NCLEX - Malabsorption Syndromes
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Malabsorption Syndromes tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for NCLEX.
Below is information not explicitly contained within the tutorial but important for NCLEX.
- --
VITAL FOR NCLEX
Assessment of Malabsorption
1. Malabsorption occurs when there's failure to assimilate one or more nutrient types due to defects in digestion, absorption, or transport.
2. Causes include deficient digestive agents (pancreatic enzymes), abnormal gastrointestinal epithelium, impaired transport, short bowel, or inadequate mixing in the stomach.
3. Key assessment findings include diarrhea, steatorrhea, weight loss, weakness, anemia, and vitamin/mineral deficiencies.
4. Complications of malnutrition include musculoskeletal issues, neurologic manifestations (peripheral neuropathy due to B vitamin deficiencies), cardiac complications, night blindness (vitamin A deficiency), and edema (protein deficiency).
Exocrine Pancreatic Insufficiency (EPI)
1. Results in malabsorption of fats and fat-soluble vitamins (A, D, E, K, and B12) when >90% of pancreatic enzyme function is lost.
2. Common causes include pancreatitis (often alcohol-related in adults), cystic fibrosis (most common in children), and pancreatic duct obstruction from tumors.
3. Assessment findings: loose, bulky, oily, pale feces that often float due to oil content; pain starting in left epigastric area radiating to back in pancreatitis cases.
4. Diagnostic indicators include reduced duodenal pH and decreased fecal elastase-1 (FE-1) levels.
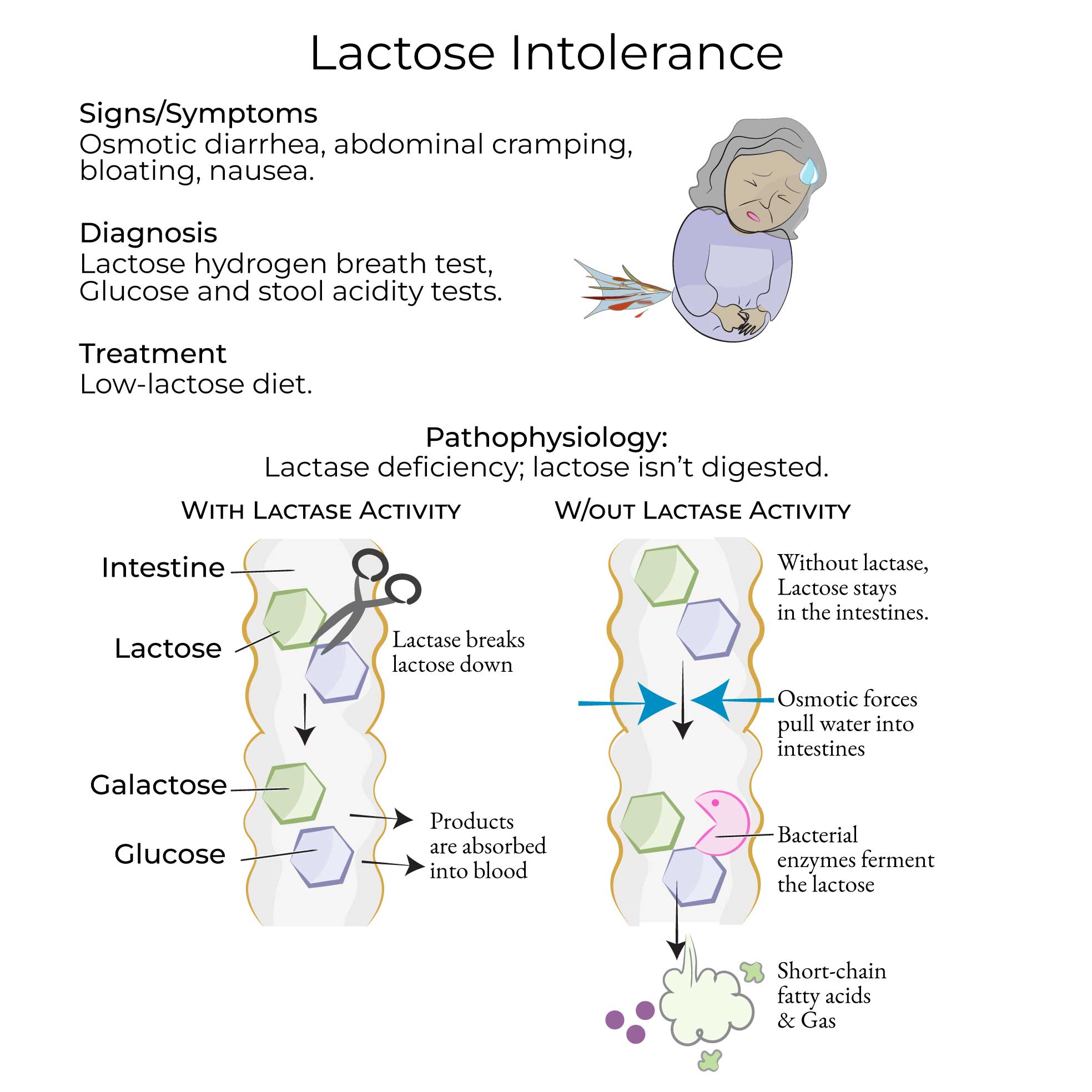
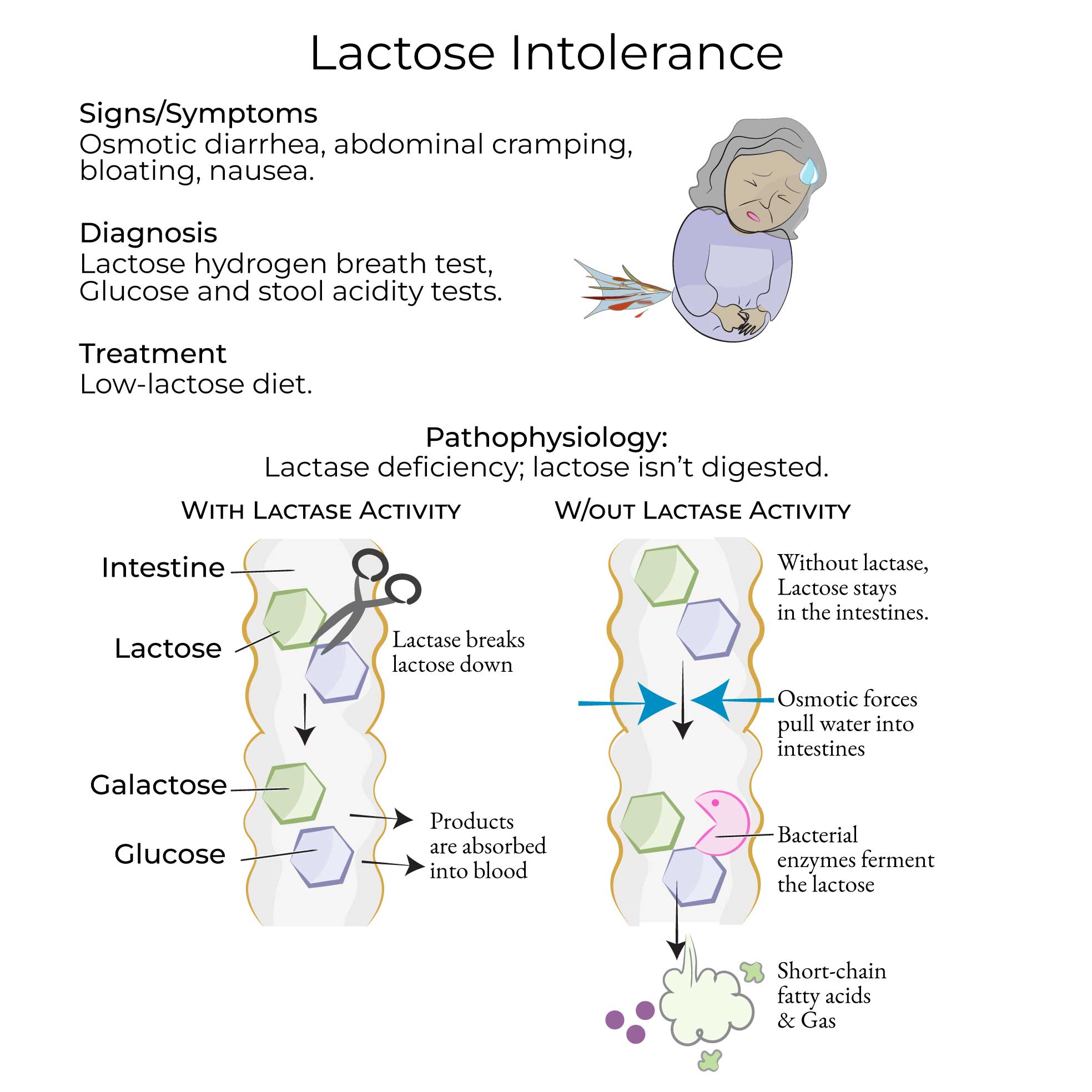
Lactose Intolerance
1. Caused by deficient lactase activity, with high global prevalence (>65%) varying by population groups.
2. Classified as congenital (rare autosomal recessive), primary (adult-type), or secondary (transient due to intestinal damage from infections or food allergies).
