NCELX - Large Vessel Vasculitis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Large Vessel Vasculitis tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR NCLEX
Recognition of Critical Symptoms
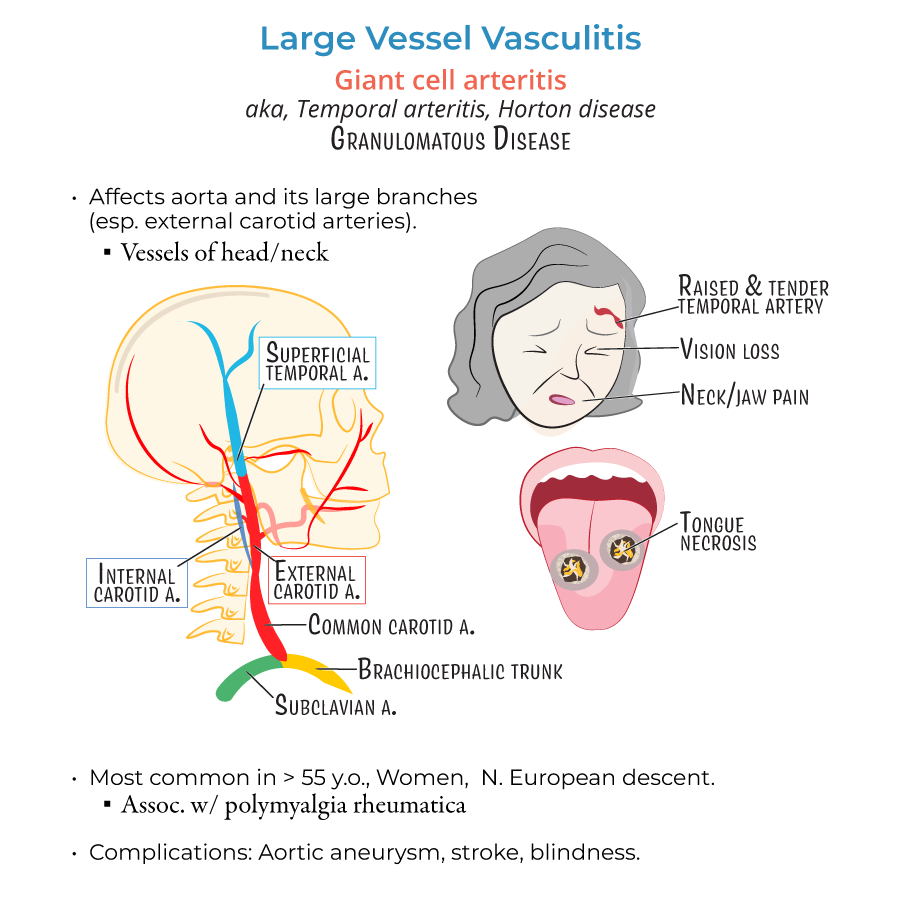
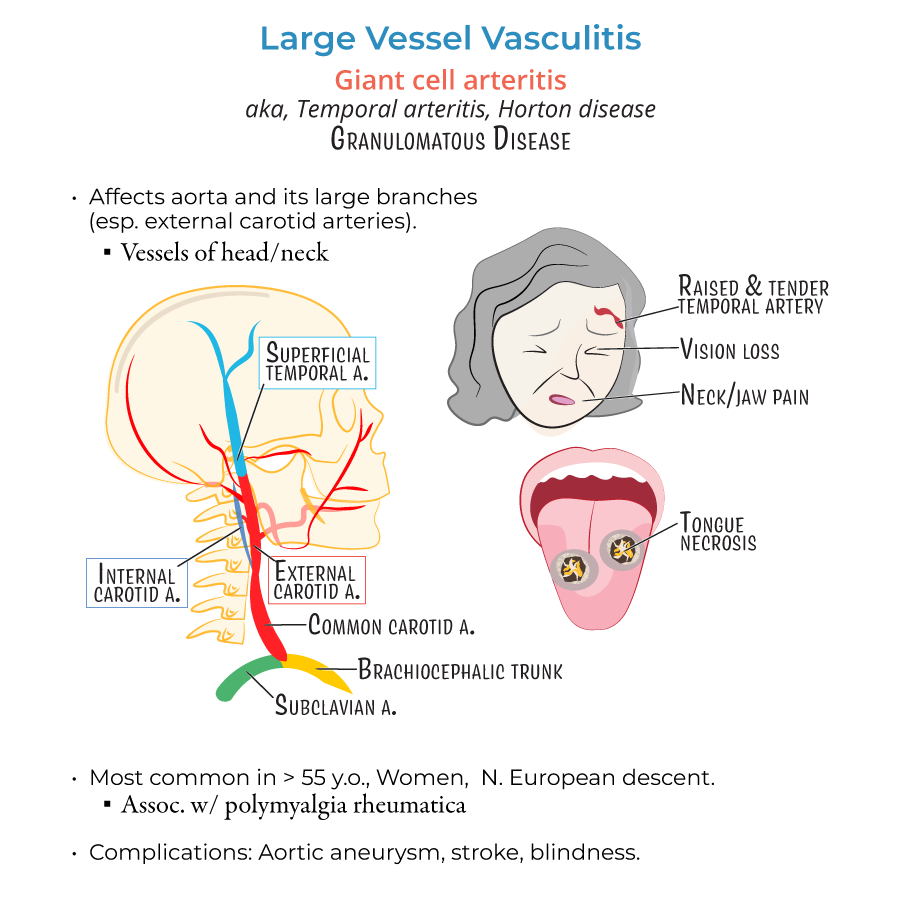
1. Giant Cell Arteritis (GCA) is a medical emergency due to the risk of permanent blindness.
2. GCA typically affects women over 50 years old, especially those of Northern European descent.
3. Key symptoms of GCA:
- New-onset, severe headache (especially temporal)
- Jaw pain with chewing (jaw claudication)
- Blurred vision or sudden vision loss
- Scalp tenderness
Core Interventions
6. Administer corticosteroids as ordered to prevent vision loss.
7. Monitor for improvement in symptoms and for side effects of steroids (e.g., blood sugar elevation, infection risk).
8. For GCA with vision symptoms, anticipate IV methylprednisolone administration first.
9. Temporal artery biopsy is the confirmatory test but is not a reason to delay starting treatment.
Takayasu Arteritis Recognition
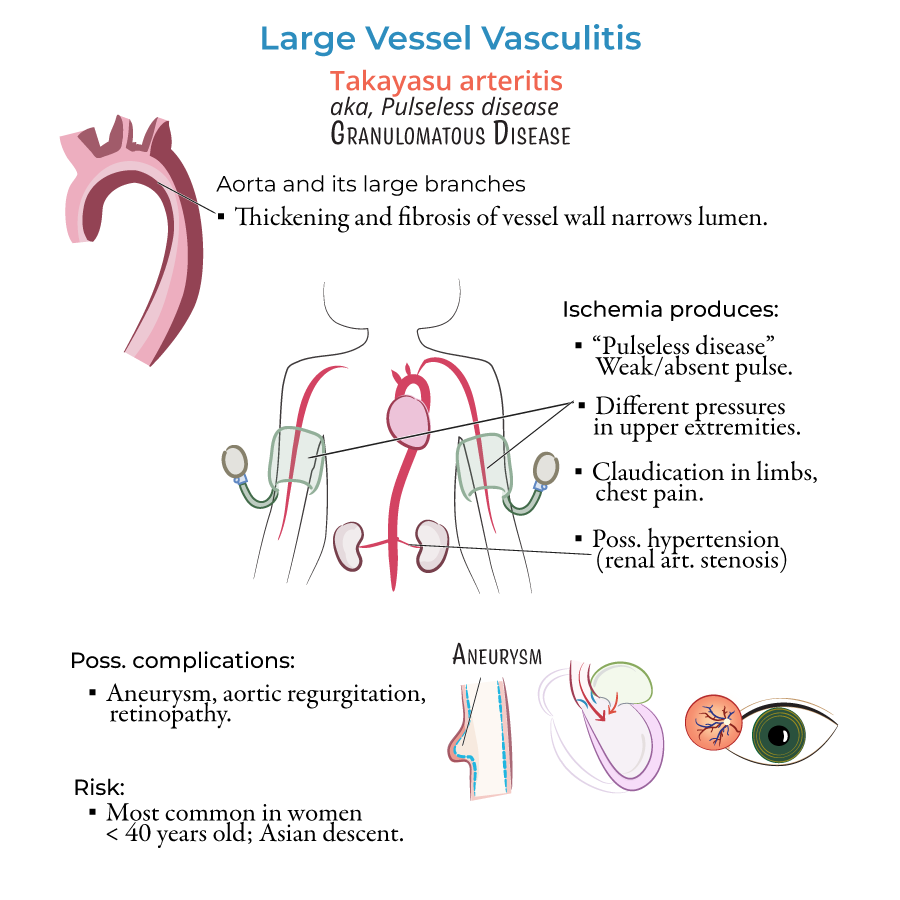
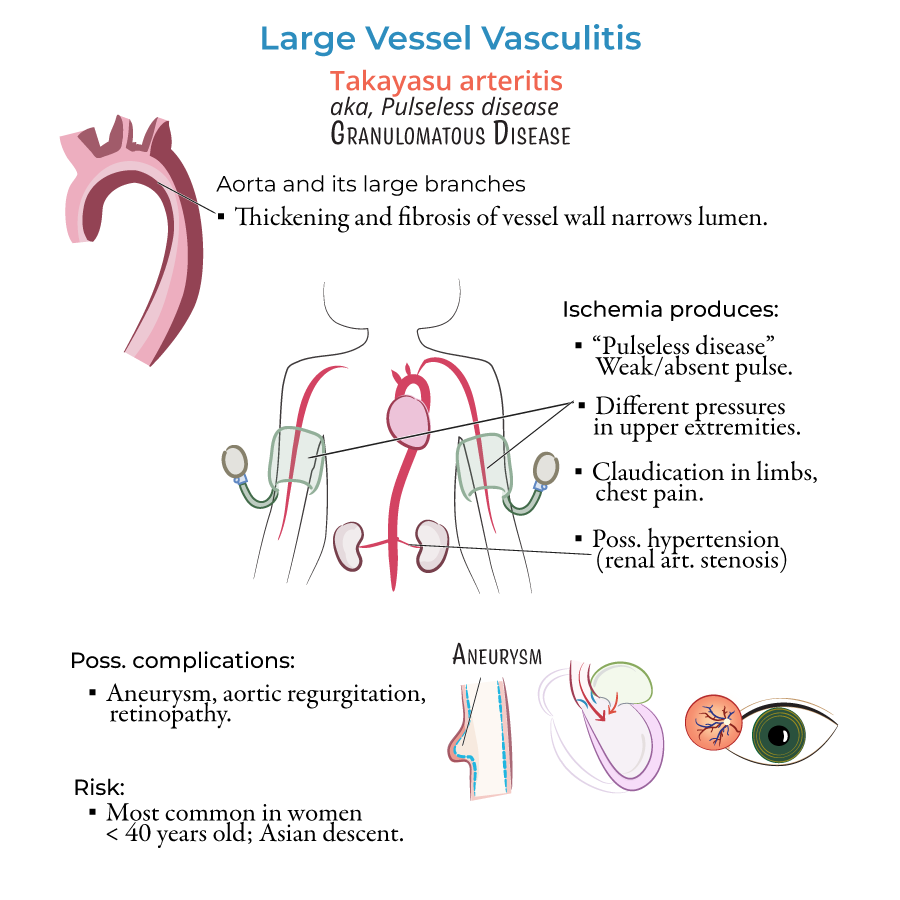
