NCLEX - Supraventricular & Ventricular Arrhythmias
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Supraventricular & Ventricular Arrhythmias tutorial, as well as points of interest that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
- --
VITAL FOR NCLEX
Assessment Findings
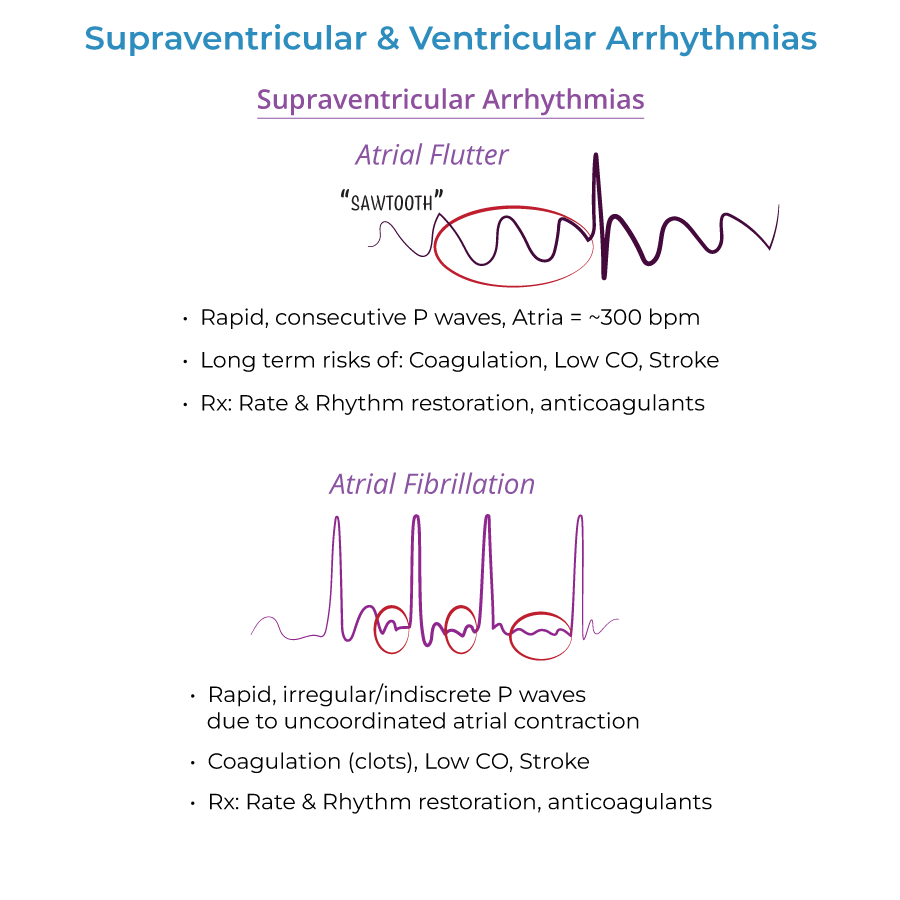
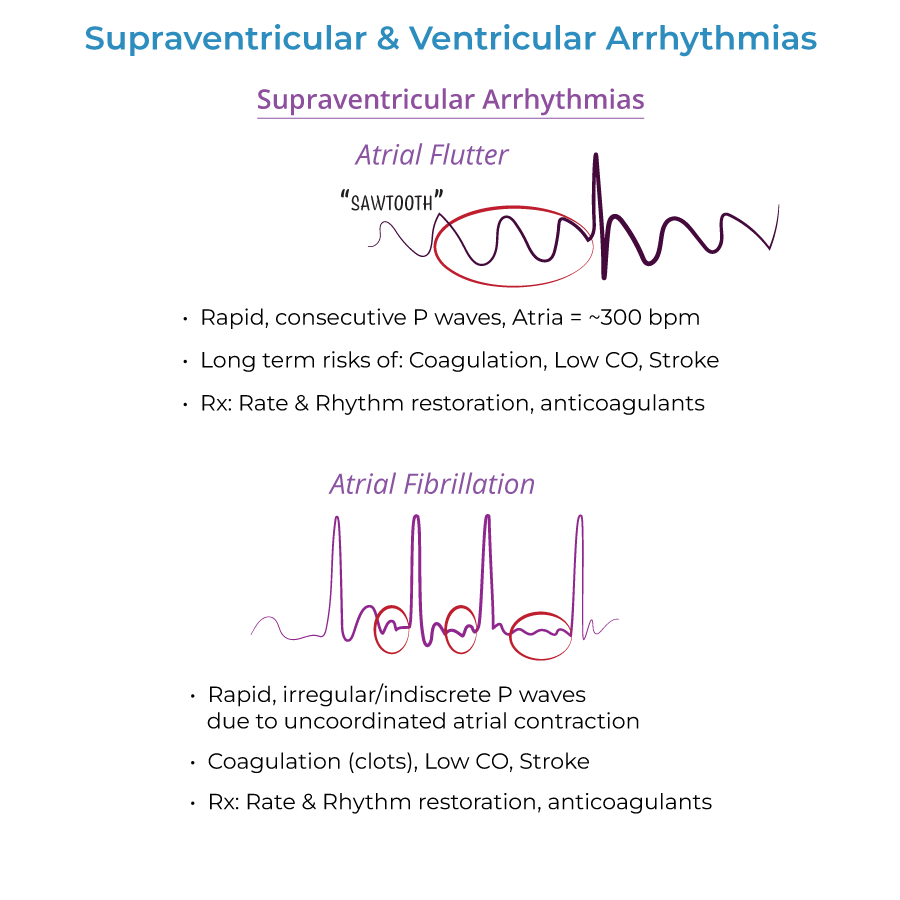
1. Atrial Flutter: Rapid, regular P waves give ECG "sawtooth" appearance. Atria beat ~300 beats/minute. Only ½ - 1/3 of the electrical impulses make it through the AV node.
