NCLEX - Pulmonary Embolism and Deep Vein Thrombosis
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX (National Council Licensure Examination) from the Pulmonary Embolism & Deep Vein Thrombosis tutorial, focusing on the nursing process, patient care, and clinical judgment essential for licensure. See the tutorial notes for further details and relevant links.
 3. Nonthrombotic Sources: PE can also result from air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors.
4. Complications: Pulmonary hypertension, right heart failure, and pulmonary infarction.
5. Mortality Significance: PE is a leading cause of cardiovascular-related death.
3. Nonthrombotic Sources: PE can also result from air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors.
4. Complications: Pulmonary hypertension, right heart failure, and pulmonary infarction.
5. Mortality Significance: PE is a leading cause of cardiovascular-related death.
 2. Combined Risk Factors: Patients with multiple predisposing factors (e.g., pregnant women on bed rest) have higher risk.
3. Preventable Factors: Many risk factors are modifiable through nursing interventions.
4. Prophylaxis Candidates: Recognition of high-risk patients who need preventive measures.
5. Assessment Focus: Comprehensive history and physical exam targeted at identifying risk factors.
Below is information not explicitly contained within the tutorial but important for NCLEX preparation.
2. Combined Risk Factors: Patients with multiple predisposing factors (e.g., pregnant women on bed rest) have higher risk.
3. Preventable Factors: Many risk factors are modifiable through nursing interventions.
4. Prophylaxis Candidates: Recognition of high-risk patients who need preventive measures.
5. Assessment Focus: Comprehensive history and physical exam targeted at identifying risk factors.
Below is information not explicitly contained within the tutorial but important for NCLEX preparation.
- --
VITAL FOR NCLEX
Understanding Venous Thromboembolism
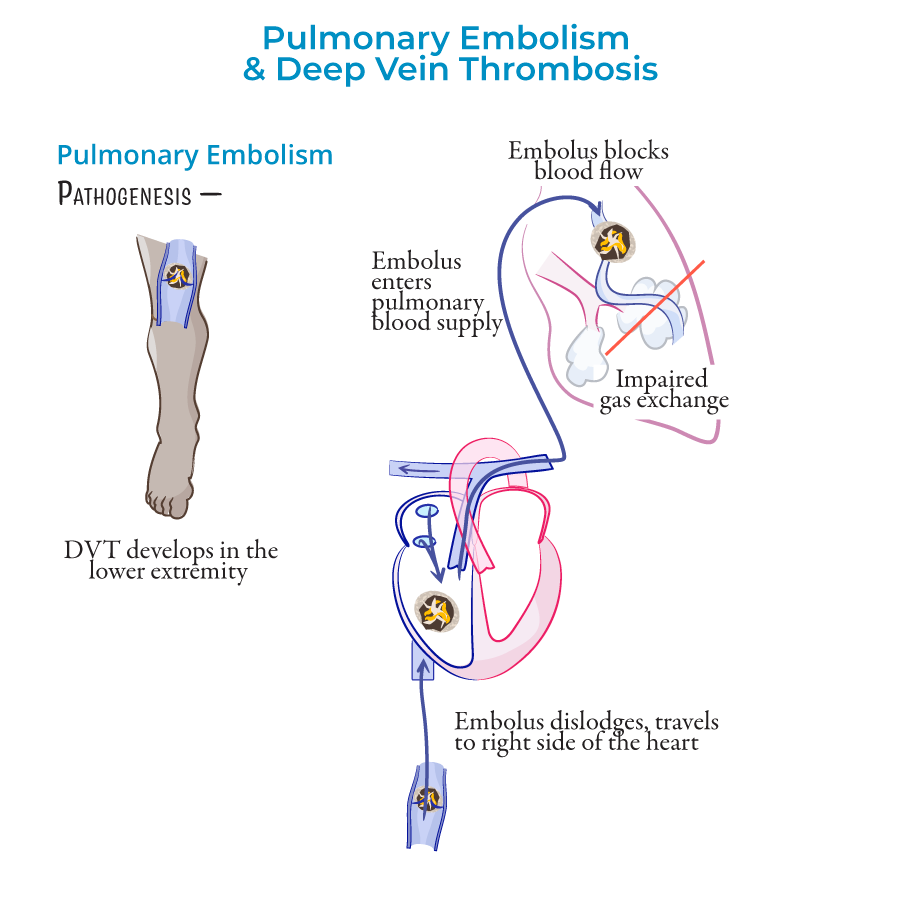
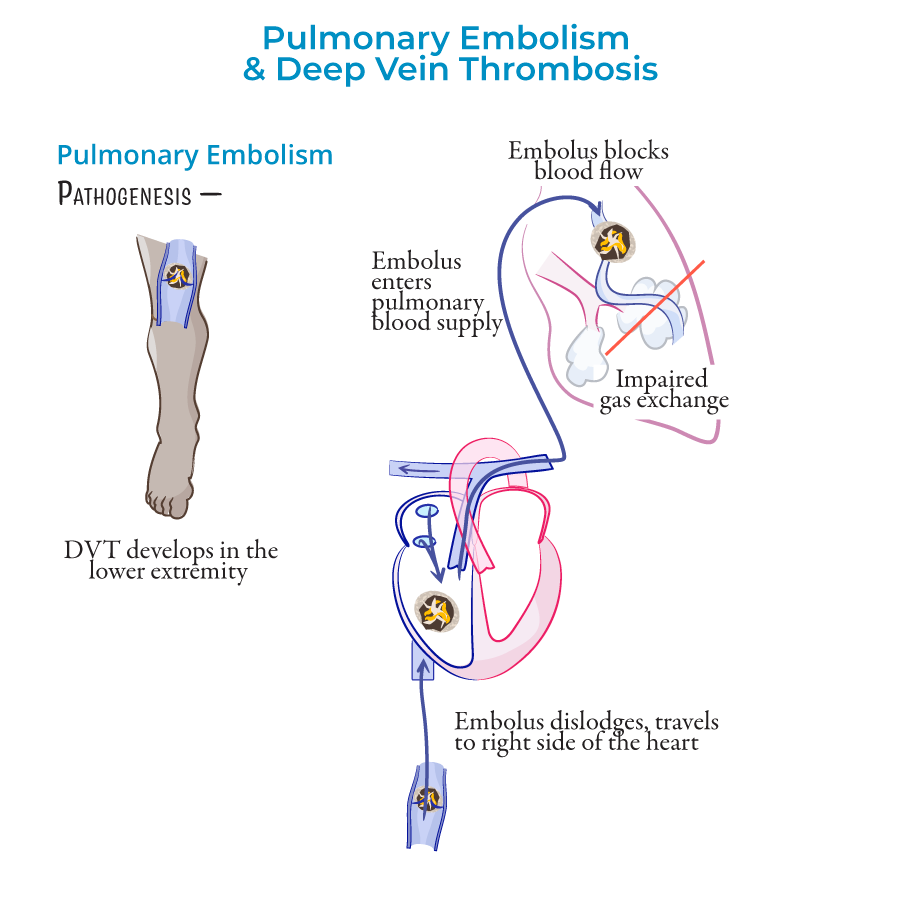
1. Definition & Relationship: Pulmonary embolism (PE) occurs when pulmonary arteries are obstructed, most commonly by emboli from deep veins of thighs/pelvis; deep vein thrombosis (DVT) and PE together are called venous thromboembolism.
2. Pathophysiology: Clot forms in deep vein → fragment breaks off → travels through IVC → right heart → pulmonary arteries → obstructs blood flow → impaired gas exchange.
 3. Nonthrombotic Sources: PE can also result from air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors.
4. Complications: Pulmonary hypertension, right heart failure, and pulmonary infarction.
5. Mortality Significance: PE is a leading cause of cardiovascular-related death.
3. Nonthrombotic Sources: PE can also result from air, fat, amniotic fluid, bacterial (septic), foreign bodies, and tumors.
