitation from Type A dissection.
Diagnostic Tests
7. CT angiography is the test of choice if the patient is stable.
8. TEE (transesophageal echocardiography) is used if the patient is unstable.
9. Chest x-ray may show widened mediastinum in aortic dissection.
Nursing Interventions
10. Maintain strict blood pressure control during acute events.
11. Prepare the patient for emergency surgery if rupture or Type A dissection is confirmed.
12. After surgery, monitor for peripheral perfusion, renal function, infection, and bleeding.
13. Teach patients about smoking cessation, medication adherence, and monitoring blood pressure.
14. Recognize that Fluoroquinolone antibiotics can increase the risk of aneurysm rupture.
- --
Beyond the Tutorial
Emergency Nursing and Prioritization
1. In patients with signs of AAA rupture or dissection, keep NPO, ensure IV access, administer oxygen, and prepare for surgery.
2. Pain assessment and control are critical to reduce sympathetic stimulation and prevent worsening dissection.
3. Patients with hypotension and a pulsatile abdominal mass should be prioritized for emergency surgical consultation immediately.
4. Monitor urine output closely post-op to assess for renal perfusion; target >30 mL/hr.
5. Avoid lifting heavy objects during AAA recovery to prevent stress on the surgical site.
Discharge Teaching
6. Teach patients recovering from aneurysm repair to monitor for signs of graft infection (fever, redness, swelling).
7. Reinforce lifelong blood pressure control with medications.
8. Schedule regular imaging follow-up (e.g., annual CT or ultrasound) after aneurysm repair.