2. Atrial Fibrillation: Rapid, irregular and indiscrete P waves on ECG. Atria do not contract in coordinated fashion, but send fast and irregular signals to ventricles increase heart rate.
3. Ventricular Tachycardia: 3+ consecutive beats 120+ beats/minute; abnormal ventricular automacy.
4. Cardiac Arrest Rhythms: Asystole often described as "Flat-lining" on ECG. Pulseless Electrical Activity shows cardiac electrical activity is present, but no pulse is present due to inactivity of cardiac muscle.
Patient Symptoms
1. Atrial Flutter: May be none. Or, may cause palpitations, and reduced CO, difficulty breathing, weakness, chest discomfort, syncope.
2. Atrial Fibrillation: May be asymptomatic. Or, may experience lack of energy, fast, irregular pulse, difficulty breathing, palpitations, chest discomfort, dizziness.
3. Ventricular Tachycardia: If sustained, palpitations, difficulty breathing, chest pain, dizziness, fainting, death.
4. Torsades de Pointes: Recurrent palpitations, dizziness, fainting, difficulty breathing.
Priority Interventions
1. Atrial Flutter/Fibrillation: Rate control with beta-blockers, calcium channel blockers (verapamil, diltiazem). Anticoagulants (warfarin) are used to prevent thromboembolism.
2. Ventricular Tachycardia: Cardioversion, antiarrhythmic drugs, defibrillator implant.
3. Torsades de Pointes: Magnesium.
4. Ventricular Fibrillation: CPR & Defibrillation.
- --
HIGH YIELD
Medication Knowledge
1. Atrial Arrhythmia Medications: Rate control with beta blockers and nondihydropyridine calcium channel blockers. Rhythm control with antiarrhythmics.
2. Anticoagulation: Required before cardioversion therapy to prevent thromboembolism in atrial fibrillation.
3. WPW Medication Contraindications: Beware digoxin/nondihydropyridine calcium channel blockers to WPW patients, as they may trigger ventricular fibrillation (fatal).
4. Medication Triggers: Torsades de Pointes can be triggered by antiarrhythmics, tricyclic antidepressants, anti-histamines when taken with erythromycin.
Risk Factors
1. Atrial Flutter: Commonly occurs in healthy people, but risk increases with other cardiac conditions, binge alcohol consumption, diabetes.
2. Atrial Fibrillation: Other cardiac problems, hyperthyroidism, obesity, diabetes, lung disease, binge alcohol consumption.
3. Premature Beats: Stress, caffeine, alcohol, hypoxia, electrolyte imbalances. Heart disease, pulmonary disease, and scarring.
4. Ventricular Arrhythmias: Heart disease, electrolyte imbalances (hypocalcemia, hypokalemia), medications.
Diagnostic Testing
1. Atrial Fibrillation: Echocardiography to check for structural defects, thyroid function tests.
2. WPW Syndrome: Short PR interval and positive delta wave at beginning of broad QRS complex; delta wave reflects early depolarization.
3. Long QT Syndrome: Long QT interval on ECG, reflects defective ion channels.
4. Torsades de Pointes: Rapid, irregular QRS complexes "spiral" around baseline, as ventricular rate varies from cycle to cycle.
Complications
1. Atrial Flutter: When coupled with other cardiac complications, can lead to stroke, makes heart work more difficult, ventricular weakening, and coagulation is more likely.
2. Atrial Fibrillation: Stroke, systemic emboli.
3. Ventricular Tachycardia: Can lead to heart failure, unconsciousness, sudden death by cardiac arrest.
4. Long QT Syndrome: Prone to torsades de pointes, which can cause syncope, ventricular fibrillation, and sudden death.
- --
Beyond the Tutorial
Nursing Care Priorities
1. Continuous Monitoring: Importance of continuous cardiac monitoring for patients with known or suspected arrhythmias.
2. Emergency Response: Protocols for responding to sudden deterioration in patients with arrhythmias.
3. Patient Positioning: Proper positioning during episodes of arrhythmias to maximize cardiac output.
4. Oxygen Therapy: Indications and administration for patients experiencing arrhythmias.
Patient Education
1. Medication Adherence: Teaching points for antiarrhythmic and anticoagulant therapies.
2. Symptom Recognition: Educating patients on when to seek medical attention for arrhythmia symptoms.
3. Lifestyle Modifications: Recommendations regarding caffeine, alcohol, stress reduction, and other triggers.
4. Activity Restrictions: Guidelines for physical activity based on arrhythmia type and severity.
Special Considerations
1. Elderly Patients: Modifications to assessment and interventions for geriatric populations.
2. Implanted Devices: Basic nursing care for patients with pacemakers and ICDs.
3. Post-Procedure Care: Nursing interventions following cardioversion or ablation procedures.
4. Electrolyte Management: Monitoring and replacement strategies for patients at risk for arrhythmias.
Nursing Assessments
1. Vital Signs Patterns: Recognizing patterns in vital signs that may indicate specific arrhythmias.
2. Perfusion Assessment: Techniques for evaluating end-organ perfusion during arrhythmias.
3. Mental Status Changes: Association between arrhythmias and alterations in consciousness.
4. Fluid Status: Connection between volume status and arrhythmia risk or management.