4. Complications: Pulmonary hypertension, right heart failure, and pulmonary infarction.
5. Mortality Significance: PE is a leading cause of cardiovascular-related death.
Risk Factor Assessment
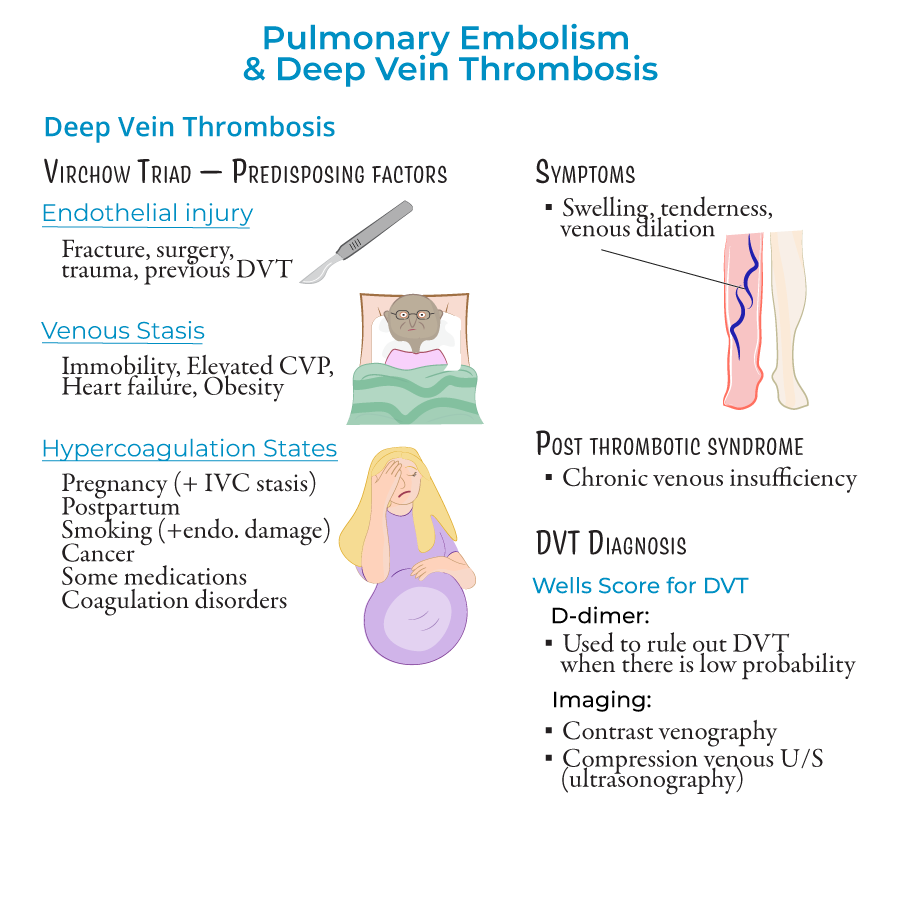
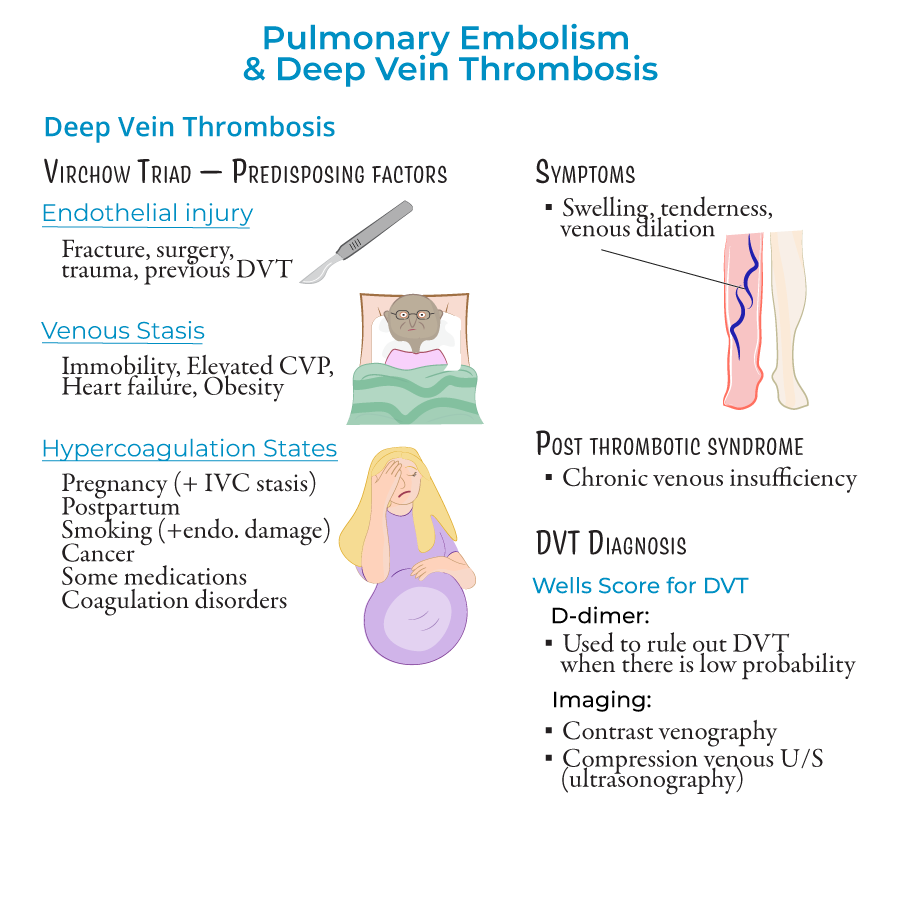
1. Virchow's Triad: Three factors predisposing to thrombosis:
- Endothelial injury: Fracture, surgery, trauma, previous DVT; triggers clotting cascade
- Venous stasis: Immobility, elevated central venous pressure, heart failure, obesity
- Hypercoagulable states: Pregnancy, postpartum period, smoking, cancer, hormonal contraceptives/therapies, coagulation disorders (Factor V Leiden)
 2. Combined Risk Factors: Patients with multiple predisposing factors (e.g., pregnant women on bed rest) have higher risk.