3. Assessment findings: abdominal pain, bloating, flatulence, and osmotic diarrhea after consuming dairy products.
4. Diagnostic tests include hydrogen breath test (>20 ppm increase indicates deficiency), blood glucose tests, DNA tests, and stool acidity tests.
Celiac Disease
1. Autoimmune inflammatory disorder of small intestine triggered by gluten (wheat, barley, rye), affecting approximately 1% of US adults.
2. Diagnostic process includes serological screening followed by endoscopy with small bowel biopsy.
3. Endoscopic findings show "scalloping" of duodenal folds and increased vascularity.
4. Associated conditions include dermatitis herpetiformis (~10% of patients), reduced bone density, and increased risk of malignancy.
Whipple Disease
1. Rare bacterial infection (Tropheryma whipplei) affecting primarily older males of European descent with immune defects.
2. Assessment findings progress from arthralgias to neurologic symptoms (dementia), endocarditis, and eventually GI symptoms (diarrhea, abdominal pain, weight loss).
3. Diagnosis requires small bowel biopsy with PAS-positive staining and PCR testing of CSF for neurologic involvement.
4. Potentially fatal without treatment and requires monitoring for relapses.
- --
HIGH YIELD
Nursing Interventions and Patient Education
1. Exocrine Pancreatic Insufficiency: Educate patients about lifestyle modifications (alcohol cessation), administration of vitamin supplements, and proper use of exogenous pancreatic enzymes with meals.
2. Lactose Intolerance: Teach patients to reduce consumption of lactose-rich foods based on individual tolerance levels and distinguish this condition from milk allergy (immune-mediated reaction to proteins).
3. Celiac Disease: Provide detailed education on strict gluten-free diet requirements, including hidden sources of gluten and cross-contamination risks.
4. Tropical Sprue: Educate patients about the importance of taking prescribed folic acid, vitamin B12 supplements, and antibiotics (tetracycline, ampicillin) as directed.
5. Whipple Disease: Stress the importance of antibiotic compliance (ceftriaxone/penicillin followed by trimethoprim/sulfamethoxazole) and follow-up to monitor for relapses.
Nutritional Considerations
1. Primary vs secondary nutritional deficiencies: Identify specific vitamin/mineral deficiencies based on presenting symptoms and laboratory values.
2. Carbohydrate and protein digestion in EPI may remain intact because amylase and protease are also secreted by salivary glands, stomach, and small intestine.
3. Monitor for signs of fat-soluble vitamin deficiencies in patients with fat malabsorption.
4. Recognize that secondary lactase deficiency may improve when underlying intestinal condition resolves.
5. Assess for complications of chronic malnutrition including bone density loss, anemia, and developmental delays in children.
Monitoring and Assessment Pearls
1. EPI: Monitor stool characteristics (oily, floating) and abdominal pain patterns.
2. Lactose Intolerance: Track symptoms in relation to dairy consumption to establish tolerance thresholds.
3. Celiac Disease: Monitor for improvement of symptoms after gluten elimination and assess for associated conditions like dermatitis herpetiformis.
4. Tropical Sprue: Evaluate response to supplementation therapy through symptom improvement and laboratory values.
5. Whipple Disease: Assess for neurologic symptoms which can be disabling if untreated; monitor for treatment response and relapse.
- --
Beyond the Tutorial
Nursing Process for Malabsorption
1. Assessment: Focused techniques for evaluating nutritional status, including anthropometric measurements, skin integrity, and functional capacity.
2. Nursing Diagnoses: Common diagnoses include imbalanced nutrition, diarrhea, deficient fluid volume, and activity intolerance.
3. Planning: Prioritization of care based on nutritional deficiencies and symptom severity.
4. Implementation: Strategies for symptom management, dietary modifications, and medication administration.
5. Evaluation: Expected outcomes and timeframes for improvement in nutritional status and symptom resolution.
Psychosocial Support
1. Addressing body image concerns related to weight loss and chronic illness.
2. Supporting patients through lifestyle and dietary changes.
3. Managing anxiety and depression related to chronic digestive disorders.
4. Promoting adherence to restrictive diets through motivational interviewing.
5. Connecting patients with appropriate community resources and support groups.
Pediatric Considerations
1. Growth and development monitoring in children with malabsorption disorders.
2. Age-appropriate nutritional interventions and feeding strategies.
3. School accommodations for children with dietary restrictions.
4. Family education to support dietary management at home.
5. Transitional care planning for adolescents with chronic malabsorption conditions.
