NCLEX - Myocardial Infarction Symptoms, Diagnosis, & Treatments
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX (National Council Licensure Examination) from the Myocardial Infarctions: Diagnosis & Treatment tutorial, focusing on the nursing process, patient care, and clinical judgment essential for licensure. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for NCLEX preparation.
Below is information not explicitly contained within the tutorial but important for NCLEX preparation.
- --
VITAL FOR NCLEX
Understanding Myocardial Infarction
1. Definition: Myocardial infarction is defined as myocardial injury with ischemia.
2. Epidemiology: Incidence is declining in high-income countries but rising in middle- and low-income countries.
3. Population differences: Within the United States, MI incidence after age 35, from highest to lowest: Black males > Black females > White males > White females.
4. Gender differences: First MI occurs approximately 10 years earlier in men than women.
5. Mortality pattern: Despite overall declining rates, mortality remains higher in women than men, especially for young and/or minority women.
Risk Factors & Prevention
1. Major modifiable risk factors:
- Dyslipidemia
- Diabetes mellitus
- Hypertension
- Smoking (including e-cigarettes)
- Obesity
- Psychosocial stress
- Alcohol consumption
- Poor diet (low in fruits and vegetables)
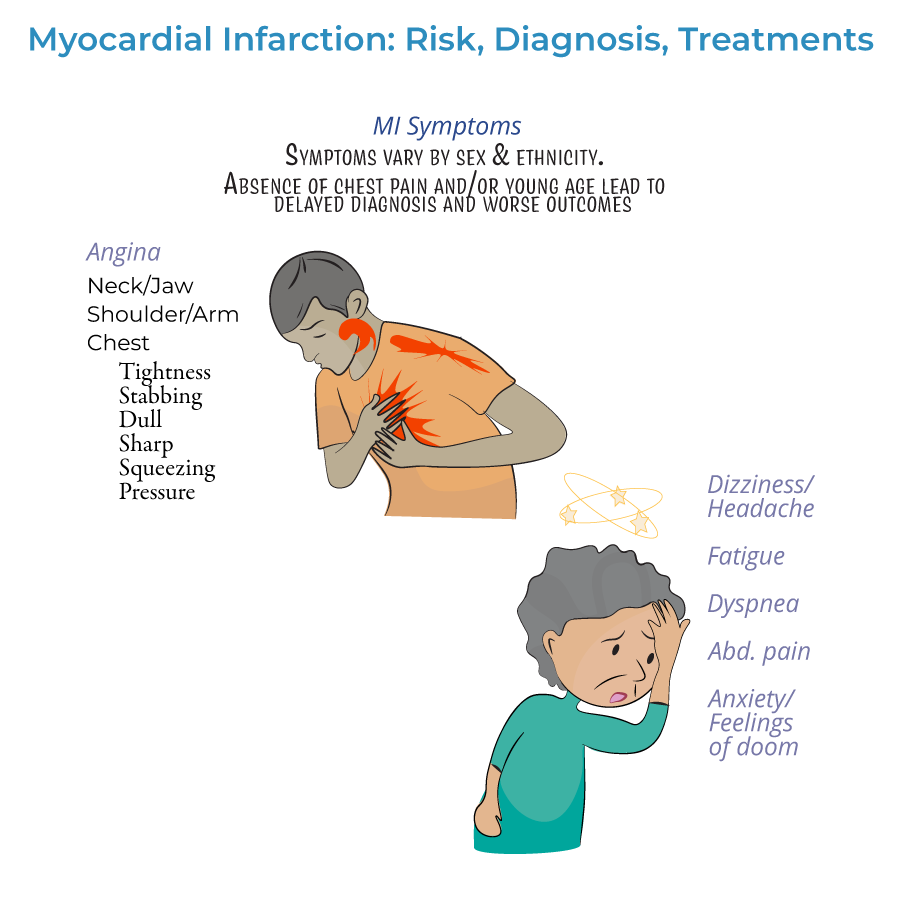
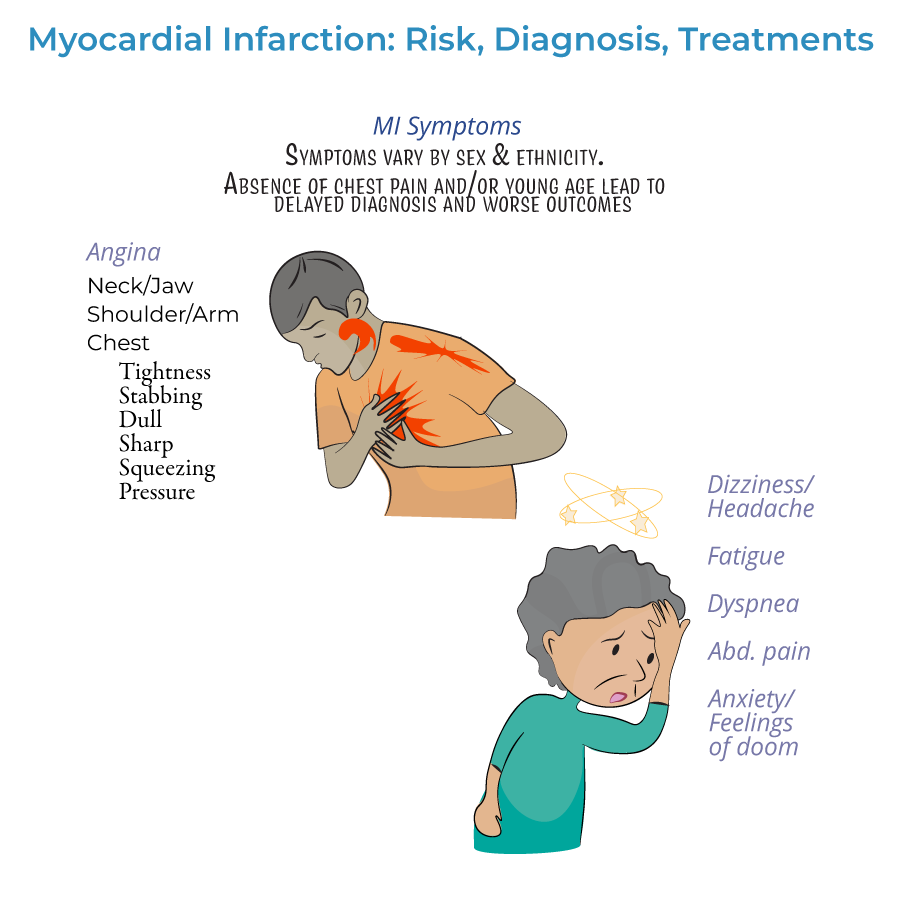
Assessment & Recognition
1. Presentation timeline:
- Prodromal symptoms: Days, weeks, or months prior to the heart attack
- Acute symptoms: Experienced at the time of the event
- Silent MI: No noticeable symptoms
- Gastrointestinal issues (nausea, vomiting, indigestion)
