NCLEX - Jaundice
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Jaundice tutorial, as well as points of interest at the end of this document that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for NCLEX.
Below is information not explicitly contained within the tutorial but important for NCLEX.
- --
VITAL FOR NCLEX
Assessment & Identification
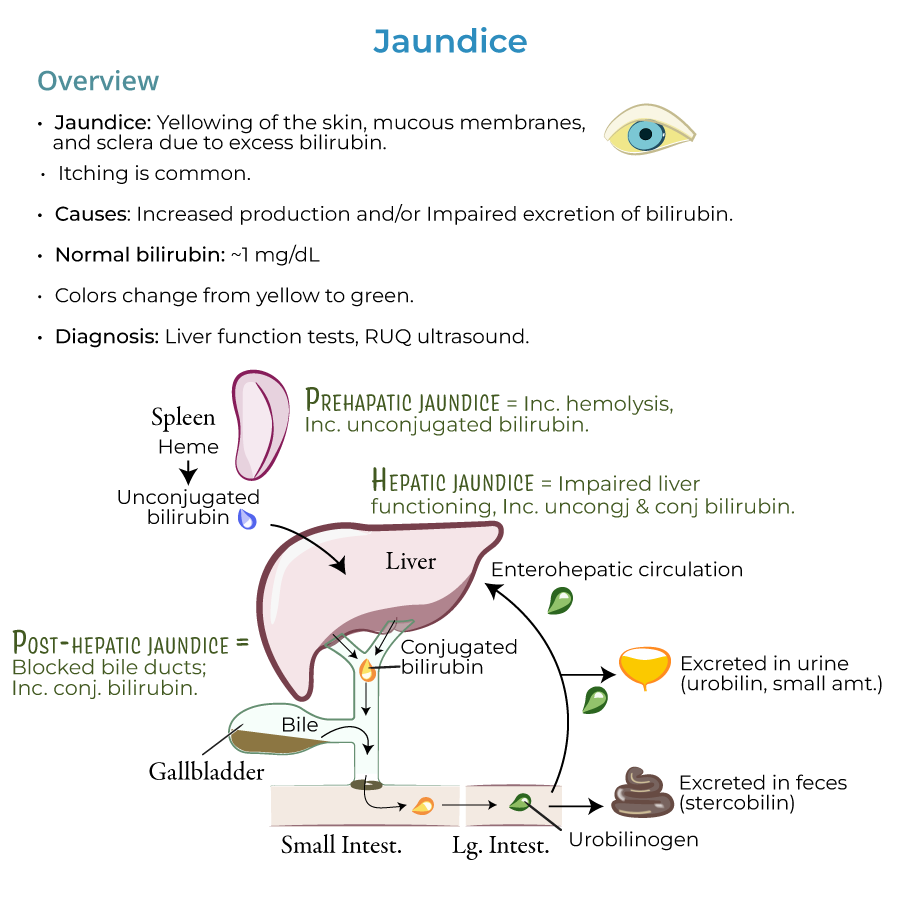
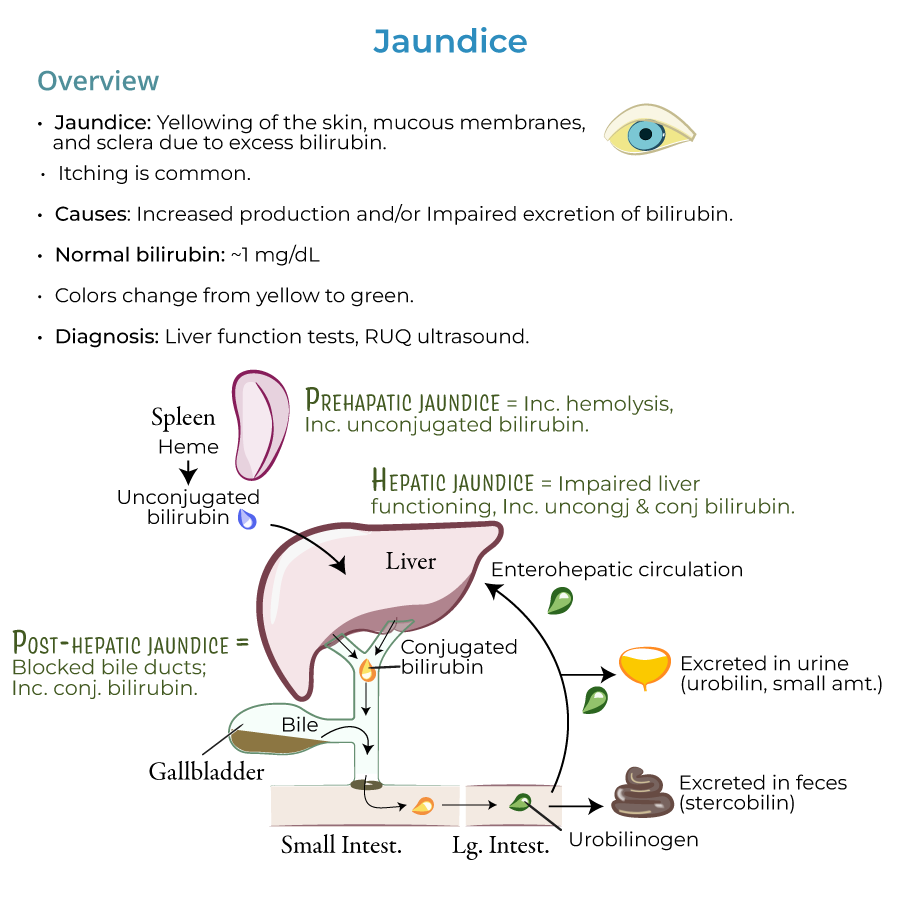
1. Clinical manifestations: Jaundice presents as yellowing of the skin, mucous membranes, and sclera due to excess bilirubin; itching is also common.
2. Normal vs. abnormal values: Normal bilirubin values are approximately 1 mg/dL; jaundice is usually present when levels are 2.5 mg/dL and higher.
3. Progressive assessment: As bilirubin accumulates, jaundice can progress from a yellowish to greenish color.
4. Differential assessment: Excess carotene can cause yellow/orange skin color, but the sclera is spared.
5. High-risk populations: Jaundice is most common in newborns and the elderly due to impaired conjugation in the liver and/or excretion.
Key Nursing Observations
1. Urine changes: Excess conjugated bilirubin is water soluble and appears in urine (dark urine).
2. Stool changes: In cholestasis, patients have pale, chalky-colored feces due to absence of stercobilin.
3. Assessment framework: HOT Liver mnemonic – Hemolysis, Obstruction, Tumors, and Liver diseases – helps categorize causes.
4. Diagnostic studies: Nurses should prepare patients for liver function tests and right upper quadrant ultrasound to discover the origins of jaundice.
