NCLEX - Liver Disease Overview
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Liver Pathophysiology Overview tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for NCLEX.
Below is information not explicitly contained within the tutorial but important for NCLEX.
- --
VITAL FOR NCLEX
Liver Disease Progression Assessment
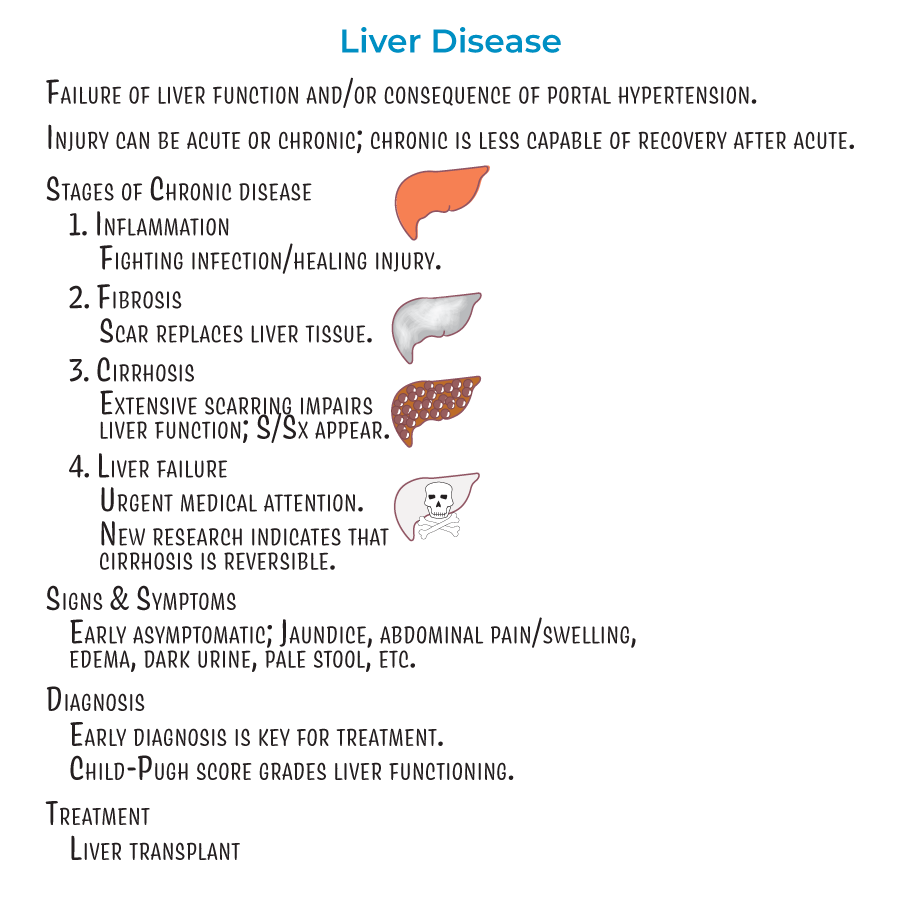
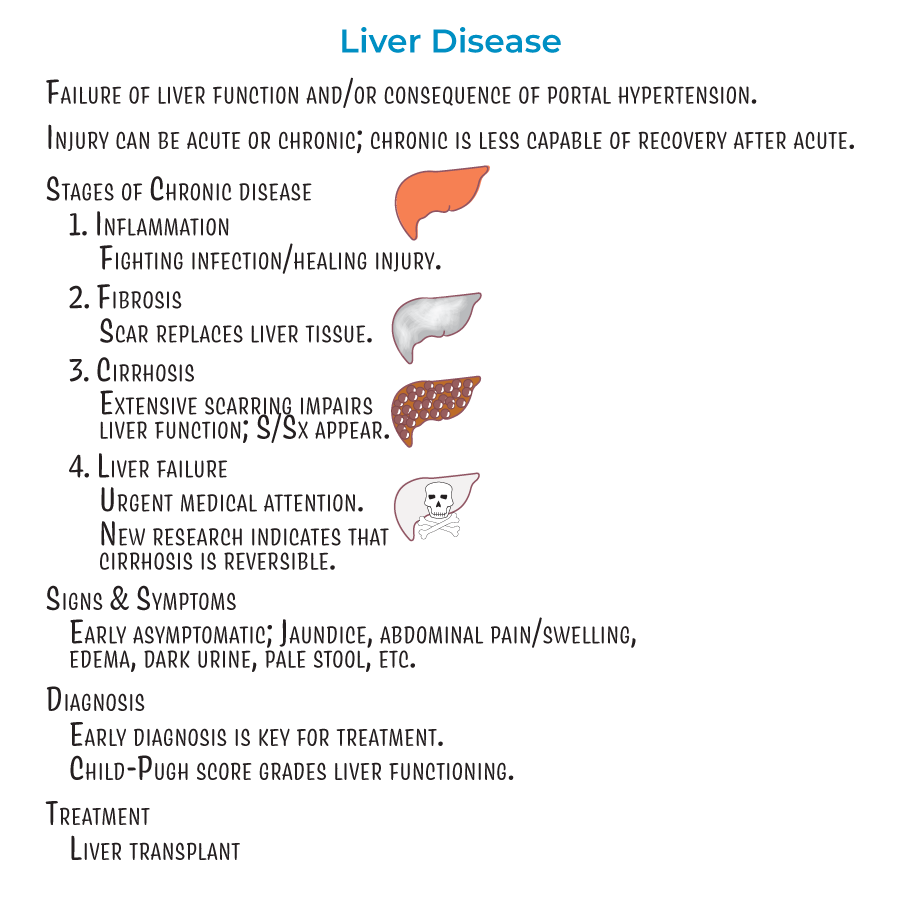
1. Four Key Stages: Liver disease progresses through inflammation, fibrosis, cirrhosis, and liver failure stages.
2. Early Detection: Early stages of liver disease are asymptomatic; later stages can present with jaundice, abdominal pain and swelling, edema, dark urine, pale stool, and other signs of liver dysfunction.