- Extreme fatigue, exhaustion, or sleep disturbances
- Headaches, dizziness, lightheadedness
- Shortness of breath (dyspnea)
- Anxiety or sense of impending doom
Diagnostic Process
1. ECG timing: Should be obtained as soon as possible when MI is suspected and repeated frequently to observe evolution.
2. ECG classification: Distinguishes between ST-segment elevated (STEMI) or Non-ST elevated (NSTEMI) myocardial infarctions.
3. Q-wave significance: May indicate size/location of current MI, or may indicate a prior MI.
4. Biomarker assessment:
- Cardiac troponin is key to diagnosis
- Helps distinguish NSTEMI (elevated troponin) from unstable angina (normal troponin)
- Both cardiac troponin I and CK-MB peak within 24 hours of MI
Nursing Interventions & Treatment
1. Time-sensitive care: Treatment should begin as soon as possible to reduce myocardial necrosis.
2. Immediate interventions:
- Oxygen administration when oxygen saturation is less than 90%
- Aspirin administration for antiplatelet effects
- Nitrates for chest pain (morphine if nitrates ineffective)
- Antiplatelets (aspirin, clopidogrel, others)
- Anticoagulation drugs (unfractionated or low molecular weight heparin)
- Beta-blockers or calcium-channel blockers
- Statins
- ACE-inhibitors
- --
HIGH YIELD
Clinical Recognition & Patient Assessment
1. Atypical presentation recognition: Many patients, especially women, elderly, and diabetics, present without classic chest pain.
2. Prodromal assessment: Ask about symptoms in days/weeks before presentation (fatigue, sleep changes, vague discomfort).
3. Comprehensive symptom evaluation: Assess for gastrointestinal, neurological, and psychological symptoms that may mask cardiac origin.