5. Newborn monitoring: Must monitor and treat bilirubin excess promptly because newborns are particularly susceptible to kernicterus, brain damage caused by bilirubin deposits.
- --
HIGH YIELD
Nursing Assessment by Etiology
1. Pre-hepatic jaundice: Assess for signs of hemolysis including fatigue, pallor, and history of hemolytic disorders like sickle cell anemia or G6PD deficiency.
2. Hepatic jaundice: Monitor for mixed hyperbilirubinemia with abnormal liver function tests in conditions like viral hepatitis, alcoholic hepatitis, and drug toxicity.
3. Post-hepatic jaundice: Assess for biliary obstruction symptoms including right upper quadrant pain, dark urine, and clay-colored stools in conditions like gallstones, biliary inflammation, or pancreatic cancer.
4. Special populations: Pregnant women may develop intrahepatic cholestasis requiring specific monitoring.
5. Medication assessment: Document history of medications that can reduce hepatic bilirubin uptake like protease inhibitors and Rifampin.
Nursing Care for Neonatal Jaundice
1. Types of neonatal jaundice: Differentiate between physiologic jaundice (immature hepatic conjugation), breast milk jaundice (3-12 weeks duration), and breastfeeding jaundice (insufficient intake).
2. Critical assessment: Monitor for signs of pathologic jaundice that may indicate underlying disorders like G6PD deficiency.
3. Nutritional support: Ensure adequate intake to promote stool production and bilirubin excretion, especially in breastfeeding jaundice.
4. Family education: Teach parents about normal progress of neonatal jaundice and warning signs requiring immediate attention.
