NCLEX - Ischemic Heart Disease Symptoms and Treatments
Start your One-Week Free Trial
Already subscribed? Log in »
Here are key facts for NCLEX from the Ischemic Heart Disease Symptoms and Treatments tutorial, as well as points of interest at the end that are not directly addressed in this tutorial but should help you prepare for the boards. See the tutorial notes for further details and relevant links.
 Below is information not explicitly contained within the tutorial but important for NCLEX.
Below is information not explicitly contained within the tutorial but important for NCLEX.
- --
VITAL FOR NCLEX
Nursing Assessment of Ischemic Heart Disease
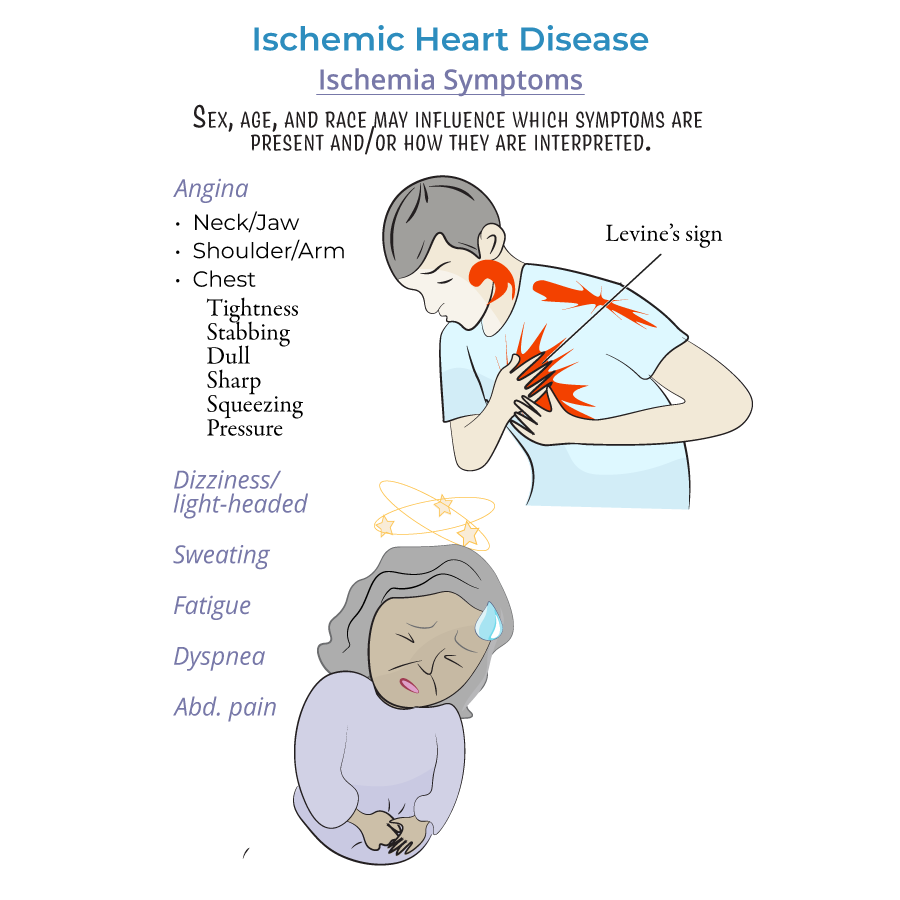
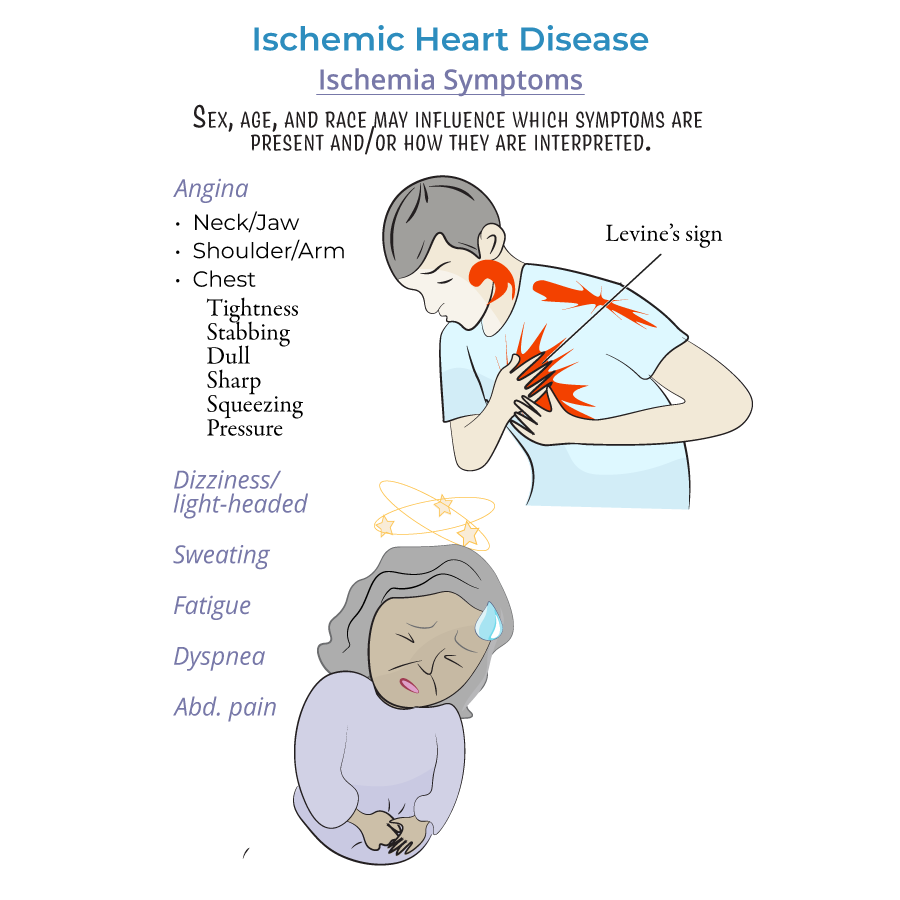
1. Angina pectoris is the hallmark symptom requiring prompt nursing assessment; characterized by chest pain/discomfort that often radiates to upper extremities, face, and other areas.