3. Monitoring Progression: Early diagnosis is key for proper treatment, and even reversal, of damage.
4. Recovery Potential: Newer research indicates that cirrhosis (stage 3) is also reversible, not just stages 1 and 2.
Cirrhosis Assessment Findings
1. Physical Characteristics: Cirrhosis is characterized by fibrosis and regenerative nodules with fatty changes.
2. Vascular Changes: Portal hypertension is increased hepatic blood pressure (above 6 mmHg).
3. Critical Assessment: The Child-Pugh score is used to grade liver functioning.
Neurological Assessment in Liver Disease
1. Encephalopathy Recognition: Hepatic encephalopathy is the result of toxin build-up in the blood; ammonia is thought to be a key culprit.
2. Asterixis Assessment: "Flapping hand tremor" or "liver flap" is the inability for a patient to sustain a posture due to involuntary, brief, "shock-like" movements.
3. Assessment Technique: To test for asterixis, have a patient sit with closed eyes, outstretched arms, dorsiflexed wrists, and spread fingers – if they suddenly "flap" their hands, this is asterixis.
Portal Hypertension Complications
1. Bleeding Risk: Varices are collateral blood vessels that form to provide alternative blood flow routes; pose significant risk for hemorrhage and GI bleeding.
2. Fluid Status Monitoring: Ascites refers to the accumulation of fluid in the peritoneum caused by systemic dilation that allows fluid leakage.
3. Infection Risk: Spontaneous Bacterial Peritonitis (SBP) is an acute infection resulting from bacteria and endotoxins leaking from the GI tract, can lead to septic shock if not treated promptly.
- --
HIGH YIELD
Integumentary System Assessment
1. Skin Changes: Elevated estrogen levels can cause spider angiomas (spider-looking collections of blood vessels visible beneath the skin) and palmar erythema (reddening of the palms and fingers).
2. Jaundice Monitoring: Impaired bile flow can lead to jaundice, visible in skin and sclera.
Gastrointestinal Assessment
1. Nutritional Status: Impaired bile flow can lead to malabsorption of GI contents.
2. GI Bleeding Risk: Varices pose an important risk for GI bleeding that requires monitoring.
Renal System Monitoring
1. Kidney Function: Renal insufficiency and failure are the result of local vasoconstriction and inflammatory processes that reduce filtration.
2. Infection-Related Complications: Spontaneous bacterial peritonitis is often a trigger for renal failure, inducing pro-inflammatory molecules that contribute to renal dysfunction.
Respiratory Assessment
1. Oxygenation Status: Hepatopulmonary syndrome involves pulmonary vasodilation leading to ventilation/perfusion mismatch, reduced oxygenation, and hypoxemia.
Metabolic Monitoring
1. Blood Glucose: Glucose metabolism is dynamically altered in liver damage so patients can be hyper- or hypoglycemic.
2. Coagulation Status: Coagulopathy results from decreased storage of vitamin K and synthesis of clotting factors.
- --
Beyond the Tutorial
Nursing Care Priorities
1. Fluid and Electrolyte Management: Accurate intake and output monitoring, daily weights, strict sodium restriction for ascites (2 grams/day).
2. Bleeding Precautions: Monitoring for signs of bleeding, avoiding NSAIDs, gentle oral care, fall precautions, frequent assessment of stools for occult blood.
3. Infection Prevention: Meticulous hand hygiene, aseptic technique for procedures, prompt recognition of fever and other infection signs.
4. Encephalopathy Monitoring: Regular neurological assessments, bowel regimen management, medication administration (lactulose, rifaximin).
Patient Education
1. Medication Safety: Teaching about hepatotoxic medications to avoid, importance of medication adherence.
2. Nutritional Guidance: Small, frequent, high-calorie, moderate-protein meals; sodium restriction; vitamin supplementation.
3. Skin Care: Prevention of skin breakdown with ascites, management of pruritus.
4. Self-Monitoring: Teaching patients early warning signs requiring medical attention (increased abdominal girth, mental status changes, GI bleeding).
Nursing Interventions
1. Paracentesis Care: Pre/post procedure monitoring, measuring abdominal girth, assessing for complications.
2. Varices Management: Positioning with head elevated, emergency equipment available, administering prescribed vasoactive medications.
3. Nutritional Support: Calorie counting, protein management, enteral feeding administration when indicated.
4. End-of-Life Care: Symptom management, family support, advanced care planning discussions.
Procedural Considerations
1. Medication Administration: Dosage adjustments for renal/hepatic impairment, monitoring for adverse effects.
2. Laboratory Value Interpretation: Liver function tests, coagulation profiles, ammonia levels, renal function.
3. Diagnostic Procedures: Patient preparation for endoscopy, paracentesis, TIPS procedure.
4. Pain Management: Careful titration of medications, avoiding hepatotoxic analgesics, non-pharmacological approaches.