4. Pain assessment: Document location, radiation, quality, severity, duration, and alleviating/aggravating factors.
5. Risk factor identification: Evaluate presence of modifiable and non-modifiable risk factors to guide prevention strategies.
ECG Interpretation Essentials for Nurses
1. STEMI recognition: ST-segment elevation indicates need for immediate reperfusion.
2. NSTEMI patterns: ST depression or T-wave inversions may be present.
3. Lead groupings and significance:
- Lateral infarction: Leads I and aVL; left circumflex artery
- Apical infarction: Leads V5 and V6; left circumflex or right coronary arteries
- Anterior infarction: Leads V3 and V4; left anterior descending artery
- Anteroseptal infarction: Leads V1 and V2; proximal left anterior descending artery
- Inferior infarction: Leads II, aVF, and III; right coronary artery or left circumflex artery
Biomarker Monitoring
1. Troponin significance: Primary biomarker for MI diagnosis; document timing of elevation.
2. Collection timing: Facilitate serial measurements to track rise and fall pattern.
3. Integration with symptoms: Correlate biomarker results with clinical presentation.
4. NSTEMI vs. unstable angina: Only NSTEMI shows rising/falling troponin levels.
5. Patient education: Explain purpose of blood tests and what results indicate.
Priority Nursing Interventions
1. Immediate assessments: Vital signs, pain level, respiratory status, oxygen saturation.
2. Cardiac monitoring: Continuous ECG monitoring for arrhythmias or evolving changes.
3. Medication administration: Prompt delivery of ordered medications (oxygen, aspirin, nitrates, analgesics).
4. IV access: Establish and maintain reliable venous access.
5. Patient positioning: Semi-Fowler's position to improve breathing and reduce cardiac workload.
Patient Education & Discharge Planning
1. Symptom awareness: Teach recognition of MI symptoms, especially atypical presentations.
2. Risk factor modification: Provide specific guidance on diet, exercise, smoking cessation, and stress management.
3. Medication adherence: Explain purpose, dosage, schedule, and side effects of prescribed medications.
4. Follow-up care: Emphasize importance of cardiac rehabilitation and outpatient appointments.
5. When to seek help: Clear instructions on when to call provider vs. when to seek emergency care.
- --
Beyond the Tutorial
Nursing Process Application
1. Assessment: Focused cardiovascular assessment techniques and documentation.
2. Nursing diagnoses: Common diagnoses for MI patients including Acute Pain, Decreased Cardiac Output, Activity Intolerance.
3. Planning: Prioritizing interventions based on patient condition and presentation.
4. Implementation: Evidence-based nursing interventions for MI care.
5. Evaluation: Expected outcomes and signs of improvement vs. deterioration.
Pharmacology for Nursing Practice
1. Thrombolytics: Administration protocols, contraindications, and nursing considerations.
2. Antiplatelet agents: Mechanisms, dosing, side effects, and monitoring parameters.
3. Anticoagulants: Administration guidelines, reversal agents, and bleeding precautions.
4. Beta-blockers: Effects on heart rate and blood pressure, contraindications.
5. ACE inhibitors/ARBs: Monitoring renal function and potassium levels.
Complications & Nursing Surveillance
1. Arrhythmias: Recognition and response to common post-MI dysrhythmias.
2. Heart failure: Assessment for pulmonary edema and decreased cardiac output.
3. Cardiogenic shock: Early recognition and emergency interventions.
4. Mechanical complications: Signs of papillary muscle rupture, ventricular septal defect, or free wall rupture.
5. Psychosocial complications: Anxiety, depression, and fear after MI.
Cardiac Rehabilitation Nursing
1. Phase I (inpatient): Early mobilization protocols and activity progression.
2. Phase II (outpatient): Monitored exercise and continuing education.
3. Exercise prescription: Guidelines for safe activity resumption.
4. Return to activities: Evidence-based guidance for driving, work, and sexual activity.
5. Lifestyle modification support: Strategies for successful behavior change.
Special Population Considerations
1. Elderly patients: Modified presentation, comorbidity management, and medication adjustments.
2. Women: Recognition of unique symptom patterns and higher mortality risk.
3. Diabetic patients: Higher risk for silent MI and complications.
4. Post-surgical patients: Recognition of perioperative MI.
5. Culturally sensitive care: Addressing health disparities and tailoring interventions across diverse populations.