2. Stable vs. unstable angina differentiation is critical for nursing triage; stable angina is predictable and resolves with rest/nitrates while unstable angina is unpredictable and unresponsive to rest/medications.
3. Levine's sign (patient holding clenched fist over sternum) is a critical assessment finding indicating possible cardiac ischemia.
4. Non-cardiac causes of chest pain require nursing differential assessment: aortic stenosis, anemia, arrhythmias, and hypertrophic cardiomyopathy.
5. Silent ischemia requires careful monitoring as these patients may have ECG changes despite being asymptomatic.
Priority Nursing Interventions
1. Stable angina management includes administering prescribed nitrates, monitoring vital signs, and ensuring rest.
2. Unstable angina requires emergency nursing interventions: oxygen administration, IV access, 12-lead ECG, cardiac monitoring, and medication administration.
3. Vasospastic angina (occurring often at night/early morning) requires monitoring response to calcium-channel blockers and nitrates.
4. Pain assessment and management using standardized pain scales is essential for evaluating treatment effectiveness.
5. Continuous cardiac monitoring for arrhythmias, ST-segment changes, and hemodynamic instability.
- --
HIGH YIELD
Demographic-Specific Assessment
1. Sex, age, and race influence presentation; nurses must recognize that symptoms vary by demographic group.
2. Women more frequently present with light-headedness, dizziness, and persistent fatigue rather than typical chest pain.
3. Patients of African descent often report gastrointestinal discomfort that may be misinterpreted as indigestion.
4. Older adults may present with confusion, weakness, or dyspnea as primary complaints rather than chest pain.
5. Diabetic patients with neuropathy may have diminished pain perception, requiring vigilant nursing assessment.
Medication Administration & Monitoring
1. Nitroglycerin administration requires checking blood pressure before dosing; assess for headache and monitor for hypotension.
2. Beta-blockers require monitoring of heart rate and blood pressure; contraindicated in vasospastic angina.
3. Calcium channel blockers require monitoring for peripheral edema, constipation, and hypotension.
4. Antiplatelet therapy requires nursing assessment for bleeding risk and patient education on bleeding precautions.
5. Statin therapy requires monitoring for muscle pain and periodic liver function tests.
6. ACE-inhibitors require monitoring for hypotension, hyperkalemia, and assessment for cough.
7. Education on medication adherence is critical for preventing recurrent symptoms.
Post-Procedure Nursing Care
1. Post-angioplasty/PCI monitoring includes access site assessment, distal pulse checks, and cardiac monitoring.
2. Post-CABG nursing care includes respiratory assessment, mediastinal tube management, and early mobilization.
3. Cardiac rehabilitation nursing includes progressive activity planning, vital sign monitoring during exercise, and emotional support.
- --
Beyond the Tutorial
Nursing Care Planning
1. Risk for decreased cardiac output related to myocardial ischemia is a priority nursing diagnosis.
2. Activity intolerance requires careful planning with prescribed activity limitations and progressive increases.
3. Knowledge deficit regarding risk factor modification requires structured patient education interventions.
4. SBAR communication with healthcare team members is essential for continuity of care.
Patient Education Priorities
1. HEART attack recognition using the mnemonic: History, ECG changes, Age, Risk factors, and Troponin.
2. Medication schedule planning with specific instructions for PRN nitroglycerin use.
3. When to call emergency services vs. when to call healthcare provider for various symptom presentations.
4. Cardiac risk factor modification including smoking cessation, diet, and exercise counseling.
