NCLEX - Nausea, Vomiting, Diarrhea
Start your One-Week Free Trial
Already subscribed? Log in »
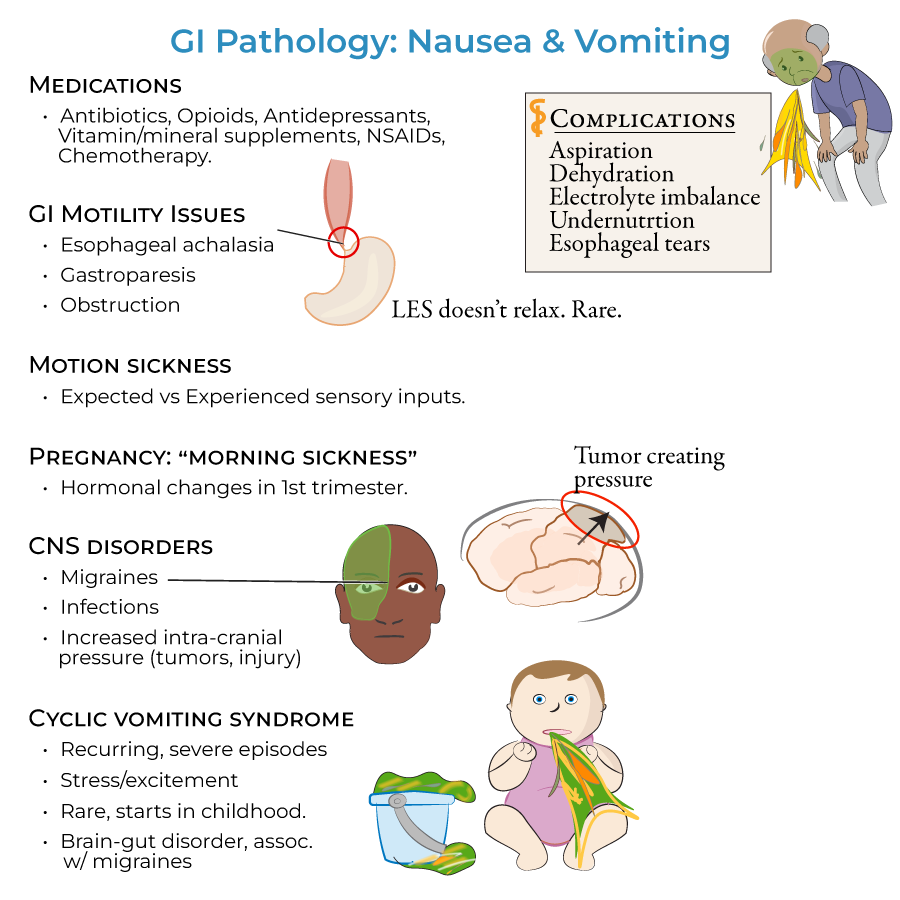
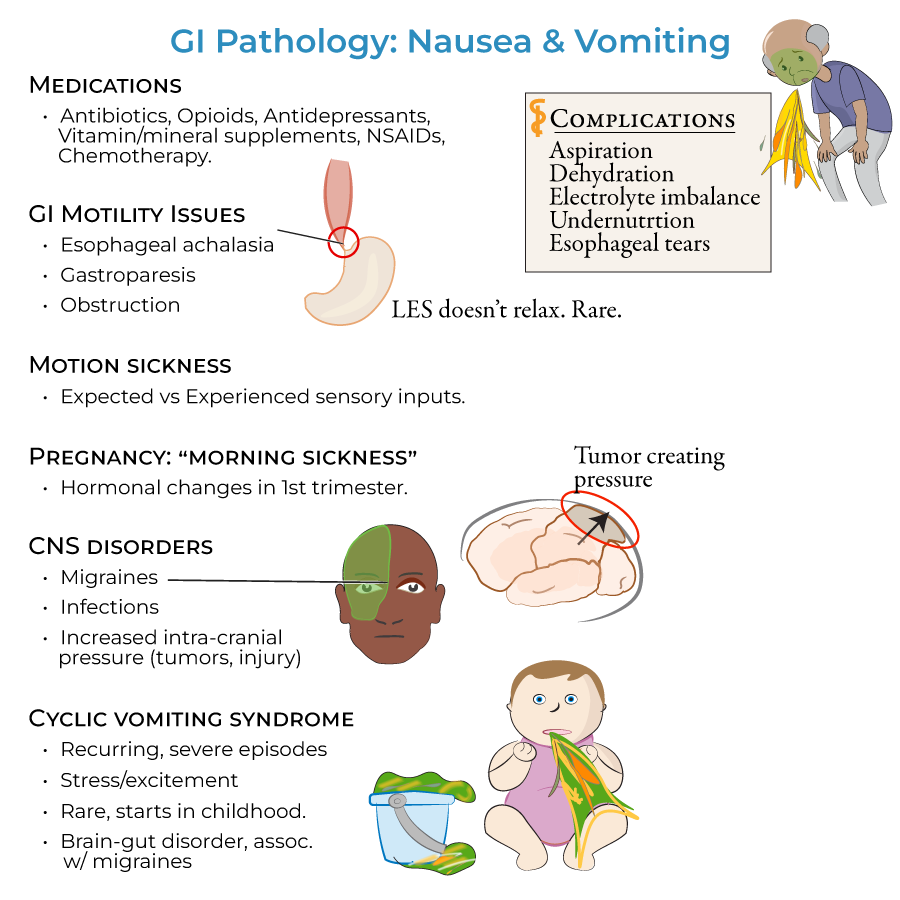
Here are key facts for NCLEX from the Nausea, Vomiting, Diarrhea tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes* for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for NCLEX.