10. Takayasu arteritis mainly affects young women (<40 years), often of Asian descent.
11. Clinical signs:
- Weak or absent pulses in upper limbs
- Different blood pressure readings between arms
- Arm or leg pain during activity (claudication)
- Bruits (swishing sounds) heard over arteries
General Management
14. Corticosteroids are the first-line treatment for both GCA and Takayasu.
15. Support medication adherence and educate on steroid side effects (e.g., infection risk, osteoporosis, hyperglycemia).
- --
HIGH YIELD
Patient Teaching and Monitoring
1. Teach patients on long-term steroids to report signs of infection and blood sugar elevation.
2. Advise use of calcium and vitamin D supplementation to prevent bone loss.
3. Teach patients that symptoms like new headache, visual changes, limb weakness, or numbness should be reported immediately.
4. Teach about the importance of follow-up appointments and regular monitoring of ESR/CRP to assess inflammation.
5. Encourage adherence to prescribed corticosteroids even if symptoms improve.
Recognizing Complications
6. GCA can cause:
- Permanent blindness (from ophthalmic artery occlusion)
- Stroke
- Aortic aneurysm
- Severe hypertension (renal artery stenosis)
- Aortic regurgitation
- Limb ischemia
- Regular neurovascular checks (pulses, capillary refill)
- Monitoring blood pressure in both arms
- Assessing for changes in vision, pain, or functional ability
- --
Beyond the Tutorial
Emergency Management Strategies
1. If a patient presents with vision changes and temporal tenderness, the first nursing action is to initiate provider contact and prepare for corticosteroid administration.
2. If a patient has signs of limb ischemia (cold limb, absent pulse), notify the healthcare provider immediately as emergent imaging and treatment may be needed.
3. Educate patients about steroid-sparing medications (e.g., methotrexate) if they are used long-term to minimize corticosteroid exposure.
4. Collaborate with other professionals (e.g., pharmacists, dietitians, ophthalmologists) to manage complications from long-term steroid use.
Priority and Safety Practice
5. In the NCLEX format, prioritize patients with:
- New vision loss
- Neurological deficits
- Absent pulses
- Severe or sudden blood pressure changes