3. Preventable Factors: Many risk factors are modifiable through nursing interventions.
4. Prophylaxis Candidates: Recognition of high-risk patients who need preventive measures.
5. Assessment Focus: Comprehensive history and physical exam targeted at identifying risk factors.
2. Combined Risk Factors: Patients with multiple predisposing factors (e.g., pregnant women on bed rest) have higher risk.
3. Preventable Factors: Many risk factors are modifiable through nursing interventions.
4. Prophylaxis Candidates: Recognition of high-risk patients who need preventive measures.
5. Assessment Focus: Comprehensive history and physical exam targeted at identifying risk factors.
Clinical Manifestations & Assessment
1. DVT Presentation: When symptomatic, presents with unilateral leg swelling, tenderness, and signs of venous dilation; can also occur in upper body (less common).
2. PE Symptoms & Signs:
- Dyspnea and tachypnea (rapid breathing)
- Chest pain
- Hypoxemia and ventilation-perfusion mismatch
- Tachycardia and potential right heart failure
- Altered mental state, especially in elderly patients
Diagnostic Tests & Procedures
1. Clinical Probability Tools:
- Wells Score for DVT: Based on swelling, edema, alternative diagnosis likelihood
- Wells Score for PE: Score ≥4 indicates PE likely; <2 low probability, 2-6 moderate, >6 high probability
- D-dimer: >500 ng/mL suggests possible PE or DVT, requiring further testing
- Arterial blood gases: May show hypoxemia and respiratory alkalosis
- For PE: CT angiography, ventilation-perfusion scan, chest X-ray
- For DVT: Venous ultrasonography with compression, contrast venography
Nursing Interventions & Treatment
1. Supportive Care:
- Oxygen administration when saturation is less than 90%
- IV fluid management with saline
- Monitoring for and managing hemodynamic instability
- Anticoagulants: Heparin/enoxaparin or fondaparinux (short-term); warfarin (long-term)
- Monitoring for side effects, especially bleeding and heparin-induced thrombocytopenia
- Application and monitoring of sequential compression devices (SCDs)
- Administration of prophylactic anticoagulants (low-dose enoxaparin or heparin)