5. Complication monitoring: Watch for signs of kernicterus including lethargy, poor feeding, and abnormal muscle tone.
Monitoring & Interventions
1. Cholestasis management: Monitor for complications of bile flow blockage including pruritus, malabsorption of fat-soluble vitamins, and infection.
2. Hepatocellular disease: Assess for signs of liver dysfunction including asterixis, confusion, and bleeding in patients with viral, alcoholic, or autoimmune hepatitis.
3. Fluid balance: Monitor intake and output, weight, and abdominal girth for signs of ascites in advanced liver disease.
4. Nutritional status: Assess for malnutrition in patients with chronic liver disease or biliary obstruction affecting fat absorption.
5. Infection prevention: Implement precautions for patients with infectious causes of jaundice such as viral hepatitis or sepsis-associated jaundice.
Patient & Family Education
1. Cause-specific teaching: Provide appropriate education based on the underlying cause of jaundice (hemolytic, obstructive, or hepatocellular).
2. Medication management: Teach patients to avoid hepatotoxic medications and alcohol with any form of jaundice.
3. Nutritional guidance: Provide dietary recommendations appropriate for specific types of liver disease.
4. Symptom monitoring: Educate patients about symptoms that should prompt medical attention, such as increasing jaundice, mental status changes, or bleeding.
5. Prevention strategies: Teach preventive measures for viral hepatitis including vaccination and hygiene practices.
- --
Beyond the Tutorial
Nursing Process Application
1. Assessment: Comprehensive skin assessment using adequate lighting; inspect sclera, oral mucosa, and skin for yellow discoloration; assess darker-skinned patients for yellowing of the hard palate, sclera, and palms/soles.
2. Nursing diagnoses: Potential nursing diagnoses include impaired skin integrity related to pruritus, imbalanced nutrition related to malabsorption, risk for injury related to altered clotting factors.
3. Planning: Develop care plans addressing pruritus management, nutritional support, fall prevention, and patient education.
4. Implementation: Administer prescribed medications, maintain skin integrity, provide comfort measures for pruritus, implement bleeding precautions.
5. Evaluation: Monitor effectiveness of interventions through reassessment of jaundice, relief of symptoms, and laboratory values.
Nursing Interventions
1. Comfort measures: Lukewarm baths, emollients, pat-drying, and antihistamines as prescribed to relieve pruritus.
2. Skin care: Maintain skin integrity through gentle cleansing, moisturizing, and protection from trauma.
3. Nutritional support: Small, frequent meals; possible medium-chain triglyceride supplementation in malabsorption; monitoring for vitamin K deficiency.
4. Phototherapy nursing care: Eye protection during phototherapy, frequent repositioning, monitoring hydration status, assessing skin integrity, and temperature maintenance.
5. Safety interventions: Side rails up, assistive devices within reach, fall precautions implemented for encephalopathic patients.
Psychosocial Support
1. Body image disturbance: Support patients coping with visible jaundice and associated stigma.
2. Anxiety management: Provide information about diagnostic tests, procedures, and expected outcomes.
3. Family support: Include family in education and decision-making, especially for neonatal jaundice.
4. Coping enhancement: Help patients develop strategies for managing chronic liver conditions.
5. Referrals: Connect patients with support groups, social services, and community resources.
Priority Nursing Considerations
1. Delegation considerations: What tasks can be delegated to unlicensed assistive personnel versus requiring RN assessment.
2. Critical lab values: Recognition of dangerously elevated bilirubin levels requiring immediate intervention.
3. Prioritization of care: Identifying most urgent nursing needs in patients with jaundice.
4. Emergency response: Recognition and management of acute liver failure or cholangitis requiring rapid intervention.
5. Discharge planning: Essential teaching points for home management of resolving jaundice.
Specific Testing Interventions
1. Patient preparation: Instructions for fasting before specific diagnostic tests; explaining procedure expectations.
2. Test coordination: Proper sequence of diagnostic tests to prevent interference with results.
3. Post-procedure care: Monitoring after invasive procedures such as ERCP or liver biopsy.
4. Medication administration: Timing related to diagnostic tests; monitoring for reactions to contrast media.
5. Documentation: Accurate recording of pre- and post-procedure assessments, patient response, and education provided.