Below is information not explicitly contained within the tutorial but important for NCLEX.
- --
VITAL FOR NCLEX
Assessment
1. Vomiting definition: Forceful eviction of the stomach contents caused by contractions of the GI tract and muscles of the thorax
2. Regurgitation definition: When food is ejected from the esophagus
3. Complication assessment: Monitor for vomiting complications (aspiration, dehydration, electrolyte imbalance, undernutrition, esophageal tears) and diarrhea complications (malabsorption, dehydration, electrolyte imbalances)
Common Etiologies - Nausea and Vomiting
1. Medication-induced: Antibiotics, opioids, antidepressants, vitamins and mineral supplements, NSAIDs, chemotherapy
2. GI motility disorders: Damaged nerves or mechanical obstruction preventing normal passage of food
3. Mechanical obstructions: Adhesions, volvulus, foreign bodies, hernias, tumors
4. Systemic conditions: Early pregnancy hormonal changes, motion sickness, central nervous disorders (migraines, infections, increased intra-cranial pressure)
Common Etiologies - Diarrhea
1. Malabsorptive disorders: Lactose intolerance, celiac disease
2. Inflammatory conditions: Inflammatory bowel disease (Crohn's disease, ulcerative colitis), microscopic colitis
3. Gastroenteritis: Infections from norovirus, rotavirus, E. coli, Salmonella, Shigella, and Campylobacter
Patient Monitoring
1. Fluid status: Assess for signs of dehydration from excessive fluid loss
2. Nutritional status: Monitor for undernutrition in prolonged vomiting or diarrhea
3. Electrolyte balance: Evaluate for imbalances resulting from fluid losses
- --
HIGH YIELD
Clinical Presentations - Key Assessment Findings
1. Esophageal achalasia: Patients present with heartburn, chest pain, and regurgitation due to sustained lower esophageal sphincter contraction
2. Gastroparesis: Patients feel full after eating small amounts of food and experience heartburn and vomiting due to vagus nerve damage
3. Steatorrhea: Characteristic oily, foul smelling stools that are yellowish and float due to high fat content in pancreatic insufficiency
Special Patient Populations
1. Pregnancy: Nausea and vomiting can occur any time of day during first trimester due to hormonal changes
2. Pediatric patients: Cyclical vomiting syndrome often begins in childhood with recurring episodes triggered by stress and excitement
3. Patients with neuroendocrine tumors: Monitor for carcinoid syndrome with watery, loose stools, flushing, wheezing, and valvular heart disease
Nursing Implications for Specific Conditions
1. Inflammatory bowel disease: Differentiate between Crohn's disease (mucous diarrhea) and ulcerative colitis (bloody diarrhea)
2. Intestinal ischemia: Recognize the triad of nausea, vomiting and bloody diarrhea when mesenteric arteries become blocked
3. Functional disorders: Understand irritable bowel syndrome results from disordered brain-gut communication
Complication Prevention
1. Aspiration risk: Position patients properly during episodes of vomiting
2. Skin integrity: Provide perineal care for patients with diarrhea to prevent skin breakdown
3. Patient education: Teach signs of dehydration and when to seek medical attention
- --
Beyond the Tutorial
Nursing Process Application
1. Assessment: Focused history taking for patterns of nausea, vomiting, and diarrhea
2. Nursing diagnoses: Risk for fluid volume deficit, imbalanced nutrition, and impaired skin integrity
3. Planning: Setting measurable goals for hydration status and symptom management
Nursing Interventions
1. Fluid management: IV therapy administration and oral rehydration techniques
2. Medication administration: Proper timing and administration of antiemetics and antidiarrheals
3. Comfort measures: Non-pharmacological approaches to symptom management
Patient Education
1. Dietary modifications: Foods to avoid during acute episodes
2. Home care instructions: When and how to use OTC medications appropriately
3. Prevention strategies: Hand hygiene and food safety to prevent infectious causes
Documentation and Communication
1. Intake and output: Accurate measurement and recording
2. Stool characteristics: Proper description and documentation
3. Interdisciplinary communication: Effective reporting of significant changes in patient condition