Patient Education & Discharge Planning
1. Risk Factor Modification: Teaching about modifiable risk factors and prevention strategies.
2. Medication Teaching: Anticoagulant purpose, administration, side effects, and monitoring.
3. Symptom Recognition: Signs of recurrent DVT, PE, or bleeding complications.
4. Activity Guidelines: Appropriate exercise and mobility recommendations.
5. Follow-up Care: Importance of continued medical monitoring and adherence to treatment plan.
- --
HIGH YIELD
Assessment Priorities
1. Respiratory Status: Monitor for dyspnea, tachypnea, oxygen saturation, and respiratory effort.
2. Cardiovascular Status: Assess for tachycardia, hypotension, and signs of right heart failure.
3. Pain Assessment: Evaluate chest pain (PE) or extremity pain (DVT) using appropriate pain scales.
4. Neurovascular Assessment: For DVT, assess affected extremity for pulses, color, temperature, sensation.
5. Mental Status: Especially important in elderly patients who may present with altered mental state.
Diagnostic Test Preparation & Monitoring
1. D-dimer Testing: Proper specimen collection and patient education about purpose.
2. CT Angiography: Assessment for contrast allergies, renal function; hydration before and after procedure.
3. Ventilation-Perfusion Scan: Patient preparation and positioning during procedure.
4. Ultrasonography: Proper positioning and support of extremity during examination.
5. ECG Monitoring: Recognition of tachycardia and S1Q3T3 pattern relevant to PE.
Anticoagulation Nursing Care
1. Heparin Administration: Proper subcutaneous injection technique, site rotation, monitoring for bleeding.
2. Enoxaparin Considerations: Weight-based dosing, renal function assessment, injection technique.
3. Warfarin Management: Food and drug interactions, INR monitoring, bleeding precautions.
4. Bleeding Precautions: Minimizing fall risk, using soft toothbrush, electric razor, avoiding IM injections.
5. Monitoring Parameters: Signs of bleeding, platelet counts (for heparin-induced thrombocytopenia), therapeutic levels.
DVT Prevention Interventions
1. Sequential Compression Devices (SCDs): Proper application, assessment of skin integrity, ensuring appropriate use.
2. Early Mobilization: Safe ambulation techniques for hospitalized patients.
3. Hydration Maintenance: Encouraging adequate fluid intake unless contraindicated.
4. Position Changes: For immobile patients, frequent repositioning to prevent stasis.
5. Patient Education: Teaching about leg exercises, avoiding prolonged sitting, and recognizing symptoms.
Complication Recognition & Management
1. Pulmonary Infarction: Monitoring for Hampton Hump on chest X-ray, indicating tissue ischemia typically in lower lobes.
2. Right Heart Failure: Assessing for jugular vein distention, peripheral edema, liver congestion.
3. Bleeding Complications: Monitoring for overt bleeding and signs of occult bleeding (tachycardia, hypotension, decreasing hemoglobin).
4. Heparin-Induced Thrombocytopenia: Regular platelet count monitoring, awareness of paradoxical clotting risk.
5. Post-thrombotic Syndrome: Long-term complication of DVT causing chronic venous insufficiency due to valve damage.
- --
Beyond the Tutorial
Nursing Process Application
1. Assessment: Focused assessment techniques for DVT and PE risk factors and symptoms.
2. Nursing Diagnoses: Impaired Gas Exchange, Ineffective Tissue Perfusion, Acute Pain, Activity Intolerance, Risk for Bleeding.
3. Planning: Prioritizing interventions based on patient status and risk level.
4. Implementation: Evidence-based nursing interventions for prevention and management.
5. Evaluation: Expected outcomes and reassessment criteria.
Pharmacology for Nursing Practice
1. Unfractionated Heparin: Mechanism, administration routes, monitoring (aPTT), protamine reversal.
2. Low Molecular Weight Heparins: Dosing considerations, reduced monitoring requirements, longer half-life.
3. Direct Oral Anticoagulants: Administration considerations, lack of routine monitoring, reversal agents.
4. Thrombolytics: Administration protocols, absolute and relative contraindications, monitoring during therapy.
5. Analgesics: Appropriate pain management strategies that minimize bleeding risk.
Priority Nursing Interventions
1. Oxygen Therapy Management: Appropriate delivery methods and flow rates based on oxygen saturation.
2. Position to Promote Oxygenation: Semi-Fowler's or high Fowler's position to reduce work of breathing.
3. Emergency Response to Massive PE: Recognition and initial management of shock or respiratory failure.
4. Psychosocial Support: Addressing anxiety related to diagnosis and treatment.
5. Activity Progression: Gradual resumption of activities following established protocols.
Patient Teaching Priorities
1. Signs and Symptoms Requiring Medical Attention: Increased shortness of breath, chest pain, increased extremity swelling.
2. Anticoagulant Safety: Medication adherence, bleeding precautions, food and drug interactions.
3. Long-Term Prevention Strategies: Travel precautions, compression stockings, hydration, mobility.
4. Pregnancy Considerations: Special precautions for pregnant women with history of VTE.
5. Self-Monitoring Skills: Teaching pulse and respiratory self-assessment, weight monitoring.
Special Population Considerations
1. Geriatric Patients: Recognition of atypical presentations, fall precautions with anticoagulation.
2. Pregnant Women: Modifications in assessment and treatment approaches.
3. Post-Surgical Patients: Enhanced monitoring and prophylaxis protocols.
4. Oncology Patients: Increased vigilance due to hypercoagulable state associated with cancer.
5. Chronically Immobile Patients: Intensified preventive strategies and routine assessment.
